Introduction
Primary spontaneous pneumothorax (PSP) is the accumulation of air in the pleural space without any underlying traumatic and iatrogenic etiology or an evident pulmonary disease. Tall and thin body habitus, male gender, smoking, and being aged between 19 and 25 years are frequently encountered clinical features whereas subpleural blebs and bullae appear to play a significant role in the pathogenesis of PSP at a rate as high as 80%1,2.
The recurrence rate of PSP has been reported to be ranging over 30% after the first episode3. Although there have been conclusive studies that indicate the risks of recurrence, debates mostly consist of similar variables and surgical outcomes while the deficiency of presenting novel predictive factors still exists1-4.
The lymphocyte-to-monocyte ratio (LMR) actually compels attention as a diagnostic tool for inflammatory events and a predictor of prognosis in malignancies for the concomitant advantages of easy accessibility and economical benefits.
Regarding that the pathological manifestations of PSP mostly develop in response to the inflammatory reactions produced by the parenchymal injury, this study aimed to investigate the efficacy of LMR in predicting the recurrence of PSP for the first time in the literature.
Material and methods
This study was approved by the Kırklareli Medical School Scientific Research Ethic Committee (P202200019-01/8.8.22). A retrospective study was conducted to include a total of 374 patients among 442 cases who had been diagnosed with PSP at the University Hospital between 2000 and 2021. Treatment with tube thoracostomy at the first episode and recurrent pneumothorax on the same side of the initial event were the principal inclusion criteria. Patients who had presented a secondary spontaneous pneumothorax, a history of chest surgery and any clinical or radiological suspicion of a local or a systemic infection, were excluded from the study. Regarding the well-accepted impact of smoking on the occurrence and also recurrence of PSP, the current and past history of smoking were accepted as exclusion criteria to provide a valid analysis of LMR as a potential risk factor. Follow-up period for the whole group of patients was 5 years.
In the first episode, all patients received 20 or 24 French chest tubes under local anesthesia. LMRs were calculated through whole blood counts that were obtained before interventions. The patients were invited to follow-up examinations during the 1st and 3rd weeks after being discharged or any time when they developed complaints similar to the initial admittance. The presence of recurrent pneumothorax was confirmed by chest X-ray or computed tomography. The patients with recurrence received chest tubes or underwent thoracotomy or thoracoscopy where partial parietal pleurectomy in addition to bullectomy or wedge resection was applied.
Whole group of patients was examined in terms of age, gender, side of the pneumothorax, LMR, status of recurrence, and the time until the recurrence. LMR was noted as a numerical value while the time of recurrence was stated as months.
The Statistical Package for the Social Sciences (SPSS) (IBM SPSS for Windows, Ver.24) statistical package program was used for calculations. The descriptive statistics were stated as mean, standard deviation, minimum, and maximum for continuous variables and as number and percentage for categorical variables. The calculations were checked for normal distribution by Kolmogorov–Smirnov (n > 50) test and parametric tests were applied. One-way analysis of variance (ANOVA) was performed to compare the mean values of the patient groups. Pearson correlation coefficients were used to reveal the relations between measurements. Sensitivity, specificity, and cut-off values of LMR were assessed by ROC analysis. Chi-square test was used to identify the relation between categorical variables. p < 0.05 were considered as statistically significant.
Results
The mean age of the patients including 296 (79.1%) males and 78 (20.9%) females was 22.45 ± 2.5 years. Pneumothorax was right sided in 177 (47.3%) and 197 (52.7%) cases. Mean LMR was calculated as 1.21 ± 0.31 at the first episode and 1.43 ± 0.58 at the time of relapse. Recurrent pneumothorax was diagnosed in 106 (28.3%) patients whereas the mean time between the first episode and the recurrence was 15.32 ± 5.57 months. Related data were summarized in table 1.
Table 1 Demographic and clinical features of the patients
| Parameters | Values |
|---|---|
| Age, mean ± SD (min-max), years | 22.45 ± 2.51 (17-36) |
| LMR at first episode, mean ± SD (min-max) | 1.21 ± 0.31 (0.7-2.5) |
| LMR at recurrence, mean ± SD (min-max) | 1.43 ± 0.58 (0.9-2.7) |
| Time until recurrence, mean ± SD (min-max), months | 15.32 ± 5.57 (6-28) |
| Gender, n (%) | |
| Male | 296 (79.1) |
| Female | 78 (20.9) |
| Side of pneumothorax, n (%) | |
| Right | 177 (47.3) |
| Left | 197 (52.7) |
| Recurrence, n (%) | |
| Present | 106 (28.3) |
| Absent | 268 (71.7) |
SD: standard deviation; Min: minimum; Max: maximum; LMR: lymphocyte-to-monocyte ratio.
Statistical studies were unable to determine a significant difference in terms of gender and side of pneumothorax regarding the status of recurrence (p > 0.05). Furthermore, gender or side of the pneumothorax did not constitute a difference in the LMR counts (p = 0.075 and 0.727, respectively). However, mean LMR was 1.53 ± 0.35 for the patients who had developed recurrence and 1.08 ± 0.15 for the rest of the cases, showing that mean LMR was significantly elevated in the patients who would encounter a relapse (p < 0.05) (Table 2). With regard to the recurrence-developing group of patients, mean time that had passed until the recurrence was shorter for the cases who had higher counts of LMR considering that statistical analysis indicated a negative if correlation coefficient between these two variables (p = 0, r = −0.81) (Fig. 1).
