Introduction
When a patient consults for chest pain with anginal characteristics, a 12-lead electrocardiogram (ECG) should be performed immediately to rule out an acute coronary syndrome (ACS) with persistent ST-segment elevation that requires urgent reperfusion. We present a case of a patient who came to the emergency room for progressive angina despite treatment, with pathological ECG but without persistent ST-segment elevation.
Case presentation
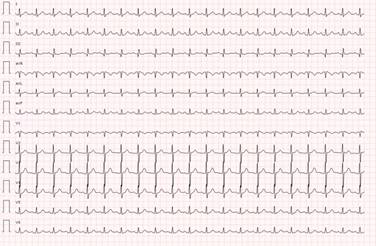
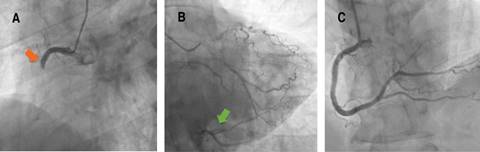
A 57-year-old man with obesity, hypertension and former smoker as cardiovascular risk factors, and previous history of Sjögren’s syndrome and gastroesophageal reflux, consulted his general practitioner for chest pain compatible with angina on moderate exertion. The ECG showed a right bundle branch block (RBBB) not present in previous ECGs (Figures 1 and 2). Treatment with ASA 100 mg od, statin and beta-blocker were started, and the patient was referred preferentially to cardiology for further evaluation. A conventional stress test was performed two weeks later. However it was stopped in the middle of the second stage of the Bruce protocol (6.8 METs and 88% of maximum heart rate) due to angina, without presenting electrocardiographic repolarization changes suggestive of ischemia. Progressive angina persisted despite treatment, so the patient consulted the emergency room four days later due to persistent chest pain at rest. The ECG did not show changes compared to the previous one, however biomarkers of myocardial necrosis were elevated (peak Tn I-hs 5140 pg/mL and CK 411 U/L), so the patient was admitted to the coronary care unit with the diagnosis of non-ST-segment elevation myocardial infarction (NSTEMI). On admission, an echocardiogram showed akinesia of the inferior basal and inferolateral basal segments with preserved parietal thickness, and normal biventricular ejection fraction, without significant valve disease or other notable findings. Antithrombotic therapy was started with ASA 100 mg, clopidogrel 300 mg, fondaparinux 2.5 mg sc, and intravenous nitroglycerin, with slight improvement, but without complete resolution of angina, so an emergent coronary angiography was decided to perform. Acute thrombotic occlusion of the right coronary artery (RCA) was observed, with collateral circulation (CC) from the left coronary tree, which did not present significant stenosis (Figure 3). Angioplasty was performed with implantation of a drug-eluting stent, with subsequent resolution of angina and disappearance of the RBBB. The patient presented a favorable clinical evolution, being discharged on the fourth day of admission.
Discussion
When a patient presents with symptoms suggestive of angina, a 12-lead resting ECG should be performed immediately to assess repolarization changes suggestive of ischemia, especially to identify early persistent ST-segment elevation, which requires emergent reperfusion.1 Characteristic ECG abnormalities in ACS without persistent ST-segment elevation include ST-segment depression, transient ST-segment elevation, and T-wave changes. Even though the ECG in this setting may be normal in more than 30% of patients,2 If the patient has signs or symptoms suggestive of ongoing myocardial ischemia and the standard leads are inconclusive, additional leads should be recorded. The left circumflex artery occlusion may be detected only in posterior leads (V7-V9) or right ventricular MI only in V3R and V4R.3 In case of persistent or recurrent symptoms or diagnostic uncertainty, it is also recommended to obtain additional 12-lead ECGs. In patients with a preexisting left bundle branch block (LBBB), specific ECG criteria (Sgarbossa’s criteria) help detect candidates for immediate coronary angiography.4 Patients with high clinical suspicion of ongoing myocardial ischemia and LBBB, regardless of whether it was previously known, should be treated similar to those with STEMI.1 In patients with RBBB, ST-elevation indicated of STEMI, while ST-segment depression in the leads I, aVL, and V5-6 is indicative of NSTE-ACS.5 Our patient did not strictly meet ECG criteria for persistent ST-segment elevation. However the patient persisted with symptoms of ongoing angina despite treatment and presented with a recent RBBB, so it was decided to perform emergent coronary angiography. Given the good heterocoronary CC observed in the infarcted territory, the infarct size was smaller than expected, as well as the poor electrocardiographic expressiveness. Therefore, it is important to always keep in mind the possibility of a MI with acute occlusion of a coronary artery in the presence of persistent angina despite adequate treatment and few repolarization abnormalities (even with a normal ECG) or new bundle branch block.











 text new page (beta)
text new page (beta)