Introduction
The nasal septum is a structure that provides physiological support to the nose and affects the intranasal airflow pattern1-4. A deviated nasal septum is any curvature of the septum contour and is identified on CT scans. According to various reports in the literature, this condition is found in up to half of the adult population5-13. Based on various evidence, trauma, particularly in childhood, is an important factor in the aetiology of septal deformity6-11, while non-traumatic deviation of the septum may occur due to pressure and expansion during septal growth from the ossification centres3-12.
The concha bullosa is the aeration (pneumatisation) of the vertical part of the middle turbinate8,9,11,13,14; this anatomical variation occurs in 24% to 55% of the population8-15. The mechanism and origin of this pneumatisation are not yet well defined8,9,11,13,14, although most authors suggest that it originates from the anterior ethmoidal sinus12-15. Two theories have been proposed: one postulates that the concha bullosa arises during compensatory changes in airflow caused by deviation of the nasal septum, while the second suggests that it is due to individual anatomical variations12,13,15-17.
Unilateral concha bullosa has been associated with contralateral septal deviation and hypertrophy of the inferior turbinate and obstruction of the osteomeatal complex8,9,12-17. In most cases, the concha bullosa is considered a normal and asymptomatic anatomical variant, but it can lead to impaired ventilation or drainage when it reaches a larger size8,12-15.
The objectives of this study are: (1) to identify the frequency of CB, (2) its relationship with the deviation of the nasal septum in the population attending the General Hospital of Mexico Eduardo Liceaga (HGMEL) and, (3) to propose a radiological classification according to its size and location in relation to the degree of turbinate obstruction (HGMEL Classification).
Materials and method
An observational and descriptive study was conducted in which 142 non-contrast osteomeatal complex CT scans performed during one year (January to December 2020) were analysed. All patients had only a deviated septum without other functional nasal obstruction, such as sinusitis or allergic rhinitis. Studies in persons under 18 years of age and those with significant distortion of the sinonasal anatomy (tumours, mucormycosis, and a history of facial fracture or post-operative sinonasal surgery) were excluded. Imaging studies were obtained using a 128-channel Somatom Definition AS CT scanner (Siemens®) with axial, coronal and sagittal reconstructions at each millimetre, all within a bone window. Nasal septal deviation was defined as any curvature of the septal contour identified on CT scans, and concha bullosa was defined as aeration of the middle turbinate in case of bilateral presentation; both sides were evaluated separately. Case images were extracted from the Picture Archive and Communication System (PACS) of the HGMEL.
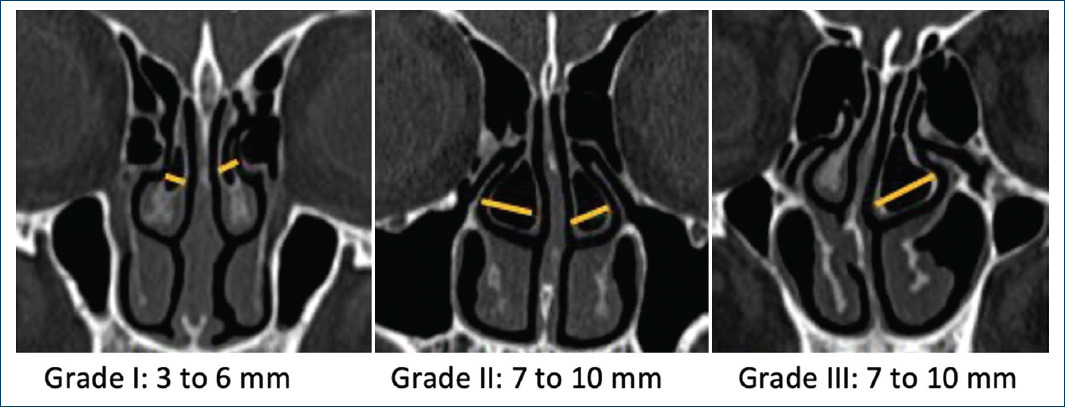
We used the Bolger classification of concha bullosa (Fig. 1)12, the Calvo-Henríquez classification by degree of pneumatisation of the middle turbinate body in the axial plane (Fig. 2)13, as well as the application of the classifications proposed by the team of the head and neck tomography department of the HGMEL Radiology Services. They are based on the size of the CB, whose extension is measured in the coronal plane from its medial to lateral edge perpendicular to its axis (Fig. 3) and based on the degrees of septal deviation in the coronal plane (Fig. 4).
