Introduction
Coronavirus disease (COVID-19), which can cause anything from minor cold-like symptoms to serious pneumonia, can be linked to a variety of illness presentations and symptoms. Patients with COVID-19 may experience healthcare-associated infections (HAIs), such as ventilator-associated pneumonia, immunosuppressive therapy, or the indiscriminate use of antibiotics(1). Additionally, patients with COVID-19 may experience bacterial and fungal coinfections linked to pre-existing comorbidities (diabetes, lung disease, immunosuppression, among others) (2) The prognosis of mucormycosis, an uncommon but potentially lethal illness, depends on prompt diagnosis and treatment. The objective of this case report is to raise awareness of the risk of this fungal complication following COVID-19 in diabetic patients as well as the prudent use of steroids and antibiotics.
Case report
In this instance, a 52-year-old man with upper respiratory symptoms (fever, cough, chest pain, disnea, and oxygen needs) indicative with COVID-19 was referred on early 2021. By using a reverse-transcription polymerase chain reaction to directly detect SARS-CoV-2 RNA, the viral infection was identified as having occurred (RT-PCR). He was given supplemental oxygen, dexamethasone (8 mg daily for 14 days), a number of antibiotics, cough medicine, and inhaled steroids prior to being admitted to the hospital for 14 days. A history of diabetes is significant pre-existing medical condition information in his medical history.
Following COVID-19, the patient developed mucormycosis. His main complaint was right eye pain (intensity 8/10), phosphenes, diplopia, and decreased visual acuity. He sought medical attention from an ophthalmologist for these symptoms, who recommended dexamethasone eye drops with neomycin, ciprofloxacin, sodium hyaluronate, fluorometholone, dorzolamide, timolol and moxifloxcin. After a month, there was a right palpebral ptosis and the pain had gotten worse.
Necrotic crusts were discovered during an anterior rhinoscopy at the orbital floor, nasal turbinate, and septum levels. In the microscopic analysis of the nasal epithelium, a biopsy and imprinting revealed the presence of hyphae at right angles, sparsely branched, and septa with morphologi cal characteristics, compatible with Mucor spp. (Figure 1).
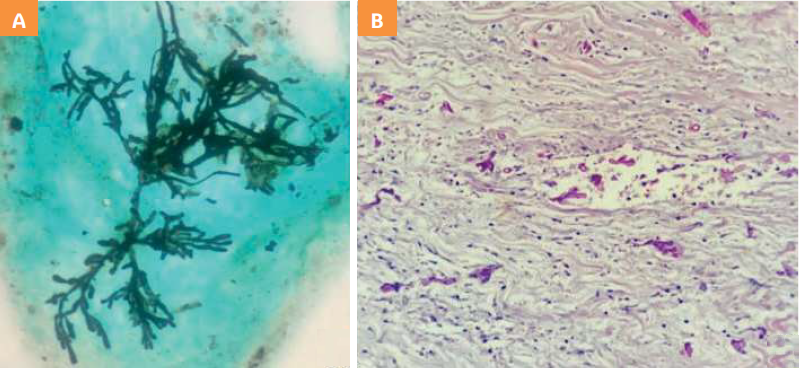
Figure 1 A: Smear, Groccott stain. The image of the septal mucous membrane shows hyphae with branches at right angles. Silver-based stains highlight the wall of pseudohyphae. B: Histological cut of mucosa of the right maxillary sinus, Hematoxylin-eosin staining. Pseudohyphae are found both in venous vessels and in the surrounding edematous stroma. In some areas, rupture of the endothelium is observed.
A 15-point Glasgow score, edema in the right centrofacial and periorbital region, ophthalmoplegia in his right eye with a mydriatic and areflexic pupil (involving the III, IV, and VI cranial nerves), ptosis, and other symptoms were all present when the patient was admitted to the hospital. Additionally, there was no corneal reflex, right ophthalmic hype- raesthesia, branches of the maxillary nerve, ecchymosis in the lower right eyelid, and nasal dorsum edema at the level of the radix ++/+++.
