Introduction
Nephrolithiasis affects approximately 12% of the general population. Nephrolithiasis is less common in children compared to adults; however, its incidence has been gradually increasing in recent years1,2. Pediatric urolithiasis remains an endemic problem in some countries and regions, including Turkey, Pakistan, South Asia, Africa, and North America3-5. Suggested etiologies of urolithiasis include genetics, racial factors, geographical conditions, infections, environmental factors, nutritional habits, anatomical disorders of the urinary system, and metabolic diseases6. Various studies have reported an incidence of metabolic anomalies of 40-50% in pediatric urolithiasis patients7.
Previously, the treatment of renal stones in children involved open surgical procedures. However, surgical options for urinary stones have expanded in recent years due to the development of extracorporeal shock wave lithotripsy (ESWL), ureterorenoscopy (URS), and percutaneous nephrolithotomy (PNL)8. Open or laparoscopic removal of stones is still recommended in certain cases, for instance when there are anatomical anomalies of the urinary system, such as ureteropelvic junction stenosis9.
Since the introduction of ESWL in the early 1980s, there have been significant changes in the management of urolithiasis patients, particularly in the pediatric age group10. Recent studies have reported that ESWL is an effective, safe, and reliable method for treating urinary stones in children11. Since the emergence of ESWL, important progress has been made in the non-invasive treatment of urolithiasis12. ESWL is considered the first line treatment for children with renal stones < 1.5-2 cm8,13. It has the advantages of being minimally invasive and economical, with low complication rates and short hospitalization times14.
In recent years, numerous studies have reported the use of ESWL in the treatment of pediatric urolithiasis. One study investigated the effectiveness of ESWL and factors affecting the number of sessions needed to treat children with renal stones. Age, radiolucency, and the size and number of stones were significant predictors of treatment success in children. Stone-free status was achieved sooner, sometimes after the first or second ESWL session, thereby significantly decreasing the need for a third session in children < 3 years of age with radiolucent stones, a stone size (SS) ≤ 10 mm, or a single renal stone15. However, there are few studies in the literature regarding the use of ESWL to treat urolithiasis in infants < 2 years of age. In this study, we report our ESWL results in urolithiasis patients < 2 years of age.
Materials and methods
The data of 60 patients < 2 years of age treated with ESWL for renal stones at the Pediatric Surgery and Pediatric Urology clinics of Dicle University, Faculty of Medicine between January 2012 and January 2020 were examined retrospectively.
Single stones < 2 cm in the renal pelvis and upper proximal ureter were assessed in this study. Patients with anatomical problems and multiple non-radiopaque, > 2 cm-sized stones were excluded from the study.
The patients were evaluated in terms of sex, age, stone location and burden, pre-procedural operations, and post-procedural complications. Urine, complete blood count, and biochemical tests were performed in all patients, and those with urinary tract infections were treated before ESWL was performed. As the primary diagnostic methods, ultrasonography (USG) and abdominal X-ray were performed (Fig. 1); computed tomography was also performed in some patients. A double-J (DJ) stent was placed in patients with significant hydronephrosis and pyonephrosis before the procedure. On observing significant parenchymal damage on USG, scintigraphic examinations were performed in six patients with, and five patients without, DJ stent placement. Patients with positive urine cultures were provided with appropriate antibiotherapy before the procedure to ensure sterility.
The procedure was performed with the Modularis VarioStar lithotripter (Siemens Medical Solutions Inc., Malvern, PA, USA), with the patients sedated under anesthesia using ketamine and Dormicum (midazolam), in the supine position. The stones were fragmented by shock waves, starting at a rate of 60 shocks per minute and increasing gradually thereafter. A maximum of 2000 shock waves were applied if the stone had not disintegrated. Fragmentation was evaluated by fluoroscopy after the procedure. Patients were discharged on the same day after urinary system USG had been performed, and were recalled for a follow-up USG examination 2 weeks after the procedure. When the USG revealed fragmented stones in patients undergoing catheter placement before the procedure, their DJ stents were removed, on average after 1 month. In patients with bilateral stones, the procedure was first performed on the side with the excess stone burden, and then repeated on the contralateral side. Patients without positive results typically underwent sessions, and one patient had three sessions. Surgical procedures were evaluated in patients undergoing ESWL without positive results. The demographic data of the patients are given in table 1. Patients were recalled for a follow-up USG evaluation after 3 months.
