Introduction
Autoimmune encephalitis (AD) by antibodies against N-methyl-D-aspartate receptor (NMDAR) is a rare condition and is usually associated with neoplasms that are more frequent in adults, such as ovarian teratomas, testicular cancer, thyroid tumors, lung cancer, colon cancer, breast cancer, and neuroblastomas1,2. In children, it is more frequent due to viral infections such as herpes virus, cytomegalovirus, vaccines, or hidden neoplasia3.
Approximately 20,000 cases per year of AD occur in the United States. In Mexico, we do not have data available specifically. Some studies have suggested that there is a predominance in the female sex of 67%, less frequent in young people of 0-10 years and adults older than 50 years. It is a neuropsychiatric and autoimmune picture that generally corresponds to a paraneoplastic syndrome as already mentioned4.
NMDARs are proteins that make up ion channels permeable to Ca++ and intervene in synaptic transmission and control the electrical impulses of the central nervous system (CNS), participating in functions such as judgment, perception, memory, human interaction, learning, and autonomous functions such as breathing and swallowing5,6.
There are two types of receptors: the NMDAR1 and NMDAR2 subunits, the first one binds to glycine and the second with a binding site for glutamic (Glu) acid. These are located postsynaptically7 (Fig. 1).
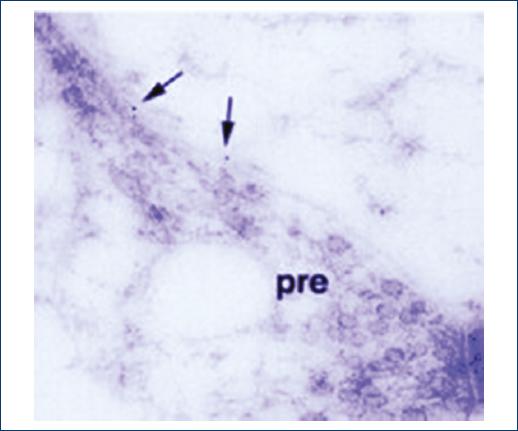
Figure 1 Microelectronic Photography showing pre- and post-synaptic border. Arrows point to dark synaptic vesicles. Imaged reproduced from Petralia, available at Openi, doi:10.1100/2012/267120.
Glu acid is the main excitatory neurotransmitter of the CNS. Glu is a non-essential amino acid that does not cross the blood–brain barrier; it is synthesized in the mitochondria of the neuron from glucose and several precursors7.
The Glu, after being synthesized, is released into the cytoplasm where it accumulates in synaptic vesicles by a process dependent on Mg++/ATP (Fig. 2). The propagation of the nerve impulse toward the axon terminal promotes the release of Glu in the synapse through a mechanism dependent on intracellular Ca++ concentration, through an exocytosis process, to interact with its specific receptors8.

Figure 2 Pre-synaptic binding and N-methyl-D-aspartate receptor. Imaged reproduced from Du et al., available at Openi.
The majority of patients with AD do not tend to present with a defined clinical picture, and the classic description is of a subacute picture (< 3 months of evolution); it is described with alterations in memory, psychiatric symptoms, and altered mental state.
Among the most frequent clinical features is the presentation of fever with psychiatric abnormalities, abnormal movements and orofacial dyskinesias; the latter occurs frequently in the pediatric patient.
The diagnostic criteria are as follows:
Subacute evolution (progression < 3 months) with symptoms of memory deficit at term, altered mental status, or psychiatric symptoms.
One of the followings: recent focal findings, unexplained seizures, and pleocytosis in the cerebrospinal fluid (leukocytosis in > 5 cells/mm3). Magnetic resonance findings suggestive of encephalitis.
Exclusion of other alternative causes.
Study of the patient
Imaging, electroencephalogram, and lumbar puncture should be performed in the presence of suspicion.
