Introduction
Endotracheal tubes (ETTs) are frequently used to ensure and maintain airway safety in patients undergoing general anesthesia. The cuffs of ETTs allow for positive pressure ventilation by preventing the leak of liquid and gas between the tracheal wall and the tube and the aspiration of the stomach content into the lungs and the environmental pollution caused by the release of the used medical gases to the outer environment1.
Patients may develop life-threatening respiratory complications ranging from a postoperative sore throat (POST), hoarseness, swallowing difficulty, cough, and throat dryness to tracheal necrosis after intubation2. Among these complications, the incidence of sore throat after general anesthesia varies from 21% to 65%3. Although the exact cause of POST, which leads to poor anesthesia experience by negatively affecting patient comfort, is unknown, it is thought to be due to irritation and inflammation mechanically caused by the cuff part of the ETT on the tracheal wall. Therefore, it is extremely important to keep the ETT cuff pressure at 20-30 cm H2O to prevent cuff-related complications in an intubated patient4,5. Environmental factors such as intra-cuff pressure, intraoperative high airway pressure, and use of nitrous oxide, patient-related factors such as differences in tracheal size and tracheal position of the cuff, personal factors such as laparoscopic surgery and patient positions, especially Trendelenburg position, and differences in the shape and diameter of the cuff may be effective in complications6,7.
Pharmacological, non-pharmacological, or various methods have been used to reduce the side effects associated with mucosal irritation caused by ETT insertion8-11. Complications such as sore throat and hoarseness can be frequently seen in traditionally used cylindrical ETTs with high-volume and low-pressure cuffs due to both the large surface area and the easy diffusion of medical gases into the cuff, resulting in excessive swelling of the cuff and therefore high pressures on the tracheal wall12. This is especially important in cases where long-term use of ETT is required. In recent years, conical-cuff tubes have been used, unlike traditional ETTs. Compared to traditional cuffs, conical-cuff ETTs can reduce POST and hoarseness because of smaller cuff diameter and cuff-trachea contact area13.
The primary aim of this study was to compare the cuff pressures of cylindrical- and conical-cuff ETTs inflated with a saline, the frequency, and severity of POST complications in the post-operative 24 h period in surgeries lasting longer than 120 min. The secondary aim was to compare the effects on post-operative analgesic consumption of the groups.
We hypothesized that conical-cuff ETTs would result in a reduction in the incidence of POST and potentially less analgesic consumption in surgeries longer than 120 min.
Materials and methods
This prospective and clinical study was conducted in the operating room of anesthesiology and reanimation between October 2020 and July 2021 after obtaining approval for the study from the Local Ethics Committee (no. 2020/299). The study included 104 patients aged 18-65 years in the ASA I-III risk group, with an expected operative time longer than 120 min in the supine position, who were scheduled for surgery by the urology, obstetrics and plastic, reconstructive, and esthetic surgery in the operating room of our hospital. All patients were informed about the purpose of the study and their written and verbal consent was obtained for participation in the study. Two patients with deformed cuff valves and unreliable cuff pressure measurements and two patients with an operative time shorter than 120 min were excluded and the study was conducted on a total of 100 patients.
Those with neurological and psychiatric disorders, severe cardiovascular and respiratory diseases, those who had an upper respiratory tract infection in the past 10 days and who were receiving treatment, morbidly obese individuals, those with known allergies to anesthetic agents, alcohol or drug addiction, a history of bronchospasm, head-and-neck surgery, laparoscopic surgery, excessive Trendelenburg position, unanticipated difficult airway or difficult intubation and tracheostomy, an estimated operative time shorter than 120 min, a history of malignant hyperthermia, and a cuff pressure of over 40 mmHg during the follow-up periods were excluded from the study.