Table 1 Demographic data
| Total number of patients | 60 |
|---|---|
| Gender | |
| Boy | 32 |
| Girl | 28 |
| Side of stone | |
| Right side | 32 |
| Left side | 23 |
| Bilateral | 5 |
| Size of stone (before ESWL) | |
| Right side | 11.5 (8-18) mm |
| Left side | 12 (7-18) mm |
| Location of stone | |
| Renal pelvis | 56 |
| Proximal ureter | 9 |
| Number of ESWL sessions (per kidney) | |
| 1 session | 57 |
| 2 sessions | 7 |
| 3 sessions | 1 |
| JJ-Stent (number of patients) | |
| Unilateral | 13 |
| Bilateral | 2 |
| Results of ESWL | |
| Stone free | 47 |
| Additional surgery | 11 |
| Lost follow-up | 2 |
| Additional surgery | |
| URS lasertripsy | 5 |
| PNL | 6 |
| Post-operative complication | |
| No | 44 |
| Hematuria | 14 |
| Vomiting | 1 |
| Stone migration into ureter | 1 |
| DMSA renal scan (11 patients) | |
| Renal functional decrease | 11 |
PNL: percutaneous nephrolithotomy; ESWL: extracorporeal shock wave lithotripsy.
SPSS for Windows software (ver. 21.0; IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Continuous variables are presented as mean ± standard deviation (SD) while categorical variables are presented as number and percentage (%).
Results
In total, 60 patients (32 [53%] boys and 28 [47%] girls) were evaluated in this study. The mean age was 17 months (range: 9-24 months). The stones were located, on the right side of the renal pelvis in 32 patients (44%), in the proximal ureter in 5 patients, and on the left side of the renal pelvis in 24 patients (33%), in the proximal ureter in 4 patients. Five patients had bilateral stones. The mean size of the stones was 11.5 mm (range: 8-18 mm) on the right side and 12 mm (range: 7-18 mm) on the left side.
A total of 74 procedures were performed on 65 kidneys. ESWL was first performed on the side with the excess stone burden in five patients with bilateral stones. One patient with bilateral stones had two sessions of ESWL on the right side; three sessions of ESWL were performed in one patient with a unilateral stone, and two sessions were performed in six patients with unilateral stones. All other patients underwent one session of ESWL.
Correlation was found neither between age and SS (p > 0.05, r = 0.160), or between age and number of ESWL sessions (p > 0.05, r = −0.049). However, a positive correlation was detected between SS and the number of ESWL sessions (p < 0.01, r = 0.320) (Fig. 2). In addition, no significant variation was observed in SS between the right and left kidneys (p > 0.05).
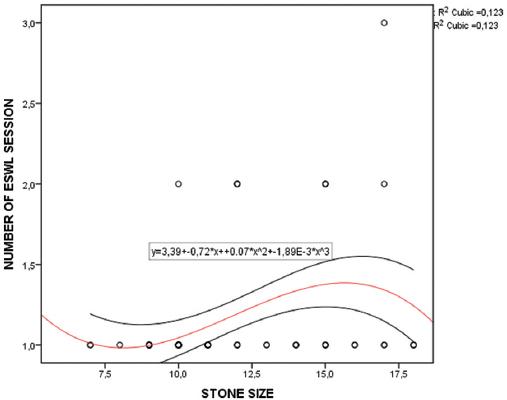
Figure 2 Correlation between stone size and number of extracorporeal shock wave lithotripsy sessions (CI 95%).
As post-procedural complications, hematuria was observed in 14 patients (12 mild and 2 significant), and vomiting occurred in 1 patient. The two patients with significant hematuria, and the patient with vomiting, were hospitalized. They were discharged after their symptoms resolved with hydration.