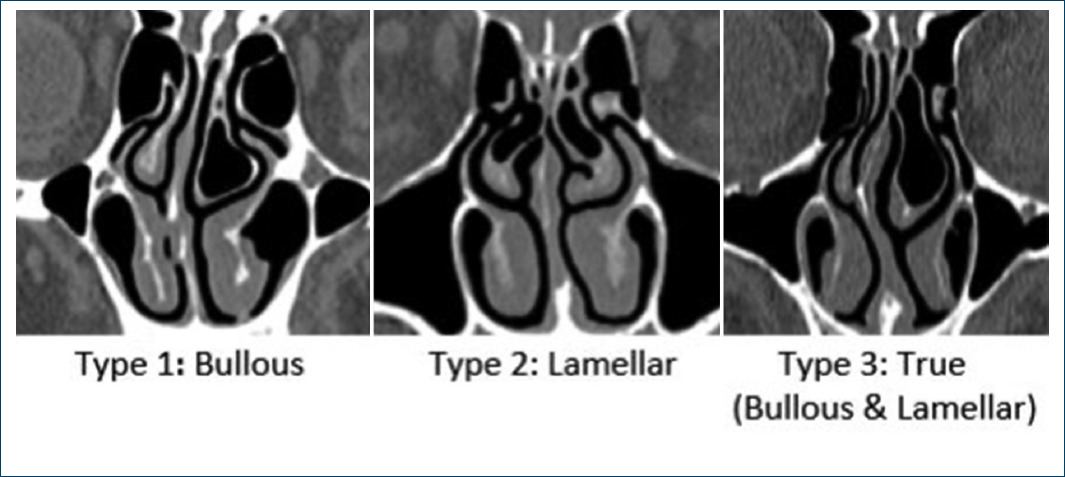
Figure 1 Coronal plane CT images showing the types of CB according to the classification by extent of pneumatisation in its different elements (Bolger).
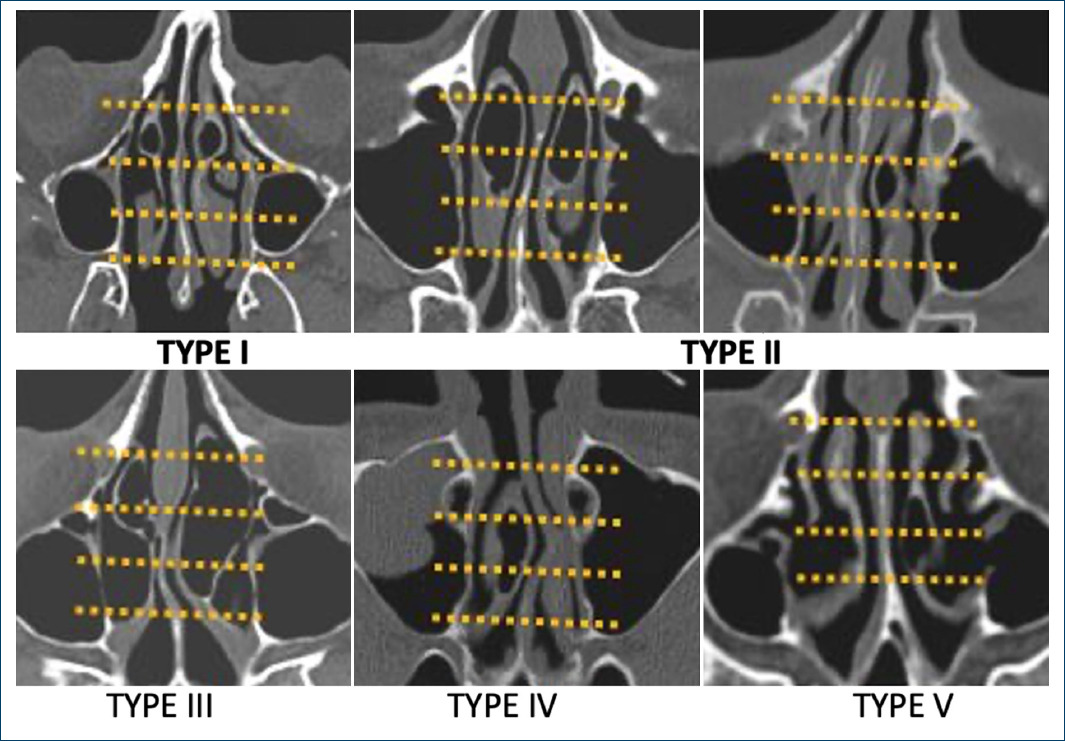
Figure 2 Axial CT scan images showing the types of CB according to the classification by extent of pneumatisation in the anteroposterior direction within the nasal cavities (Calvo-Henriquez). Type I in the anterior third of the turbinate, type II in two anterior thirds or in the middle third, type III complete anteroposterior, type IV two posterior thirds and type V in the posterior third.