All patients in both groups received 0.15 mg/kg midazolam for premedication 15 min before the induction of anesthesia in the operating room. After patients were transferred to the operating table, they were monitored with electrocardiography, heart rate (HR), non-invasive mean arterial pressure (MAP), peripheral oxygen saturation (SpO2), end-tidal CO2 (EtCO2), (Spacelabs Healthcare, Snoqualmie, WA, USA), and bispectral index (BIS) (Aspect Medical Systems, Norwood, MA, USA).
After 3 min of preoxygenation with 100% oxygen, 1 mg/kg fentanyl, 1 mg/kg lidocaine, 2-3 mg/kg propofol, and 0.6 mg/kg rocuronium were administered for anesthesia induction. Following sufficient time for muscle relaxation, ETT was inserted when the BIS value decreased below 60 (Macintosh 3 or 4 blades). Before the ETT insertion procedure, cuff leak was checked, and straight tubes with an internal diameter of 8.0-8.5 mm were used for male patients and 7-7.5 mm for female patients. After endotracheal intubation, the cuffs of the ETTs of the patients included in the study were monitored with the help of a "cuff manometer" (VBM, Medizintechnic GmbH, Germany), by setting to 25 cm H2O. Using the sealed envelope method, patients were divided into two groups: patients with cylindrical-cuff ETTs inflated with saline (Group C, n = 50) and patients with conical or tapered-cuff EETs inflated with saline (Group T, n = 50) (with the aid of a computer). Following a successful ETT insertion, the patients were ventilated with a tidal volume of 6-8 mL/kg, a frequency of 10-12/min, and EtCO2 of 32-35 mmHg. In both groups, anesthesia was maintained with a 50/50%
O2/air mixture and a 2-3% sevoflurane gas mixture. An infusion of 0.5-2 mcg/kg/min remifentanil was administered as an analgesic for the maintenance of anesthesia. Intraoperative anesthesia depth was set to be between 40 and 60 BIS. When BIS was > 60 in the absence of tachycardia and hypertension, the sevoflurane concentration was titrated to a maximum of 3% by 1% increments. Muscle relaxants, hypnotic, and analgesic drugs were administered when necessary. HR, SpO2, MAP, BIS value, EtCO2, inspired oxygen value, airway pressure, and cuff pressure of all patients were recorded at baseline, during and after intubation at 20-min intervals, and just before extubation.
All patients were extubated when their respiratory depth and rate were sufficient and cardiovascular findings were stable after removal of oropharyngeal secretions. Patients were transferred from the operating room to the post-anesthesia care unit (PACU) when they achieved sufficient muscle strength (response to commands of raising their head and moving their limbs), with sufficient airway stability. Patients with an Aldrete score ≥ 9 were transferred to the ward from the PACU. In addition, post-operative sore throat with and without swallowing were evaluated with the Numerical Rating Scale (NRS) scoring system in both groups that were followed up at post-operative 2, 6, and 24 h throughout the 24-h period. Contramal 50 mg IV was administered to those with an NRS > 3 in the PACU and ward. The amount of additional analgesic use during this period was recorded.
Statistical analysis of data
IBM SPSS 23.0 statistical software package was used for the analysis of the data. Descriptive statistics of analyzed results were presented as numbers, percentages for categorical variables, and as mean, standard deviation, and quartiles for numerical variables.
The normality of variables was checked with the Kolmogorov-Smirnov test. In the comparison of the mean values of the measurement variables between the groups, the t-test was used for normally distributed variables, and the Mann-Whitney U test was used for non-normally distributed variables. The Chi-square test was used for the comparison of categorical data. The level of statistical significance was set at p < 0.05.
The reliability of the power analysis using the mean and standard deviation values of the groups for sore throat, which is the main hypothesis of the study, showed that sore throat during swallowing at 2 and 6 h would provide a power of 100% and sore throat during swallowing at 24 h would provide a power of 99.98% by including a total of 100 patients with cylindrical- and conical-cuff ETTs (50 patients for each group).
