Introduction
Worldwide, there have been 763 million positive cases of SARS-CoV-2 and 6.9 million deaths. In Mexico, 7,595,635 positive cases and 333,961 deaths were reported until 2023, being predominantly males in their seventies1,2.
In Mexico, 29% of fatalities from COVID-19 were associated with the presence of comorbidities, such as systemic arterial hypertension (SAH) 51%, diabetes mellitus (DM) 40%, and obesity 18%. The prevalence of DM in patients with COVID-19 is 18%3.
Worldwide, 463 million people suffer from DM and it will increase to 578 million by the year 2030. In Mexico, 10.32% of people over 20 years of age had a diagnosis of DM, equivalent to 8,542,718 people. By the year 2020, 151,019 deaths were reported due to this disease, representing 14% of the total deaths in the country4.
DM is associated with a state of chronic inflammation, hyperglycemia, and decreased innate and humoral immunity. Likewise, in patients infected with SARS-CoV-2, increased IL-6, IL-10, sFas, granulysin, and IP-10 have been identified as biomarkers of disease progression and mortality, favoring the development of acute respiratory distress syndrome (ARDS)5.
Occurring 48 h after hospitalization among non-previously infected patients, nosocomial infection (NI) prevalence in developed countries varies between 5.1% and 11.6%, and between 5.7%-19.1% in low- and middle-income countries6-8.
NIs could complicate pulmonary viral infections such as COVID-19, playing an important role in the evolution and prognosis of patients during the pandemic, mainly when associated risk factors such as advanced age, cardiac disease, DM, and chronic kidney disease (CKD) were present. The prevalence of co-infection in COVID-19 varies between 4-22% and can exceed 45% in those patients requiring admission to the intensive care unit (ICU). The average occurrence length varies between 1 and 2 weeks on admission9.
Perhaps, concentration hospitals account for the most NIs in Mexico, having a mortality rate of 4.8%. The most common NI pathogens include Gram-negative bacteria such as Klebsiella pneumoniae, Pseudomonas aeruginosa, followed by Gram-positive bacteria such as Enterococcus faecalis, Enterococcus faecium, and Staphylococcus aureus6. A well-defined epidemiology, prevalence, etiology, antimicrobial resistance, and associated risk factors are paramount for NI control programs to be effective10.
This study aims at knowing the impact that NI had on patients admitted for COVID-19 and DM in a respiratory care unit in Mexico City.
Materials and methods
Observational, cross-sectional, and retrospective study including patients older than 18 years, having SARS-CoV-2 confirmed by PCR-RT, hospitalized in a tertiary care hospital respiratory care unit from April 2020 to December 2021. NI was defined as the presence of any of the following criteria: fever after 72 h of admission, new pulmonary infiltrate, not present at the time of admission, abnormal urine test in patients with normal urine tests at admission, bloodstream catheter-related infection during hospitalization or laboratory analysis suggestive of infection not present at admission.
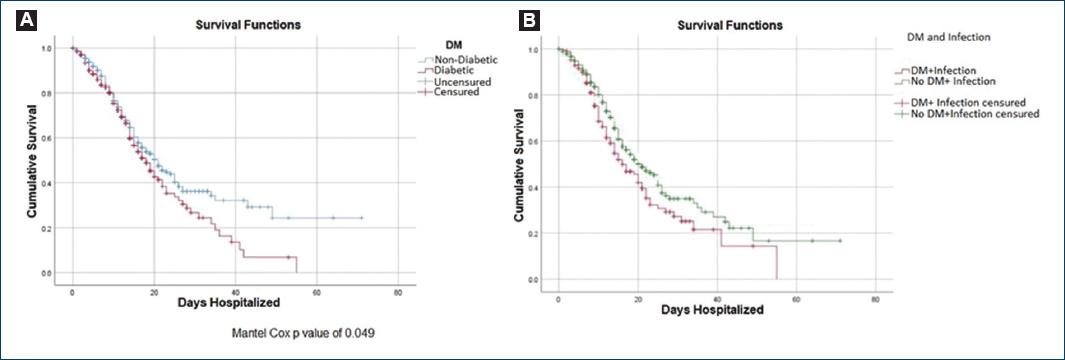
Statistical analysis was performed using the Student’s t-test for independent samples to analyze the bivariate association between variables and DM status. Chi-square test was used to analyze the bivariate association between variables and having or not DM. Kaplan-Meier graphs were used to show the survival function according to having or not DM and having or not NI. The statistical software SPSS® version 29 was used.
Results
Nine hundred and thirty records of patients hospitalized for COVID-19 were analyzed, 275 patients had Type 2 DM. The average age was 54.0 ± 15.4 years. Regarding DM status, after performing a Student’s t-test, statistically significant differences were observed in age, 58.6 ± 12.2 years in diabetic versus 52.0 ± 16.2 years in non-diabetic patients. Among patients having DM, 50.2% had SAH while only 17.9% had SAH in non-diabetic patients. Patients with CKD represented 13.1% of DM patients and 8.1% of non-diabetic patients. Mortality was higher in DM patients representing 42.9%, compared to 33.5% in non-diabetic patients. All differences were statistically significant with a p < 0.05 (Table 1). The most frequent site of culture with growth was urine culture, followed by bronchial secretion culture and blood culture, with no difference between patients with diabetes mellitus and those without diabetes mellitus (Table 2).