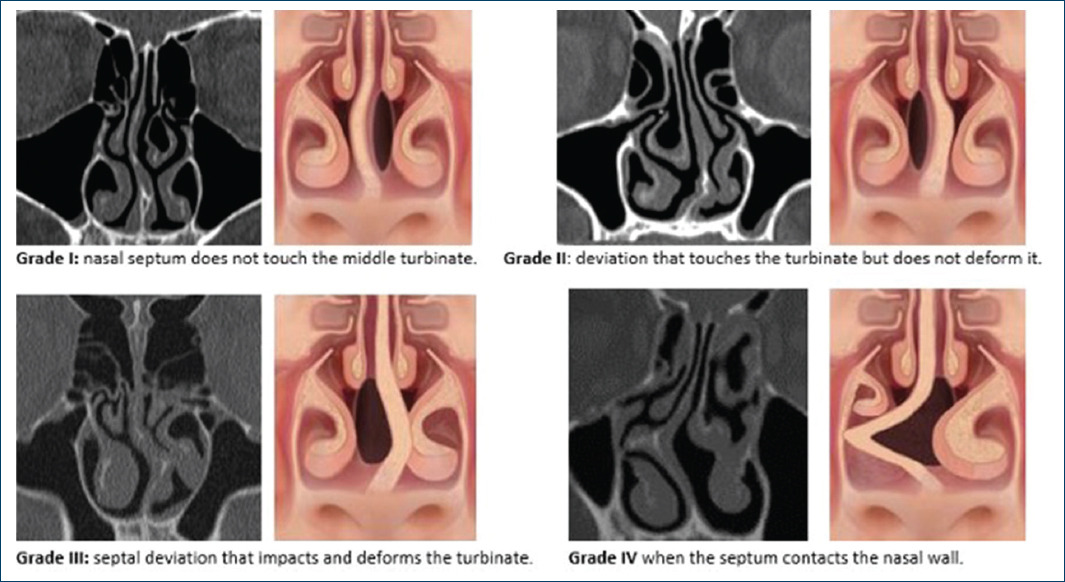
Figure 4 Coronal plane CT scan images with respective illustration showing the types of septal deviation according to the classification by degrees of obstruction over the middle turbinate (HGMEL).
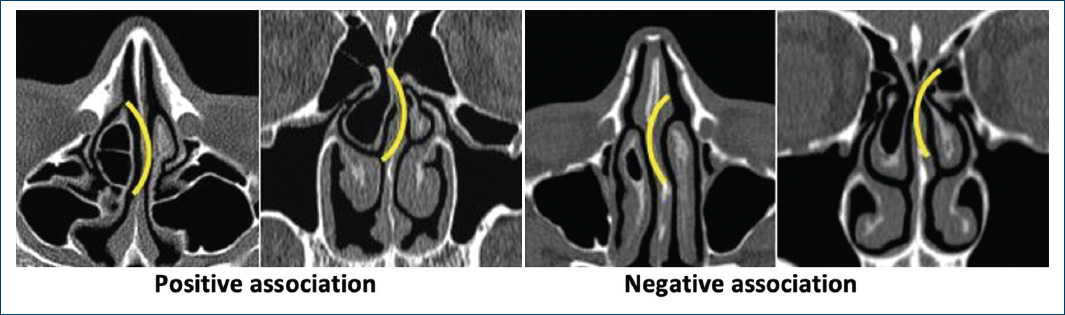
To identify the association between CB and septal deviation, we compared whether the presence of pneumatisation of the middle turbinate was on the convex or concave side of the septum in the axial and coronal planes. A positive association was determined when the CB was present on the concave side of the deviated septum and a negative association when the concha bullosa was on the convex side. In cases of bilateral pneumatisation of the middle turbinate, the largest CB was used to define its association with the septal deviation.
