Introduction
Transplant activity in Mexico is coordinated centrally and close to 3000 renal transplants that are performed across the country, with over 550 brain-dead organ donors every year1. Kidney transplantation represents the treatment of choice for patients with end-stage renal disease (ESRD) but, worldwide, organ availability has decreased significantly, directly, or indirectly associated with the severe acute respiratory syndrome coronavirus pandemic 2 (SARS-CoV-2)2-4.
The pandemic has limited the access for patients with kidney disease to continue with the transplant protocol; by health policies and the fear of contagion and its consequences, reason why they have stopped going to their medical units. This, together with the level of kidney damage and the crisis derived from the lack of donors, has contributed to ineffective control and monitoring culminating in accelerated organic deterioration leading to death. It should be kept in mind that during outbreaks, medical staff and health-care capacity might be inadequate if massive widespread occurs, and this will adversely affect the quality of patient care5.
A study conducted in Spain reported that the average number of transplants performed in 2019 decreased considerably in the first months of 20206. In Mexico, organ procurement surgeries have been severely affected as of the second quarter (Q2) of 2020, with zero multi-organ donations throughout the country. On the ongoing months until December (Q2-Q4), 51 multiple organ donations were performed, 88% less than the previous year with 433.
The state of Yucatan was not the exception in this struggle; during 2020, only two brain-dead organ donors procurement surgeries were done, while on a yearly basis are performed 9-20. Regarding living donor kidney transplantation, it has also been halted at almost all centers and a limited number of units have been able to resume some activity7.
There are different reasons that explain the decrease in donation and transplantation activities during the outbreak. In the context of an overwhelmed health-care system, there has also been a decline in the number of elective admissions to the hospital. The logistical problems are frequent, either associated with restricted mobility of health teams6 or due to the restriction of outpatient medical control with the consequent delay in medical care.
Nowadays, technological improvements make it easier to reach patients at home through telemedicine practices aided by cellphones, smartphone apps, video calls, and smartwatch apps.
Considering that most ESRD patients are at high risk of developing severe COVID-19, remote follow-up access methods will help patients follow-up5. Patients who may not efficiently use these technologies can be followed by phone, and in case of drug changes or laboratory tests, patients should come to the hospital with appropriate precautions.
Managing kidney transplant recipients require a sustainable infrastructure that can provide reliable medical care both before and after transplantation. COVID-19 pandemic has disrupted transplantation processes, leading a decrease in the number of transplant procedures, and resulted in changes in the practice of control and follow-up before and after transplantation8.
The impact of the pandemic has been noted in patient care, transplant centers, and national and local health policies8. The increase in mortality on the waiting list (WL) has become a consequence of the pandemic6 that will continue to have a negative effect long after the pandemic has subsided. This situation should be an alert that result in the protection of patients more effectively and devise rational policies for transplant decisions and establishing a strong health system8.
For all of the above, the aim of the study was to determine the mortality of patients on the WL for renal transplantation with a cadaveric donor in a third-level referral hospital of medical care in the state of Yucatan, Mexico. The purpose was to demonstrate the impact derived from the suspension of activities associated with the care of kidney disease, as well as to compare the risk-benefit of accessing a kidney transplant, in the context of the pandemic, with remaining on the WL without medical follow-up.
Materials and methods
A retrospective study was carried out with patients under a kidney transplant protocol from a tertiary hospital in the state of Yucatan, Mexico and who died. Data from February 2019 to March 2021 were analyzed.
Patients ≥ 18 years of age, who were on the national computer system WL and who were contacted by telephone were included in the study. The variables included were sex, age, body mass index (BMI), blood type, duration of renal replacement therapy (RRT), etiology of chronic kidney disease, and comorbidities. Patients who died in the aforementioned period were considered. As a cause of death, COVID-19, complications typical of kidney disease, acute myocardial infarction (AMI), and other causes were considered.
The information was divided into two periods, from February 2019 to February 2020, and from March 2020 to March 2021. The mortality data from both periods were compared with each other considering those from 2019-2020 as patients with medical care comprehensive and 2020-2021 as patients with delay in their medical care.