Positron emission computed tomography (CT) can show hypo or hypermetabolic changes in various areas of the brain, hyperintensities in temporal or frontal regions, and sometimes without magnetic resonance findings even with evidence of encephalitis. When the electroencephalogram is performed in patients with AD, delta activity is observed in temporal regions or generalized rhythmic delta activity with fast superimposed activity (delta brush), with an abnormal electroencephalogram found in 90% of cases.
The findings in the cerebrospinal fluid as pleocytosis show an increase in proteins and oligoclonal bands or elevated IgG index is found in 60%; this in about two-thirds of patients.
Differential diagnosis should be made with infectious etiologies such as viral or bacterial encephalitis, of toxic etiology such as neuroleptic malignant syndrome, drug ingestion (alcohol, ketamine, organophosphates). Epileptic disorders include non-convulsive status epilepticus, temporal lobe epilepsy, and refractory epileptic encephalopathy induced by fever.
Autoimmune disorders include acute disseminated encephalitis, CNS vasculitis, Sjögren’s syndrome, and systemic lupus erythematosus.
Tumor causes include CNS glioma and brain metastasis. Moreover, finally, psychiatric disorders include dementia9.
Treatment
The treatment is aimed to eliminate the antibodies based on the pathogenesis of the disease. The first line includes the administration of intravenous immunoglobulin at a dose of 1-2 mg/kg/total dose (divided in 2 days of administration), contraindicated in the presence of IgA deficiency, heart failure, renal failure, and risk of thrombosis.
Corticosteroids such as methylprednisolone at a dose of 30 mg/kg/dose in boluses for 3-5 days in children and adults 1.0 g/day. Hydrocortisone 4-8 mg/kg/day not exceeding 250 mg/day, taking into account if there is an active infectious process.
Plasmapheresis usually requires 3-5 plasma exchanges and its contraindications are hemodynamic instability, pericarditis, and sepsis.
Second-line management includes the administration of medications such as rituximab at 375 mg/m2/s once a week for 4 weeks in the absence of sepsis, azathioprine at a dose of 2-3 mg/kg/day orally, if the patient does not present active infections or chronic renal failure, and mycophenolate at a dose of 1-2 g/day contraindicated in active infections9,10.
AD is an entity that has been increasing, and in children, it is more related to infectious processes than paraneoplastic processes. The most frequent agent is herpes virus and others such as Epstein–Barr virus, Varicella–Zoster, Enterovirus, and arbovirus and Bartonella bacterial etiology such as Mycoplasma, Rickettsia, and others, at the end of the list and infrequent spirochetes; of these, encephalitis is the most important syndrome of anicteric leptospirosis and occurs in 50% of the patients who undergo it9.
The leptospires belong to the Spirochaetes genus, family Leptospiraceae. Leptospires (Fig. 3) are divided into two serogroups, those that are pathogenic to man and “Leptospira biflexa” with 60 serovars that are saprophytic and not pathogenic to man. In humans, severe leptospirosis is caused by Leptospira interrogans in specific serovars of the Copenhageni group and Icterohaemorrhagiae11.

Figure 3 Leptospira en campo obscuro. Imaged reproduced from Stackebrandt et al., available at Openi, doi:10.4056/sigs.3617113.
Worldwide, there are about 100,000 human cases per year and about 1000 deaths per year (0.1-1.0 cases per 100,000 inhabitants/year in temperate climates and 10 or more per 100,000 inhabitants/year in the tropics, although in outbreaks these figures can be increased to 100 or more cases per 100,000 inhabitants/year)12. In Mexico, the most affected states are Campeche, Yucatan, Oaxaca, Hidalgo, Sinaloa, and Veracruz with the highest number of cases in October, which are sometimes associated with climatic changes, human behavior, water contamination by animals, sewage, or from a natural disaster such as floods, inadequate hygiene conditions, recreational activities, and occupational risk.
In humans, the symptoms present a wide spectrum, from asymptomatic infections, rash, non-specific febrile symptoms, gastric problems, jaundice, conjunctivitis, muscle pain, liver damage, renal failure (Weil’s disease), meningeal symptoms, and rarely death13-15.