Results
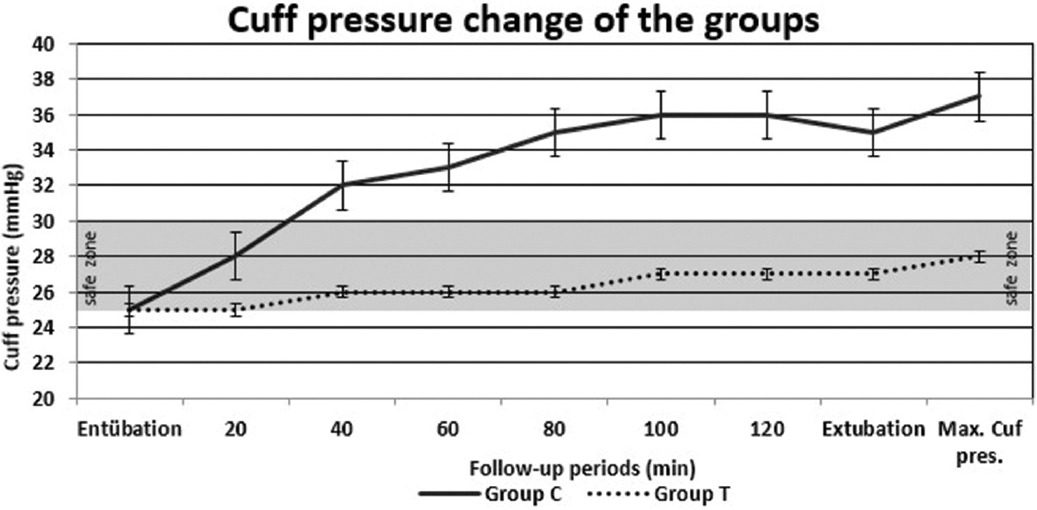
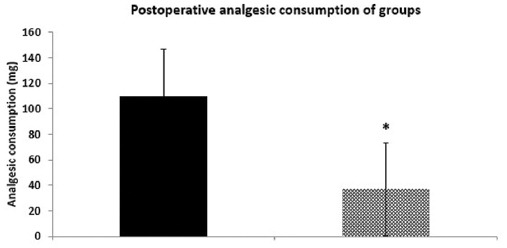
The demographic, clinical characteristics, intraoperative hemodynamic data, and type of surgery of the patients are shown in Table 1 (p > 0.05). The cuff pressure and maximum cuff pressure values at all measurement points after intubation and just before extubation at the end of the operation were significantly lower in Group T than in Group C (p < 0.05) (Fig. 1). The change of post-operative sore throat is shown in Table 2. Post-operative 2-h, 6-h, and 24-h sore throat with and without swallowing were significantly lower in Group T than in Group C (p < 0.05). The post-operative 24-h total analgesic consumption was significantly lower in Group T than in Group C (p < 0.05) (Fig. 2).
Table 1 Demographic, hemodynamic, and clinical characteristic
| Group C (n = 50) | Group T (n = 50) | p | |
|---|---|---|---|
| Demographic data | |||
| Age (year) | 49.2 ± 13.3 | 43.7 ± 15.6 | 0.097 |
| Gender (female/male) | 31/19 | 34/16 | 0.685 |
| BMI (kg.m−2) | 26.9 ± 3.3 | 26.2 ± 3.1 | 0.281 |
| ASA (I/II/III) | 14/12/4 | 13/14/3 | 0.511 |
| Intraoperative data | |||
| Operation time (min) | 147.5 ± 33.3 | 153.8 ± 32.8 | 0.405 |
| Endotracheal entubation time (min) | 147.7 ± 33.6 | 159.2 ± 33.3 | 0.06 |
| Hemodynamic data | |||
| HR (beat/min) | 61.01 ± 10.6 | 60.09 ± 15.42 | 0.386 |
| MAP (mmHg) | 66.4 ± 7.2 | 65.1 ± 5.9 | 0.514 |
| Type of surgery | |||
| General surgery | 30 | 34 | |
| Gynecologic surgery | 12 | 9 | |
| Plastic surgery | 8 | 7 |
Values are means (standard deviation) or number of patients (n). Group C: cylindrical-shaped cuff tubes; Group T: tapered-sahed cuff tubes; ASA: American Society of Anesthesiologists Classification; BMI, body mass index; HR, heart rate; MAP, mean arterial pressure.