Results
Of the 142 sinonasal CT scans, 99 (69.72%) were excluded because they did not show CB, so the final sample size were 43 cases. Table 1 shows the general features of the cases and the location of the concha bullosa. Table 2 shows the results based on the three classifications. The most common side of the septal deviations was to the left in 58.13% of the cases and the remaining percentage corresponded to right deviations. According to the HGMEL classification, the most frequent septal deviation was type 1, followed by type 2, the least frequent being type 3. No type 4 septal deviation was observed in the present study.
Table 1 Incidence of concha bullosa by gender and location
| Right n (%) | Left n (%) | Bilateral n (%) | |
|---|---|---|---|
| Women (27) | 8 (29.63%) | 10 (37.04%) | 9 (33.33%) |
| Men (16) | 4 (25.00%) | 6 (37.50%) | 6 (37.50%) |
| TOTAL (43) | 12 (27.91%) | 16 (37.21%) | 15 (34.88%) |
Table 2 Results for concha bullosa based on different classifications
| Bolger classification | n | |
|---|---|---|
| Type 1 | 9.3 | |
| Type 2 | 25 | 58.14 |
| Type 3 | 32.56 | |
| Calvo-Henriquez classification | n | % |
| Type I | 21 | 48.84 |
| Type II | 39.53 | |
| Type III | 9.3 | |
| Type IV | 1 | 2.33 |
| Type V | 0 | - |
| HGMEL classification | n | |
| Grade 1 | 23 | 53.49 |
| Grade 2 | 32.56 | |
| Grade 3 | 13.95 |
HGMEL: Hospital General de México Eduardo Liceaga.
In this analysis, we found a positive relationship between concha bullosa media and nasal septal deviation in 74.42% (32 studies) and a negative relationship between these entities in 25.5% (11 studies). Of the cases without this association, seven had a small lamellar CB and 3 had increased hypertrophy of the contralateral middle and inferior turbinate.
Larger CB size (grade 3) was associated with a larger contact area with the nasal septum. There was a direct relationship between the size of the concha bullosa and the degree of septal deviation (Fig. 5).
Discussion
Anatomical variants of the paranasal sinuses exist in the population worldwide1-8. In Mexico, we do not have data on this, thus in this study the overall incidence of CB was determined to be 30.2% using a simple bone window scan for the paranasal sinuses, data that coincide with those reported by Soo et al8. Nasal septal deviation was more common in females (62.7%), which is consistent with Mostafa et al15.
To classify septal deviation, a morphological reference based on the position where the deviation occurs and its types (Mladina’s classification)14,18 is used, which is not practical as it does not provide data on function. This led us to propose and use our own classification (HGMEL classification) based on the degree of involvement of the middle turbinate caused by the deviation of the septum and its anatomical and physiological relevance. This is because there is a lot of information that mentions the massive importance of the air passage in the middle turbinate4,5,12-15; thus, applying this classification, we found that the most common septal deviation was type I, in which no significant obstruction is generated.
In our study, the turbinate location of the concha bullosa showed the highest incidence, suggesting that these patients present greater resistance to airflow, compared to the lamellar location, which anatomically does not restrict inhaled airflow, which coincides with the results of other authors7,9,10,12-15,19. Regarding the size of the CB, we found that the most common is grade 1 (3 mm to 6 mm). These are small and do not influence the components of nasal resistance, and only influence the deviation of the nasal septum1,13, while the large ones (grade 3, 11 mm to 14 mm) have a larger surface area in contact with the septum and cause airflow resistance.
Based on this study, we also found that the maximum point of septal deviation is directly or concavely (positively) related to the presence and location of the CB, i.e. the angle of septal deviation, since when the septum deviates, it closes or decreases in front of the CB, as if it exerts pressure on the nasal septum.
Conclusions
Based on our results, we conclude that there is a direct association: the larger the concha bullosa, the greater the septal deviation, which supports our initial approach. It is not possible to determine whether the CB was formed by compensatory changes in airflow caused by the deviated septum, or whether the deviated septum was generated by the airflow resistance caused by the CB presence.
The radiologist should identify and report the anatomical variants of the paranasal sinuses (their location and size) in preoperative imaging studies, hence providing the most useful information to the surgeons for the development of their intervention.
The proposed classification (HGMEL) of septal deviation and concha bullosa size is more practical in quantifying the degree of obstruction, as there is an association between a larger concha bullosa and a larger nasal septal deviation.











 text new page (beta)
text new page (beta)