This causes a generalized capillary vasculitis, penetrates the man through mucous membranes, healthy, or eroded skin, and at 48 h is already found in humors and tissues. It is resistant to the activity of macrophages and polymorphonuclear cells, and at 5-7 days, the specific antibodies formed favor the opsonization of the microorganism that is no longer found in the blood and are eliminated in the urine for months. It is a generalized, systemic disease that can progress toward multiple organ failure16.
Clinical case
This is a 13-year-old female patient from Veracruz who started symptoms in October 2015 after a flood in her community and who volunteered to clean up her school.
She started symptoms 3 months later with asthenia, adynamia, nausea, photophobia, and frontal headache, so she went to the hospital in her community, without integrating a diagnosis, she prescribed antiparasitic drugs, with no clinical improvement, and 3 days later, she began with tonic seizures approximately 3 min long with loss of alertness. She is admitted to the emergency service in her locality, initiating management with DFH, deciding to transfer her to the regional hospital for the study. There, CT and lumbar puncture were performed, integrating the diagnosis of viral encephalitis, treatment was Aciclovir for 13 days, and discharge with DFH, Clonazepam, Sertraline and Olanzapine.
Four days later, she continues with hallucinations, delirium, self, and heteroagresividad. Magnetic resonance imaging was performed (the results of the studies carried out in that institution were unknown) and continued with olanzapine, clonazepam, and quetiapine for further 25 days.
Without clinical improvement, she is sent to psychiatric hospital to rule out mental disorder, maintaining the same management and adding clopixol (antipsychotic); there is discarded psychiatric illness until she is transferred to this pediatric service for the study, managed with risperidone and haloperidol. CT (Fig. 4) reports a discrete loss of cortical volume in the frontal region without further findings.
She presents the data of pseudotumor cerebri of origin for infectious, increasing the neurological deterioration of the patient.
Neuro-ophthalmology reports grade 1 macular edema and cerebrospinal fluid samples are reported negative for bacterial development. The patient is metabolically stable.
Glomerular filtering cup of 99.23%, antigenic determinations through real time for cytomegalovirus, Epstein–Barr virus, and herpes virus are reported negative, liver function tests are normal, C-reactive protein 2.03 (0-8 mg/L), as well as thyroid function. The negative lupus anticoagulant, Anti DNA of 91.84. (0-200 UI/ml) Rheumatoid factor < 20 (< 20), Procalcitonin 0.050 (< 0.05 ng/ml).
Blood count, Leukocytes 9100 (4.5-10×10e3/uL), Neutrophils 5700 (40-70%), Lymphocytes 2200 (20-30), Monocytes 1100 (6-8%), Hemoglobin 13.9 (12-16 g/dL), Hematocrit 43.2 (37-47%), Platelets 270,000 (150-450×10e3/uL).
Alpha-fetoprotein 1.65 (0-9 ng/ml), CA125 antigen of 12.60 (0-35 U/ml), carcinoembryonic antigen 0.56 (0-3 ng/ml), Beta fraction of HGC 2.509 (0-3.1 mIU/ml), Antibodies Anti Smith 5.89 (<20 U/ml) antibodies against cytoplasmic antigens SS-A (ro) 4.82 (<20 U/ml), antibodies against cytoplasmic antigens (SS-B, La) 5.57 (<20 u/ml).
Magnetic resonance imaging (Fig. 5) reports changes in vascular structures and cerebral parenchyma suggesting non-specific generalized inflammatory process and cranial hypertension is ruled out. It should be considered among the differential diagnosis inflammatory angiopathy probably autoimmune, infectious, leptomeningeal metastasis, and small vessel disease. Cerebellar tonsil descent is observed without meeting criteria for a Arnold-Chiari type malformation.
The results of the analysis of cerebrospinal fluid and urine by darkfield microscopy are positive for Leptospira and the search for antibodies by the indirect immunofluorescence technique tests positive for L. interrogans IgG 1:40 (must be negative) and IgM serovar Icterohaemorrhagiae 1:20 (must be negative) so treatment starts with crystalline sodium penicillin at a dose (200,000 IU every 6 h).