A binary logistic regression analysis was conducted to assess whether the risk model, with 6 predictors, varied significantly by whether patients developed hematuria. The development of hematuria was not related to age (p > 0.05), gender (p > 0.05), SS (p > 0.05, mean difference 0.27), side of stone (p > 0.05), number of ESWL sessions (p > 0.05), and location of stone (p > 0.05) (Table 2).
Table 2 Analysis of risk factors for hematuria in patients with kidney stone
| Risk factors | B | S.E. | Wald | df | Sig. | Exp(B) |
|---|---|---|---|---|---|---|
| Gender | −0.227 | 0.637 | 0.127 | 1 | 0.721 | 0.797 |
| Age | −0.049 | 0.066 | 0.544 | 1 | 0.461 | 0.952 |
| Side | −0.533 | 0.659 | 0.655 | 1 | 0.418 | 0.587 |
| Stone size | 0.022 | 0.121 | 0.034 | 1 | 0.853 | 1.023 |
| Number of ESWL | −0.95 | 1.098 | 0.749 | 1 | 0.387 | 0.387 |
| Location | 0.345 | 0.904 | 0.145 | 1 | 0.703 | 1.411 |
| Constant | 0.537 | 2.37 | 0.051 | 1 | 0.821 | 1.711 |
ESWL: extracorporeal shock wave lithotripsy.
URS was performed in one patient due to hydronephrosis and severe pain caused by the accumulation of fragmented stones at the lower end of the ureter, and a DJ stent was placed. Before the procedure, a DJ stent was placed in 15 patients, 2 of whom underwent bilateral placement. The stent was removed in patients with fragmented stones after ESWL.
In DJ stent-placed group had a larger SS comparing the non-DJ group (p < 0.05, SS: 12.9 vs. 11.4, mean difference −1.54). A ROC analysis of SS for DJ placement detected a sensitivity of 65%, and specificity of 68% when the cutoff value is 11.5 mm (AUC: 0.66, 95% CI: 0.52-0.80).
As a result of ESWL, 47 (78%) patients were completely stone-free (< 10 mm 87%, 10-20 mm 70%) (Fig. 3). Residual stones < 4 mm were considered insignificant. URS was performed in 5 patients, and PNL in 6 patients due to a failed procedure.
Impaired renal parenchymal structure and reduced function were observed in 11 patients undergoing scintigraphic examination.
A binary logistic regression analysis was conducted to assess whether the risk model, with 5 predictors, varied significantly by whether patients developed renal scarring. We considered only SS was associated with an increased risk for renal function loss (AdjOR: 1.4, 95% CI: 1.11-1.81, p < 0.01) (Table 3).
Table 3 Analysis of risk factors for renal damage in patients with kidney stone
| Risk factors | B | SE | Wald | df | Sig. | Exp (B) |
|---|---|---|---|---|---|---|
| Stone size | 0.349 | 0.124 | 7.873 | 1 | 0.005 | 1.418 |
| Gender | 0.866 | 0.764 | 1.283 | 1 | 0.257 | 2.377 |
| Age | 0.098 | 0.089 | 1.196 | 1 | 0.274 | 1.103 |
| Side | 0.171 | 0.746 | 0.052 | 1 | 0.819 | 1.186 |
| Location | −0.512 | 1.149 | 0.199 | 1 | 0.656 | 0.599 |
| Constant | −7.397 | 2.761 | 7.176 | 1 | 0.007 | 0.001 |
ROC analysis was used to determine at which cutoff value of SS required DMSA to assess SS -related kidney damage. At the 11.5 mm cutoff value of the SS, sensitivity 85%, specificity 70%, positive predictive value 40%, negative predictive value 95%, accuracy 73%, error rate 27%, likelihood ratio 2,9, and OR:13 were measured as such (AUC: 0,82, 95% CI: 0.70-0.93) (Fig. 4).
The patients were followed up by the Department of Nephrology. During follow-up, including of the patients who underwent scintigraphic examination, no new-onset or progressive impairment was observed in parenchymal structure and function. Two patients were lost to follow-up.
Discussion
The incidence of urolithiasis is gradually increasing in childhood13,16,17 and is a growing problem in endemic regions. It is diagnosed in approximately 7% of children < 16 years of age18.