Descriptive statistics were performed with measures of central tendency and dispersion. The data were presented in means ± SD and percentages, according to the type of variables. Kaplan-Meier analysis was performed to compare the number of deaths between both periods. p ≤ 0.05 was considered statistically significant; a systematic error (SE) ≤ 0.05 was considered clinical significance. Odds ratio (OR) between death from COVID-19 and death from complications derived from underlying kidney disease, AMI, and other causes was calculated. In addition, the OR was calculated between deaths before the pandemic (those who underwent medical follow-up, according to the WL protocol) and those that occurred during the pandemic, that is, those who were delayed in their medical care due to the restriction admission to any of the areas of the hospital involved with their comprehensive treatment.
Results
Of the 333 patients included in the National Computer System a total of 144 were excluded because the phone number was incorrect or inactive. Of the 189 patients contacted, 50 deaths were reported, 13 between February 2019 and 2020 and 37 between March 2020 and 2021 (Fig. 1).

Figure 1 Flow chart of patients anlyzed from the national computer system.The flow chart shows the selection procedure for patients admitted to the study. Many patients could not be reached by phone, making it difficult to track their outcome.
Demographic and clinical characteristics are described in table 1. Patients death mean age was 48.5 ± 11.4 years, 66% were men, with a BMI of 26.7 ± 4.8 (Fig. 2), and 76% on blood group 0 list, with diabetes and hypertension as the main cause of ESRD, with 4.6 ± 2.6 years on RRT, most on peritoneal dialysis (64%). Comorbidities were frequent, as shown in table 2.
Table 1 Baseline characteristics of deceased patients on the kidney transplant waiting list
| Variables | Descriptive data |
|---|---|
| Age (years) | 48.56 ± 11.42 |
| Weight (kg) | 68.44 ± 16.18 |
| Height (m) | 1.57 ± 0.1 |
| Body mass index (kg/m2) | 26.73 ± 4.82 |
| Duration of renal replacement therapy (years) | 4.6 ± 2.6 |
| Sex | |
| Men | 66% |
| Women | 34% |
| Blood Group | |
| 0 | 76% |
| A | 20% |
| B | 4% |
| Renal Replacement Therapy modality | |
| Hemodialysis | 36% |
| Peritoneal dialysis | 64% |
| Cause of chronic kidney disease | |
| Hypertension | 28% |
| Diabetes mellitus | 34% |
| Nephrolithiasis | 2% |
| Polycystic Kidney Disease | 8% |
Numerical variables are expressed as means with their standard deviation (± SD); qualitative variables are expressed as a percentage. The data correspond to a sample of 50 deceased patients.

Figure 2 Distribution by body mass index (BMI). 50% of the patients were classified as overweight; this must be studied to determine as an independent risk factor for developing severe COVID.
Table 2 Distribution of comorbidities identified in deceased patients on the kidney transplant waiting list
| Comorbidities | Percentage |
|---|---|
| Hypertension | 60 |
| Diabetes mellitus | 42 |
| Nephrolithiasis | 2 |
| Ischemic heart disease | 6 |
| Depression | 2 |
| Anemia | 10 |
| Hyperparathyroidism | 8 |
| Dyslipidemia | 6 |
| Number of comorbidities | |
| 1 | 52 |
| 2 | 30 |
| 3 | 14 |
| ≥ 4 | 2 |
About 74% of the deaths occurred during COVID-19 pandemic, but only 18% where directly related to SARS-CoV-2 infection; the majority was associated to non-COVID-19 causes. Most deaths occurred during the pandemic, they were attributed in 68% of the cases due to delay in follow-up clinic visits.
COVID-19-related death risk for an ESRD patient on the WL in 2020 was OR = 5.04 (IC 95%: 1.65-7.14; p = 0.023). The OR between death for an ESRD patient on the WL and delay in follow-up clinic visits was 6.59 (IC 95%: 2.7-16.2; p = 0.008). OR for others variables is shown in table 3.