Table 2 Post-operative sore throat change in groups with and without swallowing
| Group C (n = 50) | Group T (n = 50) | p | |
|---|---|---|---|
| Sore throat with swallowing at the 2nd h postoperatively | 4.5 (0-7) | 3 (1-4) | < 0.001 |
| Sore throat without swallowing at the 2nd h postoperatively | 4 (0-7) | 1 (0-4) | < 0.001 |
| Sore throat with swallowing at the 6th h postoperatively | 3 (0-5) | 0 (0-3) | < 0.001 |
| Sore throat without swallowing at the 6th h postoperatively | 3 (0-5) | 0 (0-3) | < 0.001 |
| Sore throat with swallowing at the 24th h postoperatively | 1 (0-4) | 0 (0-2) | < 0.001 |
| Sore throat without swallowing at the 24th h postoperatively | 1 (0-4) | 0 (0-2) | < 0.001 |
Values are medyan (min-max). Group C: cylindrical-shaped cuff tubes; Group T: tapered-sahed cuff tubes
Discussion
The present study demonstrated that intraoperative cuff pressures were lower, and postoperative sore throat and analgesic consumption were lower in patients who used conical-cuff ETTs inflated with saline in surgeries lasting longer than 120 min in the supine position compared to those with cylindrical-cuff ETTs.
ETT is frequently used in the operating room, intensive care units, and emergency rooms to control the airway and prevent possible complications. Mechanical ventilation can be provided to patients for a long time in intensive care units and some particular surgeries. The cuff parts of ETTs are designed to prevent aspiration and allow positive pressure ventilation, provided that adequate cuff pressure is maintained14. Respiratory complications associated with cuffed ETTs used during intubation should also not be overlooked. Both over- and under-inflation of the cuffs are of great importance because of the association with clinically significant complications. The cuff pressure of ETT must exceed the sum of the hydrostatic pressure on the cuff and the negative pressure created during inspiration15.
Exposure to time-independent cuff pressure combined with high cuff pressures can cause laryngotracheal morbidities in the tracheal mucosa. It is known that tracheal capillary perfusion pressure is between 30 and 44 cmH2O in vivo studies. When the ETT cuff pressure exceeds 30 cm H2O, the blood supply to local tissue and perfusion of the tracheal mucosal wall and surrounding anatomical structures begin to deteriorate16,17. It has been reported that the blood supply, especially to the anterolateral portion of the trachea, is compromised at pressures exceeding 30 cm H2O, causing it to become obstructed at pressures exceeding 50 cm H2O, and the tracheal circulation may completely stop at pressures above 60 cm H2O18. Therefore, as a general approach, it is recommended that the ETT cuff pressure be kept between 20 and 25 cmH2O3.
The incidence of POST resulting from high cuff pressure after endotracheal intubation, which is one of the respiratory complications associated with the deterioration of the integrity of the microcirculation and tracheal mucosa, has been reported to be 30-70%3. There may be damage to any part of the pharynx, larynx, or trachea. The reasons for the increase in ETT cuff pressures include lateral wall pressure, ETT insertion time, patient position, head position, cuff volume, temperature, nitrous oxide use, and other lesser-known factors16,19-23.
