Introduction
Enteric T-lymphoma subtype represents < 20% of lymphomas of the intestinal tract, with a low annual incidence according to epidemiological data1. Two histological subtypes have been described. Type I with refractory celiac disease that represents 80-90% of cases common in western countries. Type II is present sporadically in 10-20% of cases, not associated with celiac disease and more frequent in Asian countries according to the WHO classification1. Clinically, these patients debut with acute abdomen due to intestinal perforation in more than 50% of cases. A 60% survival rate has been reported when there is no secondary disease and < 20% at 5 years when there is metastatic involvement1. In Colombia, no cases associated with Type 2 have been reported. We describe a patient who presented an exact picture of subtype 2, infrequent in western countries and of which there are no reports in Colombia. The acute manifestation was an acute abdomen after a closed abdominal trauma where the case was oriented based on the imaging findings and the clinic presented to perform the surgical procedure.
Case description
A 53-year-old male patient was admitted to the emergency department due to a 4-day history of abdominal pain in the upper abdomen radiating to the dorsal region, pain which began after receiving blunt trauma with a soccer ball in the epigastrium. Subsequently, he developed nausea and fever and decided to consult for this reason. During the review by systems on admission, he did not report any additional pain, he denied weight loss, diaphoresis, or other constitutional symptoms and he referred that it was the 1st time he presented that clinical picture.
On initial physical examination, he was afebrile, diaphoretic, dehydrated, algic, normotensive, tachycardic, with adequate oximetry, and generalized mucocutaneous pallor. The abdomen was distended, with generalized peristaltic sounds decreased in frequency and intensity, pain on superficial, and deep palpation in the epigastric region and in the right hypochondrium, with a doubtful Murphy’s sign and no signs of peritoneal irritation.
Paraclinical tests do not show leukocytosis or neutrophilia (White blood cells [WBC]: 5700 c/mm3, N: 5.1%, Hemoglobin [HB]: 17.4 g/dL PL: 346,000 c/mm3), arterial gasses with hyperlactatemia (1.87 mmol/L), liver profile in normal ranges (Alanine aminotransferase: 21, Aspartate aminotransferase: 35, Total bilirubin: 1.16, bilirubin Indirect: 0.86, Bilirubin direct: 0.3, Alkaline phosphatase: 65). A total abdominal ultrasound was performed where a moderate amount of free perihepatic, perisplenic, and pelvic fluid was found. He was assessed by the general surgery service who indicated the taking of an abdominal CT due to the suspicion of mesenteric ischemia versus abdominal sepsis. 24 h later, the patient presented hypotension and tachycardia with new paraclinical tests with marked leukocytosis and elevation of acute phase reactants with elevation of nitrogen (WBC: 23,100 c/mm3, N: 91%, HB: 17 g/dL %, PL: 342,000 c/mm3, Polymerase chain reaction: 183 mg/L). The findings found in the tomography showed generalized ascites, diffuse edema of the mesenteric fat, without evidence of organized collections, diffuse thickening of the walls of the ascending colon, and the terminal ileum and bilateral pleural effusions, with passive atelectasis of the adjacent lung segments. Finally after exhaustive review of the intestinal loops, a continuity solution of the jejunal loop was visualized with extralumination of the intestinal content (Fig. 1).
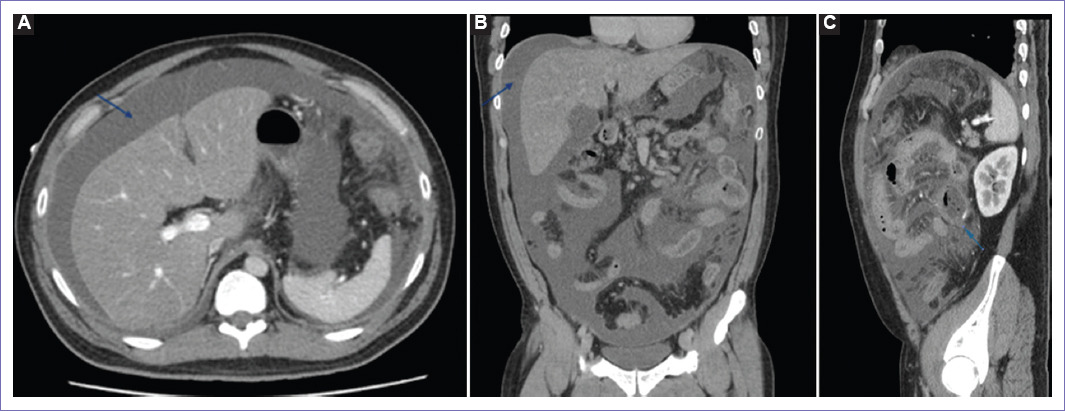
Figure 1 Contrasted abdominal tomography. A and B: Axial, Coronal section of the abdomen with contrast with abundant ascitic fluid. C: Sagittal section of the jejunal loop with loss of continuity of its wall and extralumination of its content.