Table 3 Comparison of the OR of death from delay in medical care and death from COVID-19
| OR | CI95% | p | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| OR of death from COVID-19 | 5.04 | 1.65 | 7.14 | 0.023 |
| OR of death due to delay in medical attention* | 6.59 | 2.7 | 16.28 | 0.008 |
| OR of death due to complications associated with chronic kidney disease and hypertension | 5.78 | 0.65 | 51.237 | 0.086 |
| OR of death due to complications associated with chronic kidney disease and diabetes mellitus | 3.81 | 0.6 | 24.5 | 0.067 |
| OR of death due to complications associated with chronic kidney disease and ischemic heart disease | 0.93 | 0.85 | 1.010 | 0.446 (SE 0.037) |
| OR of death due to complications associated with chronic kidney disease and dyslipidemia | 0.38 | 0.39 | 3.72 | 0.41 |
| OR of not dying due to anemia | 0.89 | 0.79 | 0.99 | 0.313 (SE 0.041) |
| OR of not dying due to hyperparathyroidism | 0.9 | 0.82 | 0.99 | 0.373 (SE 0.039) |
| OR of dying from the etiology of chronic kidney disease (nephrolithiasis) | 0.98 | 0.93 | 1.023 | 0.67 (SE† 0.033) |
*The concept of delay in medical care was operationally defined as the period between March 2020 and March 2021 (during the pandemic), which was characterized by the temporary suspension of comprehensive medical care provided to patients with chronic kidney disease who require transplantation, which were on the national computer system waiting list.
†Systemic error. The ES ≤ 0.05 means that the clinical phenomenon occurs, although statistically it is not possible to confirm it, probably due to the sample size. OR: odds ratio
Finally, figure 3 shows the cumulative survival rate of ESRD patients on WL for kidney transplantation, whether or not they had delayed medical care during the pandemic (Fig. 3).
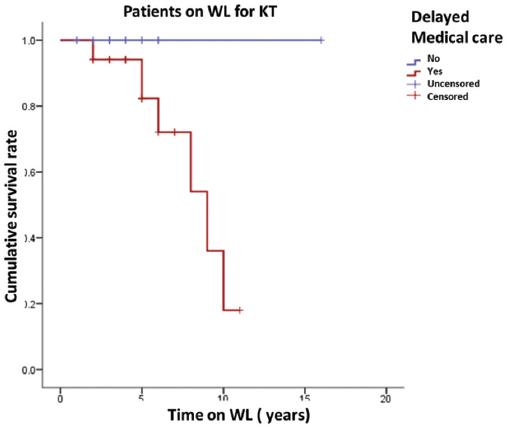
Figure 3 Survival before and during the pandemic. The figure shows a comparison between the deaths on the waiting list for kidney transplants that occurred before and during the pandemic. (From February 2019 to February 2020, blue line; from March 2020 to March 2021, red line). There was an increase in patients who died during the pandemic due to the temporary suspension of health services because follow-up visits and transplantation were not considered a priority, such as COVID management. This policy was adopted as a measure to prevent infections caused by SARS-CoV-2 in vulnerable patient groups.
Discussion
During 1Q 2020, there was a reasonable fear as to whether already immune compromised transplanted population had an increased risk of severe SARS-CoV-2 or death development, which resulted in many transplant societies and regulatory agencies recommended temporary suspension of transplant activity. Mexico published their own on March 17, 2020 with very similar policies9-11.
However, during the following months and the emerging knowledge regarding the clinical course in transplanted population, where apparently no worse prognosis developed, led to reconsideration of the measures taken. On June 2020, Mexico published a reactivation plan, which included chest CT and PCR screening. Unfortunately, the recovery of donation and transplants programs in the country was poor, unlike those reported in the US or Spain12-14.
This disparity may correspond to the fact that the reality in emerging countries is very different from that of the first world. Kute et al.15 mention several possible obstacles that may affect the management of pandemic outbreaks and the reactivation of transplant programs: limitations in protective equipment; high prevalence of asymptomatic infections; availability of reverse transcription polymerase chain reaction tests; isolation rooms and beds in intensive care units; functions duplicity in healthcare workers; the constant changing dynamics and waves of this pandemic; and, ultimately, the pressure on the already overwhelmed health-care system.
Despite these considerations, doubts raised as to whether recommendations for temporary suspensions of transplant activity were the best way to act in our country. The need for scientific evidence to support reactivation became a priority.
The endpoint of this study showed a 19.5% of mortality rate in ESRD patients on the WL for kidney transplantation during the last pandemic year, in comparison with a 6.8% mortality rate noted in 2019. A significant increase on the death risk developed.
One might question whether the deaths were secondary to COVID infection; however, only a quarter of them were directly associated to it. Most deaths were due to delay in medical care because of loss in follow-up clinic visits and lack of access to kidney transplantation.