In light of everything said above, thrombosis of the right cavernous sinus and right cavernous syndrome, likely owing to rhino cerebral mucormycosis, was determined to be the presumptive diagnosis. Unaffected was the left eye. The nuclear magnetic resonance of the facial massif revealed mucus sequestration-suggestive soft tissue erosion in the an- terior ethmoid cells, supraorbital, posterior, and sphenoidal areas, as well as bone lysis of the septum in areas I, II, and IV, and middle and lower right turbinate (Figure 2).

Figure 2 Magnetic reso- nance imaging of the skull showing soft tissue opacification of the sinuses with extension of necrosis to the orbital zone (which causes hypointensity).
Hyperglycemia (glucose of 244 mg/dl/ concentration of 10% haemoglobin A1c) and elevated C-reactive protein (50.6 mg/L) were discovered upon admission to the hospital. After one week of treatment, the patient had hemoglobin levels of 12 g/dl (normal: 13-17 g/dl), leukocyte counts of 6.4 x 103/ ml, neutrophil counts of 4.6 x 103/ml, lymphocyte counts of 1.8 x 103/ml, hyponatremia of 130 (normal: 135-145 mE- q/L), and hypokalemia of 3.18 (normal: 3.5-5.0 mEq. Clindamycin, levofloxacin, and intravenous amphotericin were started as part of the antibiotic therapy after the histological diagnosis confirmed the presence of mucormycosis.
As the patient's health worsened, urgent surgery became necessary. A right medial maxillectomy, right ethmoidectomy, and right orbit exenteration were carried out due to all the anatomical features implicated and to stop the fungus from spreading to the endocranium.
The patient's condition improved two weeks after the surgical intervention, culminating to discharge and referral for follow-up to outpatient consultation by otolaryngology, ophthalmology, neurosurgery, psychiatry, and thanatology.
Discussion
This Mucormycosis case shows how untreated type 2 diabetes and COVID-19 are connected (a prevalent risk factor related to mortality in the Mexican population). This fungus affects people of both sexes and has no connection to profession or direct person-to-person transfer.3Mucor spp. spores can be found in soil and decomposing debris. In immunocompetent individuals, those spores can adhere to nasal mucosa and be expelled by swallowing or sneezing. Polymorphonuclear neutrophils phagocytose and eliminate the fungus when the mucous membranes are injured. However, because the innate immune response is initially the most efficient method of fungus elimination, individuals with neutropenia or neutrophil malfunction may be more susceptible to infection.4
In addition to patients with acquired immunodeficiency syndrome, iatrogenic immunosuppression, oncohematological patients, and recipients of bone marrow or organ transplants, fungi of the genus Mucor spp. can cause an opportunistic, invasive, serious, and quickly spreading infection in patients with poorly controlled diabetes. Poor diabetes management results in a continuous rise in blood glucose levels, which impairs neutrophil chemotaxis and phagocyte function. Additionally, hyperglycemia offers a perfect envi ronment for the quick formation of filamentous structures that adhere to blood arteries and infiltrate them, causing blockage, ischemia, and hemorrhage in the affected tissues or organs.5
Studies in murine models have demonstrated that diabetic ketoacidosis, in particular, causes hyperglycemia to result in GRP78 (Glucose Receptor Protein 78) overexpression, which has been linked to making it easier for Mucor to infiltrate the vascular endothelium and thereby promoting its dissemination.6 Elevated serum iron is another sign of immunosuppression-related diseases, which is a perfect substrate and growth environment for this fungal infection.7 But at the other hand, COVID-19's inflammatory phase depletes lymphocytes, while long-term high dosages of dexamethasone inhibit the immune system. (Figure 3).