Positive results are obtained for anti-NMDA1 and NMDA2 antibodies (negative), starting with methylprednisolone 1.0 g/day for 3 days and then hydrocortisone 600 mg I.V. every 6 h (4-8 mg/kg/day, maximum dose 250 mg/day) showing little clinical improvement, so it is decided to add gammaglobulin 150 mg I.V to pass in 2 days (1-2 mg/kg/day) and a cycle of cyclophosphamide 1.5 g I.V. (500-800 mg/m2/day). 10 days later, the clinical evolution is not as expected, so it is decided to add rituximab 1000 mg I.V. in 24 h (375 mg/m2 s.) obtaining slow but progressive improvement, decreasing neurological symptoms, and 17 days after administering rituximab, she is improvement.
Subsequently, it was kept under surveillance every month by external consultation with administration of immunoglobulin with proline I.V. During the following 4 months and in a period of 6 more months, there have been no relapses or evidence of neoplasms, cognitive, motor, convulsive, learning, and sleep problems, the latter, in particular, being the most frequent in anti-NMDA encephalitis.
Discussion
In AD that is mediated by the production of IgG, two types of antibodies are produced against intracellular antigens: those that are related to neoplastic processes and surface antigens and not related to neoplasms17.
Leptospira activates an innate immune response with activation of the alternative pathway of complement. However, this mechanism is not effective against all leptospires, while L. biflexa dies in the presence of these mechanisms, the pathogenic species of Leptospira (L. interrogans) survive and are able to resist the lytic action of complement by remaining viable. It has been shown that phagocytosis of leptospira by neutrophils and macrophages is only effective if the pathogen is previously opsonized by specific IgG antibodies, and since most infections are in non-immune individuals, this is minimal or even non-existent.
Being an extracellular pathogen, the acquired immune response depends on the production of IgG and IgM that are specific for serovar (cell surface antigens TLR2 and TLR4 stimulating B and T cells), as well as having outer membrane lipoproteins (LIP32, LIP36, and LIP41) which play an important role in the pathogenicity, evasion of the immune response, and dissemination to other tissues9,18.
During the infectious process, peptidoglycans, cytokines, interleukins (IL6 and IL17A), and tumor necrosis factor (alpha) activation are produced, resulting in damage to the vascular endothelium and giving a generalized vasculitis, which influence the permeability of the blood–brain barrier, thus allowing dissemination to the CNS19,20.
Conclusions
The encephalitis by antibodies against NMDA receptors is an entity that has been identifying itself more and more for a few years. It is an autoimmune entity that can present as a syndrome of multiphasic evolution which is easier to suspect when it is associated with tumors, but when its etiology is not paraneoplastic is when it can become a challenge for identification. The clinical presentation can be insidious with very non-specific symptoms, frequently, it can be accompanied by cognitive alterations such as learning, attention, memory, language, and reasoning, and this causes it to be confused as a psychiatric patient, thus delaying its diagnosis. Auxiliary tests such as lumbar puncture, electroencephalogram, and magnetic resonance support the diagnosis.
Autoantibody tests should be used to diagnose or exclude certain autoimmune causes, and the risk of occult neoplasia should always be considered.
Perform appropriate tests to exclude relevant pathogens, but without taking into account that any pathogen could give us this entity. In this case, leptospira was an initially unexpected etiologic agent that triggered the AD syndrome. A good anamnesis was the key to the suspicion of the etiological agent. The importance of this disease lies in the high rates of lethality that can be reached, especially, when it is not identified in a timely manner. The literature indicates that 5-10% are serious and potentially lethal. However, this does not mean that Leptospirosis is rare, rather it is little known and suspected by doctors, and it has probably been misdiagnosed as a study fever, dengue fever, or even hepatitis.
Leptospirosis and encephalitis are diseases that merit being studied indepth in our patients.











 text new page (beta)
text new page (beta)




