Introduction
Anorectal malformations (ARMs) are one of the most frequent congenital malformations in pediatric surgery. Its estimated incidence ranges between 1 in 2000 and 1 in 5000 live newborns approximately.1
It has been described that between 49 and 93% of ARMs associate some type of congenital malformation.2 Overall, urinary tract abnormalities are the most frequent with an incidence from 28% to 50% depending on the series,3 including solitary kidney, ectopic and fused kidneys, renal dysplasia, hydronephrosis and vesicoureteral reflux.4 The risk of an associated urinary abnormality is higher in worse prognosis anorectal malformations.5 The actual incidence of end-stage renal failure in patients with ARM is unknown.6 This pathology represents an important factor in the contribution to morbidity and mortality in these patients.7
The aim of the work is to present the associated urinary anomalies and functional renal outcomes in patients with worse prognosis anorectal malformations treated in our department.
Material and methods
A retrospective review of the patients operated at our center with complex anorectal malformations was performed, including urological abnormalities and long-term renal follow-up.
All the patients studied had complex anorectal malformations. The following ARMs are included as complex types: a. Girls with cloaca, b. Boys with recto-prostatic fistula, c. Cloacal exstrophy, d. Patients with other complex combined malformations ("H" fistula, genital duplication, bladder exstrophy + anorectal malformation with rectal fistula to prostatic urethra).
All patients were screened for urological malformations by ultrasound at presentation, and imaging and renal function tests (MRI, voiding cystography, nuclear renography, urodynamic studies and renal blood profile) were performed during follow-up according to their clinical course.
Collected data included the type of urinary abnormality, classified as high or low, renal function (glomerular filtration rate and blood creatinine level), the presence of chronic kidney failure (CKD), the need for surgery to correct the urinary abnormality, the need for kidney transplantation and complications and long-term results.
As for urological abnormalities, the presence of renal dysplasia, agenesis, ectopy, duplication, stenosis of the pyeloureteral junction or lower urinary tract abnormalities (bladder structural or functional alterations, vesicoureteral reflux, obstructive megaureter, posterior urethral valves or ureterocele) were recorded.
For the statistical study, the SPSS 27 system was used to examine differences between groups.
Results
A total of 55 patients were included, 32 girls and 23 boys. Mean age at the time of corrective surgery for the anorectal malformation was 9 months (SD 2.18). The mean follow-up of the patients was 13 years (SD 7.01).
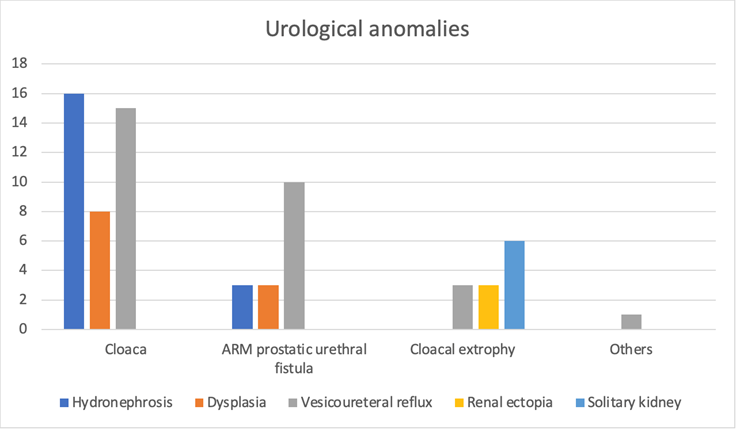
Sixty-nine per cent of the patients presented some urological anomaly, being more frequent in the cloacal group (Figure 1).
Renal structural abnormalities were found in 22 (40%) of 55 patients. They were identified in 11 (47%) cloacal patients, being the most frequent renal dysplasia (n=7; 32%), followed by position abnormalities in 3 (2 horseshoe kidneys, 1 crossed renal ectopia), a duplicated excretory system in 3 and renal agenesis in 2. In the group of patients with rectal fistula to prostatic urethra there was one horseshoe kidney. In patients with cloacal exstrophy there were three pelvic kidneys and one of them horseshoe.
Regarding the lower urinary tract anomalies, it was described in 32 (58%) patients. In the cloacal group, the incidence was 65%, being the most frequent vesicoureteral reflux (n = 14, 60%) as well as in the group of patients with a fistula to the prostatic urethra and in the group with exstrophies of the cloaca (n=3, 42%).
Regarding the rest of the lower urinary tract anomalies, the general incidence of anatomic bladder anomalies (bladder diverticulum, patent urachus) was 15%. As a pathology related to the upper urinary tract: primary obstructive megaureter 5%, ureterocele 1% and posterior urethral valves 1%.
Some of the main characteristics by groups are reflected in Figure 2.
Figure 2 Summary results by groups.
| Groups | Estructural urological anomalies | Lower urinary tract anomalies | Urological intervention | Chronic kidney disease |
|---|---|---|---|---|
| Cloaca (n=23) | 11 (47%) | 15 (65%) | 16 (69%) | 6 (26%) |
| Recto-prostatic fistula (n=22) | 7 (31%) | 12 (54%) | 12 (54%) | 3 (13%) |
| Cloacal exstrophy (n=7) | 4 (57%) | 3 (42%) | 4 (57%) | 2 (28%) |
| Complex combined malformations (n=3) | 0 | 2 (66%) | 2 (66%) | 0 |
As for patients who met criteria for VACTERL syndrome, we found 43% (n=10) of cloacae, 13% (n=3) of patients with fistula to the prostatic urethra, and 42% (n=3) of patients with cloacal exstrophy.