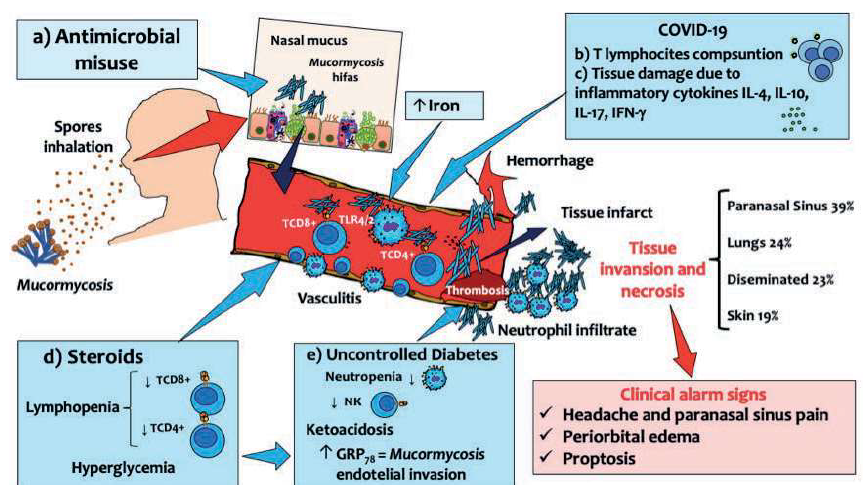
Figure's author: José Luis Gálvez Romero
Figure 3 Immunopathogenesis of mucormycosis in COVID-19. Mucormycosis is a rare infection caused by the fungus Mucor spp. This micro-organism is typically inhaled and spread through the nasal mucosa of immunocompromised people. The dissemination of Mucor spp. in the context of COVID-19, involves several mechanisms: A) unnecessary use of antimicrobial drugs, which destroy the protective microbiota of the mucous membranes, B) TCD4 and TCD8+ lymphocyte consumption per SARS-CoV-2 activity, C) direct tissue damage from a variety of inflammatory cytokines (IL-4, IL-17, IL-10 and IFN-g), D) use of long-term high doses of steroids that affect hyperglycemia and lymphopenia, e) uncontrolled diabetes resulting in the dysfunction of innate immune cells, and in the case of ketoacidosis there may be an overexpression of GRP78 (Glucose Receptor Protein 78) which contributes to the endothelial spread of Mucor spp.
Diagnosis and treatment of mucormycosis
Clinical suspicion, recognizing risk factors such uncontrolled diabetes or corticosteroid usage with symptoms and clinical manifestations, are the primary clinical criteria for the diagnosis of mucormycosis.8
In a diabetic patient or neutropenic host, diplopia, cranial nerve paralysis, sinus discomfort, proptosis, and periorbital inflammation should be suspected. Using imaging techniques and doing histological analyses since mucormycosis is characterized by tissue necrosis.9
Although culture is the gold standard, the diagnosis of mucormycosis can also be determined by seeing Mucor-like hyphae on histological examination.10 Due to their destructive character, common complications of mucormycosis which it occur from late diagnosis are associated with a high mortality and psychological stigmas.
Amphotericin B is the drug of choice for medical treatment, although debridement of the afflicted tissue is important to prevent death from the spread of this fungus. Similarly, the successful treatment of mucormycosis requires an early diagnosis and a study of risk factors. Surgical debridement before the spread of infection to other distant organs and tissues has been found to improve clinical results.11
Conclusion
This is one of the earliest documented cases of mucormycosis attributed to COVID-19 in Mexico, to our knowledge. The interdisciplinary medical team quickly recognized mucormycosis from the patient's clinical setting, which included all the risk factors and highly suggestive clinical signs. Although the patient had to endure a disfiguring treatment, quick histology confirmation and the best management prevented a worse prognosis. Psychiatric and thanatology experts collaborated to further improve the case's outcome.











 nueva página del texto (beta)
nueva página del texto (beta)