The most relevant factor revealed that the risk of death because of SARS-CoV-2 infection is lower than the risk of death if the patient remains on the WL and is not transplanted. We suggest reconsidering the adopted measures in our country at the beginning of the pandemic and reactivate all transplantation programs.
Miller et al.16 reported a rise in kidney WL mortality in the United States (adjusted hazard ratio [aHR], 1.37; 95% CI: 1.23-1.52), especially during the he first 10 weeks after the declaration of a national emergency. Mortality was not significantly for liver, pancreas, lung, and heart. They also hypothesized that the mortality rate increase may be due to delays in transplants.
Understanding the reasons for higher waitlist mortality among kidney candidates will require continued study. Social distancing may have been more challenging for kidney transplant candidates undergoing in-center dialysis.
Case series published in the United States with more than 400 solid organ transplant recipients have provided information on the clinical presentation of COVID-19 in this population, with mortality in the range of 6-30%17.
Clarke et al.18 analyzed a cohort of 1 433 patients with end-stage kidney disease, resulting that COVID-19 infection was more commonly diagnosed in the waitlist patients (p = 0.001), than on transplant population.
Pereira et al.19 reported a series of 90 solid organ transplant recipients with COVID-19 with the following symptoms: fever (70%), cough (59%), and dyspnea (43%); 76% required hospitalization and 35% mechanical ventilation. Overall mortality was 18%. Mexican regulatory agencies statistics as of December 21, 2020, reported 232 suspected and or confirmed COVID-19 cases in kidney transplant recipients, with 64 deaths (overall 27%)20.
The decrease in transplant activity was not only observed in Mexico. Most transplant centers worldwide temporarily reduced the number of procedures early in the pandemic but did not stopped as in Mexico21-23.
At the end of March 2020, a U.S. survey of 88 transplant institutions reported that 71% had temporarily stopped living donor kidney transplantation and 84% had implemented restrictions on deceased donor kidney transplantation9.
Another report informed productivity reductions of 51% and 90% in solid organ transplantation procedures in the US and France24. However, at the end of 2020, the activity recovered close to that reached in the previous years; organ donation from deceased donors in the United States increased 6% over 2019. Deceased donor transplantation briefly fell approximately 50% in early April before returning to a more consistent baseline in late May. Living donor transplants decreased 22.6%13.
The negative impact on multi-organ donation in Spain was mostly affected during the March-May 2020 period, coinciding with the worst months of the pandemic. However, according to ONT reports these have recovered to levels close to those registered in 201914, based on a staggered recovery, contrary to what was observed in Mexico, where activity came to an abrupt halt in March and so far, the its recovery has been very limited.
Mexico continues to be on the list of countries with high transmissibility for SARS-CoV-225. In addition to this, the vast majority of first and second level care hospitals (donor recruitment centers) as well as third level and high specialty hospitals (transplantation centers) had the need to use their health-care resource converted into COVID units, severely affecting activity in the whole country, in terms of transplantation. It is necessary to review the public policy for the management of the pandemic, so that high specialty hospitals continue their transplantation activity, while other lower-level hospitals continue the care for COVID-19 patients. It is vital to adopt mitigation strategies such as donor screening, resource planning, and a staged approach to transplant volume considerations as local resource issues demand.
The management of immunosuppression in transplant patients with COVID-19 is not well defined. Current recommendations are based on reducing immunosuppression according to the severity, beginning with suspension of antiproliferatives and continue with calcineurin inhibitors, while steroids are not discontinued.
The use of any therapy for COVID-19, such as chloroquine, azithromycin, remdesivir, favipiravir, tocilizumab, convalescent plasma, and among others, should be used cautiously, based on the available evidence at least for the general population and taking into account peculiarities of the transplanted patient and possible drug interactions26.
Conclusions
This study aims to help quantify the negative impact of the COVID-19 pandemic on ESRD patients on the WL at a hospital in Yucatán, Mexico and serves as a good example of the devastating impact on withholding organ harvesting and renal transplantation activity.
The death OR for an ESRD patient on the WL with delay in follow-up clinic visits and transplantation withhold is statistically higher than COVID-19 death OR.
The risk of dying due to lack of prompt access to transplantation is way much higher than the presumed risk of dying from COVID, so we hope that these findings can help inform new policies and specific service strategies to bring transplant activity back to previous rates.











 text new page (beta)
text new page (beta)