There were 18 patients (33%) with neurogenic bladder, of which 83% received some type of urological surgical intervention (5 endoscopic treatments for vesicoureteral reflux, 3 ureteral reimplantations, 4 enterocystoplasties, 5 continent catheterization mechanisms and 1 cervicourethral disconnection). Thanks to these procedures, intermittent catheterization, and the treatment of some of these patients with anticholinergics, the patients are now continent.
Of all patients, 61% required some type of urological surgery, being more frequent in the cloacal group. The most frequent urological surgery was endoscopic antireflux treatment, and 5 patients finally underwent ureteral reimplantation.
A total of 7 (12%) nephrectomies were performed. In the cloacal group there were 6 (27%) and in the group with fistulas to the prostatic urethra one (4%). Of the total of nephrectomized patients, 3 (43%) patients developed CKD.
Fifteen patients (27%) had a solitary kidney, either anatomically or functionally, six of which developed chronic kidney disease.
It was found that unlike nephrectomized patients, patients with renal agenesis did not develop chronic kidney disease
Of all patients, 21% had chronic kidney disease, considering glomerular filtration rate and serum creatinine values. Of the patients with chronic kidney disease, most had a G2 stage and only one patient (who had cloacal exstrophy) had a G5 stage and required kidney transplantation.
Of the patients who developed chronic kidney disease (predominantly in the cloacal group), the majority had vesicoureteral reflux followed by renal dysplasia.
Among the patients with neurogenic bladder, 47% developed chronic kidney disease, requiring a kidney transplant.
Statistically significant differences were found in relation to vesicoureteral reflux, 81% patients with chronic kidney disease presented it, compared to 46% of patients without (p=0.03) (Figure 3).
It was shown that 63% of the patients with CKD had renal dysplasia (n = 7, p = 0.001) compared to 36% of those without renal function impairment.
Likewise, of these 7 patients with CKD and renal dysplasia, 6 of them had a neurogenic bladder.
In addition, no significant differences were found regarding the presence of spinal or lumbo-sacral abnormalities and the presence of any urological structural abnormality or the development of chronic kidney disease.
The relationship between congenital kidney damage and the presence of neurogenic bladder was analyzed. As results, it was found that 58% (n=7) of the patients with dysplasia presented neurogenic bladder. Of the patients with renal dysplasia, 16% (n=1) presented neurogenic bladder, as well as 40% of the patients with renal agenesis (n=6).
Discussion
Worse prognosis anorectal malformations are a type of complex anorectal malformation with a presentation of variable characteristics in terms of anatomy and a wide spectrum of severity.8 The diagnosis of these malformations is made based on a meticulous physical examination of the newborn.
Associated anomalies are very common in these patients and include, among others, urological, and vertebral / medullary, being more frequent in the cloacal group and cloacal extrophies.9
Overall, urinary tract abnormalities are the most frequent with an incidence from 28% to 50% depending on the series.3 This wide range is due to the fact that genital anomalies as crytorchidism are included in some studies. We did not include it in our analysis. Our high rate of associated urological anomalies found is due to the selection of patients, which excluded those anorectal malformations with better prognosis (perineal, vestibular and recto-bulbar fistula).
This pathology represents an important factor in the contribution to morbidity and mortality in these patients.7 The impairment of renal function can sometimes be preventable with an early diagnosis, an adequate treatment and a long-term follow up. Most of the urological abnormalities associated with complex ARMs can be detected with a neonatal ultrasound. Duci et al.10 evaluated the efficacy of the early detection and found that the screening program can diagnose 88% of urinary disorders. Goossens et al.5 in their evaluation of urological pathology screening methods in patients with ARM, concluded that an ultrasound of the urinary tract should be performed in all patients. All this information could help to select the cases that require closer work-up to optimize long-term follow-up. Furthermore, Duci also evaluated the efficacy of clinical follow-up, and their study suggests that monitoring can find 12% of the total.10 This emphasizes the need for appropriate long-term follow-up in these patients.
Renal function depends on a variety of factors, including bladder status, intrinsic abnormalities, and other associated abnormalities.4,11 There is not much information on kidney function results in patients with anorectal malformations and studies in this regard are scarce. The actual incidence of end-stage renal failure in patients with ARM is unknown.6 In our series, 21% of the patients with complex anorectal malformations had chronic kidney disease, the most frequent cause being urinary tract infections secondary to vesicoureteral reflux. It is worth mentioning that of the patients with vesicoureteral reflux who developed chronic kidney disease, 89% had a neurogenic bladder.
These patients will require attention beyond the pediatric age and they will benefit from adequate participation in transition plans to adult care.12 It is crucial that the transition begins at an early age with regular and well-structured follow-up to reduce long-term morbidity. Urologic goals during the transition from childhood to adulthood continue to include preservation of kidney function and optimization of lower urinary tract function. Transition is intended to maximize quality of life and independence by ensuring appropriate uninterrupted care. Cooperation with a selected multidisciplinary team of pediatric and adult physicians and surgeons is required to prepare patients and families for an effective transition.13
In summary, neonatal evaluation of the upper and lower urinary tract, accompanied by prompt detection of abnormal anatomy and function of the urinary system, is essential in every patient diagnosed with a complex ARM to minimize the impact of any urological condition on their renal function and overall health. An adequate screening, with early recognition of existing urological abnormalities, is crucial to allow optimal and appropriate medical and surgical treatment, continued follow-up during childhood and a controlled transition to adulthood, reducing the morbidity of these patients. A late or failed diagnosis can have adverse consequences for the patient.
Conclusions
Patients with complex anorectal malformations have a significant risk for renal impairment. Adequate screening, high level of suspicion, treatment and long term follow up of any associated urinary anomaly in patients with complex anorectal malformations is essential to preserve renal function and prevent CKD. Care by a multidisciplinary team and adequate transition to adulthood is essential to optimize the medical management of patients and long-term outcomes.











 text new page (beta)
text new page (beta)