ESWL allows for the natural removal of stones by fragmenting them into smaller pieces using shock waves, which can be delivered under fluoroscopy or ultrasound guidance. Current American Urological Association and European Association of Urology guidelines suggest that ESWL is a good option for ureteral and renal stones in selected children19,20.
In the study of Tekgül et al., the success rate of ESWL was approximately 90% for renal stones < 10 mm, and approximately 80% for 10-20-mm stones. They noted that the number of sessions of ESWL needed to be increased as the SS increased19. Other studies have reported that short- and long-term stone-free status was by ESWL in 37-52% and 57-100% of cases, respectively21,22. Few studies in the literature have reported on ESWL during infancy. In the study of Turna et al., ESWL was performed for renal stones in 36 patients < 1 year of age. The stone-free rate was 80% after one session, and 84% at follow-up23. In our study, a total of 75 sessions of ESWL were performed on 65 kidneys. We recorded a mean stone-free rate of 78%, 87% for stones < 10 mm, and 70% for stones between 10 and 20 mm. In line with the literature, as the size of the stone increased, so too did the number of sessions. As binary logistic regression analysis report marked the SS as a risk factor for renal damage, stones larger than 11,5 mm have the potential to develop renal damage. Thus, we recommend revealing DMSA scanning in patients at risk for renal damage such as stones larger than 11.5 mm.
Placement of a preoperative stent into the ureter for renal stones has been recommended by some studies, to prevent the development of complications, facilitate passage of the stone, and reduce pain. However, studies have shown that stone passage is easier in children, although the diameter of the ureter is narrow compared to adults. Thus, its routine use is controversial24,25. Some studies found that the use of stents before ESWL was not necessary26,27. We did not routinely apply stents to our patients. In our study, DJ stents were placed in a total of 15 kidneys (23%) before the procedure, due to significant hydronephrosis and pyonephrosis. We report that DJ stent-placed group had a larger SS comparing the non-DJ group. In this way, DJ placement may be considered in selected patients.
Clinical application of ESWL in pediatric urolithiasis was delayed due to concerns regarding potential effects on organ development in children compared to adults28. The complication rate of ESWL is low, although renal, hepatic, and splenic hematomas have occasionally been reported. However, hypertension after ESWL has not been seen in recent long-term studies29,30. ESWL may lead to minor such as skin rash, renal colic, and hematuria in 5-30% of patients31. In addition, there have been some reports of severe acute damage to the kidneys after ESWL, such as subcapsular or peritoneal hematoma32,33. In one study, hematuria was detected in 44% of patients34. Turna et al. observed transient hematuria in 15 patients23. Aksoy et al. reported spontaneous subcapsular hematomas after ESWL in children35. Hematuria developed in 14 of our patients (23%). Two of them were hospitalized. According to our logistic regression analysis, large SS did not pose an extra risk for hematuria. Although the rate of hematuria in our study is similar to the literature, it is clear that the frequency of hematuria varies widely.
One of the most common problems after ESWL is ureteric obstruction resulting from the accumulation of fragmented stones. In the distal ureter, a condition called steinstrasse (stone street) may occur, which can lead to severe obstruction. Studies have reported abdominal colic in 6.3% of cases, and steinstrasse in 6-8.5%36-38. Hematuria was observed in 23% of patients, vomiting in one patient, and accumulation of fragmented stones in the distal ureter in one patient in our study. It is important to inform pediatric patients and their parents that fragmented stones may accumulate at the lower end of the ureter after ESWL, causing vomiting, and abdominal pain.
In our study, 18% of the patients who did not benefit from ESWL required URS lasertripsy or mini PNL to achieve stone-free status. This rate was lower than in the literature27. During long-term follow-up, no procedure-related structural or functional impairment was detected in any of the kidneys.
Conclusion
ESWL treatment is effective and has advantages such as a short hospitalization time, good reproducibility, cost-effectiveness, and a low rate of complications. Therefore, we recommend ESWL as the first line treatment for renal and proximal ureteral stones in infants < 2 years of age. However, it should be kept in mind that urinary obstruction may develop after ESWL and may require intervention.











 text new page (beta)
text new page (beta)