Table 1 Sociodemographic and clinical characteristics of people with COVID-19, according to Type 2 diabetes mellitus status
| Variable | Total (n = 930) | Non-diabetic (n = 655) | Diabetic (n = 275) | p-value |
|---|---|---|---|---|
| Age, y, mean (SD) | 54.0 (15.4) | 52.0 (16.2) | 58.6 (12.2) | 0.001a |
| Hospital LOS, mean (SD) | 11.8 (9.0) | 11.8 (9.2) | 11.9 (8.5) | 0.778a |
| SpO2, mean (SD) | 86.4 (14.0) | 86.7 (14.0) | 85.8 (13.9) | 0.409a |
| CRP, mean (SD) | 155.7 (124.4) | 151.5 (124.7) | 165.3 (123.7) | 0.233a |
| Ferritin, mean (SD) | 1339.5 (1224.3) | 1362.2 (1259.9) | 1285.3 (1135.9) | 0.442a |
| D dimer, mean (SD) | 4254.6 (8579.8) | 4076.4 (8404.8) | 4667.1 (8976.3) | 0.375a |
| Procalcitonin, mean (SD) | 1.2 (4.8) | 1.1 (4.2) | 1.5 (6.0) | 0.234a |
| Gender, n (%) | ||||
| Female | 399 (42.9) | 274 (41.8) | 125 (45.5) | 0.308b |
| Male | 531 (57.1) | 381 (58.2) | 150 (54.5) | |
| Comorbidities | ||||
| SAH, n (%) | 255 (27.4) | 117 (17.9) | 138 (50.2) | 0.001b |
| CKD, n (%) | 89 (9.6) | 53 (8.1) | 36 (13.1) | 0.018b |
| Cancer, n (%) | 37 (4.0) | 34 (5.2) | 3 (1.1) | 0.003c |
| Cardiac disease, n (%) | 25 (2.7) | 17 (2.6) | 8 (2.9) | 0.025b |
| COPD, n (%) | 12 (1.3) | 10 (1.5) | 2 (0.7) | 0.526c |
| OSA, n (%) | 2 (0.2) | 0 (0.0) | 2 (0.7) | 0.086c |
| Deaths, total, n (%) | 334 (36.3) | 217 (33.5) | 117 (42.9) | 0.007b |
| Deaths plus superinfection, n (%) | 164 (17.6) | 114 (17.4) | 50 (18.2) | 0.081b |
| Deaths w/o superinfection, n (%) | 766 (82.4) | 541 (82.6) | 225 (81.8) | 0.081b |
| Causative agents | ||||
| E. coli, n (%) | 38 (23.2) | 27 (23.7) | 11 (22.0) | 0.223c |
| Staphylococcus spp., n (%) | 40 (24.4) | 29 (25.4) | 11 (22.0) | |
| Enterobacterias, n (%) | 28 (17.1) | 22 (19.3) | 6 (12.0) | |
| Candida spp., n (%) | 23 (14.0) | 15 (13.2) | 8 (16.0) | |
| Klebsiella spp., n (%) | 15 (9.1) | 10 (8.8) | 5 (10.0) | |
| Pseudomonas, n (%) | 1 (0.6) | 1 (0.9) | 0 (0.0) | |
| Acinetobacter, n (%) | 6 (3.7) | 1 (0.9) | 5 (10.0) | |
| Other, n (%) | 13 (7.9) | 9 (7.9) | 4 (8.0) | |
| Antibiotic resistance | ||||
| Carbapenems, n (%) | 13 (18.1) | 6 (12.8) | 7 (28.0) | 0.110b |
| No carbapenems, n (%) | 133 (81.1) | 95 (83.3) | 38 (76.0) | 0.269b |
| Lincosamides, n (%) | 3 (4.8) | 1 (2.1) | 2 (12.5) | 0.156c |
SD: standard deviation; LOS: length of stay; SpO2: oxygen saturation; CRP: C reactive protein; SAH: systemic arterial hypertension; CKD: Chronic kidney disease; COPD: chronic obstructive pulmonary disease; OSA: Obstructive sleep apnea/hypopnea syndrome.
aStudent t test for independent samples.
bChi-Square test.
cFisher’s exact test.