Abdominal sepsis was suspected due to visceral perforation, starting antibiotic therapy and subsequently an exploratory laparotomy was performed. During the surgical procedure, ascitic fluid was found, thickening with inflammatory changes of the epiploic appendages and section of the jejunum of 90% of its circumference at 25 cm from the Treitz angle (Fig. 2). Peritoneal fluid drainage, enterotomy with side-to-side anastomosis, and proximal exeresis of the surgical piece were performed, which was carried out for pathological study, reporting non-Hodgkin’s T lymphoma.
Discussion
Primary gastrointestinal tumors of the small intestine account for about 2% of all malignancies. Primary gastrointestinal lymphoma (PGIL) is a rare neoplasm that corresponds to 1 to 4% of tumors of the gastrointestinal tract2, made up of only 5-20% of all extranodal lymphomas. The stomach, small intestine, colon, and ileocecal valve are the most affected sites of tumor involvement3-5. In the small intestine, a higher percentage of presentation in the ileum has been described in 60% of cases, followed by the jejunum in approximately 25% and finally the duodenum6.
PGIL is the most frequent extranodal manifestation of non-Hodgkin lymphoma (NHL) representing 20%7 of cases, originating histologically from the lamina propria and submucosa; its main difference from secondary lymphoid tumors, is given by its tendency to develop in multiple locations, including mesenteric nodes due to the abundant lymphoid tissue in the gastrointestinal tract. Histologically, the most frequent NHL is the diffuse type of giant B cells and the mucosa associated lymphoid tissue type8, being T and NK/T cell lymphoma the ones with the worst prognosis and the most infrequent, covering approximately 3% of NHL, being more common in Asia and less frequent in the United States and Western countries9.
In its pathogenesis, a close association has been described with Helicobacter pylori infection, HIV, celiac disease, and the epstein-barr virus (EBV). The way in which EBV enters the cell is unknown; however, it is thought that it possesses identical episomes to those present in tumor cells, indicating that it originates from a single infected cell. Histologically, extensive ischemic necrosis is observed along with “large azurophilic granules” in the cytoplasm of tumor cells, a feature that can also be found in normal natural cytolytic lymphocytes9.
On the other hand, enteric T-lymphoma subtype, which originates from the intraepithelial cells of the intestinal mucosa, representing <20% of lymphomas of the intestinal tract, should be suspected as the first diagnostic possibility. It has a reported incidence of 0.5/1 million inhabitants per year10. Its most frequent location is located at the level of the proximal jejunum and ileum. It is divided into Type I that is associated with refractory celiac disease that represent 80-90% of cases and Type II present sporadically in 10-20% of cases, not associated with celiac disease and more frequent in Asian countries according to the WHO classification10.
Histologically, Type I manifests with large multinucleated lymphoid cellularity with irregular nuclei, similar to anaplastic lymphoma, associated with an inflammatory infiltrate with the presence of histiocytes and eosinophils, which leads to necrosis with subsequent intestinal perforation, molecularly, they are positive for CD3, CD7 and CD103, being negative for CD4, CD5, and variable reactivity CD8,CD3010. Type II manifests as a proliferation of small to medium-sized lymphocytes with no associated inflammatory component and with an expressed immunophenotype of CD3, CD4, CD8, and CD5610.
Clinically, these patients debut with acute abdomen due to intestinal perforation in more than 50% of cases, this being more typical in men and less so in Type B lymphomas, abdominal pain associated with nausea or vomiting and constitutional symptoms such as weight loss and diaphoresis have also been described. A 60% of survival rate has been reported when there is no secondary disease and <20% at 5 years when there is metastatic involvement11.
For image analysis, the use of contrast-enhanced abdominal CT and barium studies is preferred; however, the findings may be non-specific. On tomography, the tumor may affect one or several segments of a small intestinal loop with significant thickening of its wall. Aneurysmal dilatation has also been described as a finding secondary to wall invasion and damage to the myenteric plexus.12 Splenomegaly, lymphadenopathies, and lymphadenopathy contiguous to the tumor site or in the retroperitoneal region have also been described, and intestinal obstruction is present in a lesser proportion. In cases of visceral perforation, free fluid can be observed in the peritoneal cavity associated with the aforementioned signs.13
Conclusion
This case represents a typical picture of this histological subtype of enteric T-lymphoma that is infrequent in Western countries and of which there are no current reports in our country. Knowing the existence of this entity has a direct impact on making a timely diagnosis and guiding decision-making in the medical field, since guided by both the clinic and the images, the best treatment for the patient can be indicated and the definitive diagnosis made by means of biopsy taking.











 text new page (beta)
text new page (beta)