Medical gases used in anesthesia procedures including Trendelenburg position, laparoscopic surgery, and general anesthesia with low flow N2O, which is frequently used as an analgesic in general anesthesia, can diffuse into ETT cuffs. As a result, an intraoperative increase in ETT cuff pressures can lead to undesirable respiratory complications such as POST and hoarseness, as well as a bad anesthesia experience24,25. Many pharmacological and non-pharmacological studies have been conducted to minimize the intraoperative increase in ETT cuff pressures, to reduce the pressure of the cuff on the trachea, and to prevent POST. Opioid and non-opioid analgesics, local anesthetic agents and adjuvant analgesics, non-steroidal anti-inflammatory drugs, and steroids are among the most frequently used pharmacological agents26. These drugs can be administered systemically, as well as in different forms as a spray, gel around the ETT cuff, intracuff solutions or oral pastil, spray, or mouthwash27. Inflation of ETT cuffs with saline is frequently used to prevent POST in general anesthesia with N2O and in laparoscopic surgeries, especially in the Trendelenburg position, because it is easy to use, simple, and does not have any difficulty in removing from the cuff28,29.
In anesthesia practice, ETTs with high-volume and low-pressure cuffs are frequently used to reduce ischemic complications of the trachea due to high ETT cuff pressure. However, the greater contact area of cylindrical-cuff ETTs with the trachea may cause an increase in the frequency of POST12. In recent years, conical cuffs have been used to prevent POST different from traditional cylindrical cuff shapes. With the geometric structure of the conical-cuff tubes, they are designed to minimize air leakage and microaspiration, as well as to create less pressure on the tracheal wall with less contact area on the tracheal mucosa13. In addition, the less bulky conical-cuff tubes provide less contact with the trachea and ease of passage during endotracheal intubation. A model trachea study conducted by Tsuboi et al. by creating a mechanical test lung reported that the intra-cuff pressure of conical ETTs did not increase as rapidly as in cylindrical cuffs during mechanical ventilation using 66% N2O, with a lower incidence of complications associated with cuff pressures, especially in the post-operative period7. A study by Chang et al. on 191 adult patients scheduled for general surgery, urology, orthopedics, and gynecological operations showed that the overall incidence of POST in the postoperative 24-h period was lower in conical-cuff tubes compared to cylindrical-cuff tubes (32% vs. 54%)13. In the present study, the intraoperative cuff pressures, maximum cuff pressure, and the frequency of POST in the post-operative 24-h period were found to be significantly lower in conical-cuff tubes than in cylindrical-cuff tubes (52% vs. 69%, respectively). Similar to the study of Chang et al., the present study showed a lower incidence of complications in the group using conical-cuff ETTs. However, we think that the reason for our higher incidence of POST in the conical-cuff ETT group (32% vs. 52%) than this study is due to the longer mean duration for endotracheal intubation in our study (115 ± 37 min vs. 159.2 ± 33.3 min).
A study by Bernhard et al. on humans reported that cuff pressures higher than 50 cm H2O caused ischemic changes in the tracheal wall within 15 min30. One of the most important conclusions to be drawn from here is how important time is with high ETT pressures. Therefore, it is very important to monitor cuff pressures closely to prevent possible respiratory complications that may be caused by high cuff pressures in long-term surgeries with an endotracheal intubation duration exceeding 2 h under general anesthesia.
In prolonged operations under general anesthesia with an endotracheal intubation duration exceeding 2 h, the frequency of POST increases due to the prolonged contact of the cuff with the tracheal mucosa5. To reduce the frequency of POST, especially in long-term surgeries, it would be beneficial to minimize the cuff volume in the trachea and the cuff-trachea contact area due to the greater tracheal mucosa contact of high-volume and low-pressure cylindrical-cuff ETTs. A study by Loeser et al. investigating the effect of ETTs with different cuff designs on POST reported that high-volume cuffs led to a greater incidence of POST as a result of the larger cuff-tracheal contact area12.
Conical-cuff tubes, on the other hand, have a sealing zone where the outer diameter of the cuff corresponds to the inner diameter of the trachea when inflated. The sealing area and the lower part of the cuff are not folded in the trachea due to their geometric shape and remain limited to the upper part of the cuff. As a result, the use of ETTs with conical cuffs has been found to potentially reduce POST and hoarseness as a result of the smaller cuff-tracheal contact area13.