Table 2 Factors associated with the recurrence
| Parameters | Recurrence (n = 106) | Non-recurrence (n = 268) | p-value |
|---|---|---|---|
| Age, mean ± SD | 21.3 ± 2.42 | 22.09 ± 2.26 | 0.263* |
| Gender, n (%) | 0.081† | ||
| Male | 83 (28) | 213 (72) | |
| Female | 23 (29.5) | 55 (70.5) | |
| LMR at first episode, mean ± SD | 1.53 ± 0.35 | 1.08 ± 0.15 | < 0.001* |
| Side of pneumothorax, n (%) | 0.848† | ||
| Right | 51 (28.8) | 126 (71.2) | |
| Left | 55 (27.9) | 142 (72.1) |
*ANOVA: analysis of variance.
†Chi-square. SD: standard deviation.

Figure 1 Relation of lymphocyte-to-monocyte ratio and the time between first episode and recurrence of pneumothorax.
LMR demonstrated a 70.8% sensitivity and a 94.4% specificity in predicting a potential recurrence for a cut-off value of 1.25 (area under the curve: 0.931, p = 0.001) (Fig. 2).
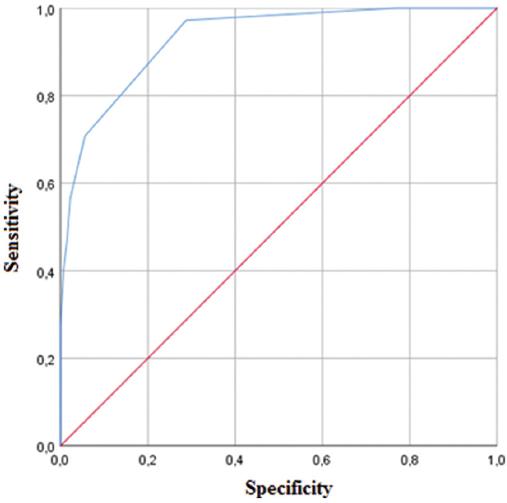
Figure 2 Receiver operating characteristic analysis of lymphocyte-to-monocyte ratio as the predictor of recurrent pneumothorax.
Among a total of 442 cases with the first episode PSP, 68 patients were only observed clinically and radiologically and discharged without any additional treatment or intervention. Thoracoscopy was performed for 78 (73.6%) and thoracotomy for 26 (24.5%) cases who had developed recurrence whereas 2 (1.9%) patients who had disapproved surgery were treated with tube thoracostomy.
Discussion
The findings of this study show that LMR exceeding the threshold value of 1.25 at the first episode of pneumothorax may contribute to predict a potential recurrence.
PSP more frequently occurs in young males with tall and thin habitus whereas bullous parenchymal lesions and smoking are considered as definite risk factors2,4-8. Although the optimal management strategy of first-episode PSP is still controversial, techniques of observing small PSPs without intervention and placing small-bore chest tubes for larger PSPs only if the attempts to success by simple aspiration fail have been approved9. A recent study by Brown et al. reported that conservative management of moderate-to-large PSPs provided resolution of pneumothorax within 8 weeks and resulted in lower rates of recurrence when compared to interventional treatment10. Recurrence of PSP ranging from 16% to 52% and progressively increasing incidence of subsequent recurrences constitutes a significant challenge for both patients and physicians2,5.
Histopathologic findings in the surgical specimens from the patients with pneumothorax mostly conform with chronic inflammation that demonstrates eosinophilic pneumonia-like changes, pleuritis, and hemosiderin deposition in both pleura and lungs11. This evidence has arised the efforts to consider the inflammatory events associated with pneumothorax to predict a potential relapse. De Smedt et al. reported that peripheral blood analysis in patients with first-episode pneumothorax indicated an increase in white blood cell, neutrophil, monocyte, and eosinophil counts and also a non-significant decrease in lymphocyte counts when compared to the control group of healthy individuals12. A study by Selvi et al. also announced that elevated neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios were associated with recurrence in the patients with PSP13.
Utilization of LMR was announced to be efficient in the diagnosis and the determination of prognosis in both inflammatory diseases and malignancies. LMR was reported as an independent prognostic factor in the patients following antituberculous treatment and also a valuable independent indicator to identify the extent of involvement for active ulcerative colitis14-16. Moreover, recent studies reported that LMR was instructive in obtaining additional prognostic information in malignancies including colon cancer, hepatocellular carcinoma, and follicular lymphoma17-19. The current literature does not include any studies that address LMR as a risk or a predictive factor for the recurrence of pneumothorax. In this series, the presence of elevated LMR noticed at the first episode was related with a relapse. Moreover, the time interval until the recurrence demonstrated a significant negative correlation with higher counts of LMR. All these findings imply that LMR that elevates in relation to the severity of inflammatory processes lends assistance to predict the recurrence of pneumothorax as well as the prognosis of several malignancies. However, multicentered prospective studies with larger study populations and multivariate analysis are needed.
The principal limitations were the retrospective design over a long period of time during which the management for PSP has evolved and the strict norms for the exclusion of cases with secondary spontaneous pneumothorax, smoking, and a past history of chest surgery.











 text new page (beta)
text new page (beta)