Table 2 Positive culture site in diabetic and non-diabetic patients
| Site | Total (n) (n = 930) | Non-diabetic (n) (n = 655) | Diabetic (n) (n = 275) |
|---|---|---|---|
| Blood culture | 112 (12.04%) | 75 (11.45%) | 37 (13.45%) |
| Urine culture | 226 (24.30%) | 156 (23.82%) | 70 (25.45%) |
| Bronchial secretions | 166 (17.85%) | 119 (18.17%) | 47 (17.09%) |
| Catherter tip | 16 (1.72%) | 14 (2.14%) | 2 (0.73%) |
| Wound | 6 (0.65%) | 4 (0.61%) | 2 (0.73%) |
| Sputum | 8 (0.86%) | 6 (0.92%) | 2 (0.73%) |
| Pleural fluid | 7 (0.75%) | 5 (0.76%) | 2 (0.73%) |
| Peritoneal fluid | 1 (0.11%) | 0 | 1 (0.36%) |
| Secretions | 4 (0.43%) | 2 (0.31%) | 2 (0.73%) |
| Cerebrospinal fluid | 1 (0.11%) | 1 (0.15%) | 0 |
In the Kaplan-Meier graph for survival function, we observed that survival was higher in non-diabetic patients (Fig. 1A). Similarly, the survival function was slightly higher in non-diabetic patients having superinfection (Fig. 1B).
Discussion
NIs, as a global public health problem, constitutes a permanent threat in the care of patients in respiratory care units, affecting hospital stay, and costs. In Mexico, a high prevalence of NIs is commonly observed in internal medicine, pediatrics, and surgery floors. Knowing the associated risk factors help us to prevent up to a third of NIs11.
Well-known macro-and microvascular complications of DM affect patient survival. The association between diabetes and associated infections is also well known; however, evidence is controversial regarding whether DM itself increases susceptibility to infection, or whether cardiovascular and renal comorbidities that are frequently associated with DM are the main responsible factors12.
The prevalence of DM in patients with COVID-19 in our study (29%) was higher compared to other series where only 5.9% of patients outside the ICU had DM9. Our findings are in agreement with other studies reporting that the risk of contagion of COVID-19 in DM patients is similar to the general population; nonetheless, DM patients are more prone to complications carrying higher rates of morbidity and mortality13.
No differences were observed in NIs and mortality between diabetic and non-diabetic patients (18.2% vs. 17.4%), which is similar to the 15% mortality rate found in a Dutch series and the 16% rate in a systematic review of 48 studies in 16 countries, supporting the rationale use of antibiotics on admission. About 40% of patients with DM and NIs developed ARDS. Lowering the incidence of bacterial superinfection, even in populations at risk, could be attributed to reinforcing the correct use of personal protective equipment and hand hygiene during and after patient examination14,15.
No significant differences were observed when comparing the isolated infectious agents between diabetic and non-diabetic patients; although, when comparing our results with those of a recent systematic review, large differences in isolated pathogens exist: Escherichia coli (23.2% vs. 3.1%), Staphylococcus aureus (24.4% vs. 10.4%), Klebsiella pneumoniae (15% vs. 13.5%), Pseudomona aeruginosa (0.6% vs. 17.2%), and Acinetobacter baumannii (3.7% vs. 25%)3.
Antimicrobial resistance increased during the COVID-19 pandemic, according to a meta-analysis, the prevalence of coinfection plus antimicrobial resistance was 24%. In our study, antimicrobial resistance was 18.1% for non-carbapenems, 81.1% for carbapenems, and 4.8% for lincosamides, without finding a difference between diabetic and non-diabetic patients. Antibiotic prescription is of paramount complexity among large concentrating hospitals, hence the importance of having committees that regulate its use and limit its abuse16,17.
Hospital stay is another factor favoring the onset of NIs. A prolonged hospital stay results from more than 9 days of hospitalization18. In our study, no significant differences were observed in hospital length of stay between diabetic and non-diabetic patients (p = 0.778). Diabetic patients presented more associated comorbidities such as SAH, CKD, cancer, and cardiac disease, similar to other studies where a higher prevalence of obesity and COPD was also found14.
In our cohort, 20% of patients had metabolic dyscontrol, 15% had sepsis, 10% had acute kidney injury, and 1% had pulmonary thromboembolism. The main nosocomial complications were respiratory tract infection, urinary tract infection, and central venous catheter-related infection in that order. Similar to what was published by Alnimr et al., who reported a preponderance of respiratory and bloodstream infections with a prevalence of 57.4 and 25%, respectively19.
NIs represent a threat in immunocompromised patients with invasive devices, the main ones called ventilator-associated pneumonia, urinary tract infection, and bloodstream catheter-related infection, in our study corresponding to 60%, 20%, and 10%, respectively. Its frequency and severity made it imperative to implement actions, which included detection of causative agents, hand hygiene reinforcement, limitation of insertion of invasive devices, and rational use of antibiotics, which decreased NI incidence in our unit during the COVID-19 pandemic.
Conclusions
NIs continue to be a public health problem that requires preventive action by multidisciplinary teams. DM is a risk factor for the development of severe COVID-19 bacterial superinfection, and increased hospital length of stay, favoring the appearance of ARDS and increasing mortality rates.











 text new page (beta)
text new page (beta)