In an in vitro experimental study, Dave MH et al. determined that cylindrical- and conical-cuff ETTs placed in the trachea of different sizes could cause a decrease up to 40% in the areas of contact with the trachea (cross-sectional areas; 530 mm2, 314 mm2)31. In the present study, the decreased frequency of POST in the group using the tapered-cuff ETTs compared to the cylindrical-cuff ETTs can be explained as the result of this decrease in the contact area of the cuff to the trachea.
There are a limited number of studies in the literature investigating the post-operative respiratory effects of cuff exposure due to endotracheal intubation times longer than 120 min under general anesthesia in the operating room. Souissi et al. showed a decreased frequency of respiratory complications associated with ETTs in the group with ETTs inflated with 160 mg alkalinized lidocaine compared to the group with ETTs inflated with saline in surgeries lasting longer than 120 min under general anesthesia without the use of nitrous oxide11. Moreover, Liu et al. showed that among those who were scheduled for elective surgery under general anesthesia and who had an endotracheal intubation duration of 120-180 min, the group with values measured regularly intraoperatively at regular intervals had a decreased frequency of complications associated with endotracheal intubation, such as cough, sore throat, hoarseness, and bloody sputum in the post-operative 24-h period compared to the non-measured group. Besides, it has been reported that the frequency of sore throat increases as the duration of endotracheal intubation is prolonged, even though the cuff is checked at regular intervals5. To compare the effects of different cuff shapes on the sore throat in the present clinical study, patients with operative times longer than 120 min (from 125 to 225 min) were included. The reason for this was that the stretch receptors in the tracheal mucosa responsible for the cough reflex would be activated in such a period32. In the limited number of studies investigating the frequency of POST associated with endotracheal intubation in the supine position, especially in long-lasting surgeries, the cuffs were inflated with pharmacological agents or saline. Apart from this approach, the conical-cuff ETTs, which have been used recently, were used in the present study. Although the cuff pressures in both groups increased over time, the conical-cuff ETT pressures remained within the "safe zone" recommended in the literature, while the cylindrical-cuff ETT pressures increased above 30 cm H2O. Moreover, the maximum cuff pressures of the groups were found to be lower in the conical-cuff group than in the cylindrical-cuff group, at levels that would not impair tracheal perfusion (28.56 ± 2.79 cm H2O, 37.18 ± 3.65 cm H2O, respectively). Therefore, we concluded that the use of tapered-cuff ETTs to reduce the contact of the cuff to the trachea in long-term surgeries may provide more clinical benefits by reducing the incidence of POST.
The physical stress caused by POST can affect the patient’s satisfaction, comfort, and activities. The aim of the methods used to prevent this is to reduce the amount of POST and analgesic use and to provide a more comfortable postoperative period33. The present study also found that the use of conical-cuff tubes decreased the post-operative analgesic consumption, and the desired post-operative comfort was achieved with less POST in the post-operative period.
Limitations
This study has several limitations. First, the tracheal mucosal injury could not be directly assessed, and instead, subjective assessment scores were used for the evaluation of patients’ POST after endotracheal intubation. Second, patients were followed up for 24 h postoperatively. Although the frequency and severity of sore throat tend to decrease in the post-operative 24-h period, POST assessment may require longer periods. Finally, anatomical structures such as the upper part of the trachea and its internal diameter differ by geographic region. Since the present study was a single-center study, the results are limited to a specific region. Therefore, there is a need for multicenter studies are needed.
Conclusion
We think that in surgeries lasting longer than 120 min in the supine position, the use of conical-cuff ETTs prevents the increase in intraoperative cuff pressures, reduces the incidence of postoperative sore throat, and accordingly decreases postoperative analgesic consumption compared to cylindrical-cuff ETTs.











 text new page (beta)
text new page (beta)