Introduction
Acute massive gastric distention (AMGD) is a rare condition which associates a high morbidity and mortality rate. Its pathogenesis is still unclear. However, it is sometimes related to alimentary disorders with binge eating behavior, gastric herniation, volvulus, and small bowel obstruction1. If the AMGD evolves, it may lead to gastric ischemia with bacterial infection developing emphysematous and necrotizing gastritis2.
In this case, we report the case of a patient with emphysematous and necrotizing gastritis due to acute massive gastric distention without apparent predisposing cause. Furthermore, in the specimen analysis, Sarcina ventriculi infection was found.
Case report
An 18-year-old female, without comorbidities, presented to the emergency department with severe, continuous, and diffuse abdominal pain for about 24-h. She also associated anorexia, nausea, and coffee-ground vomitus. The patient had ingested pizza, alcohol, and smoked cannabis the day before. She had no previous history of eating disorders or psychiatric pathology. Her BMI was 21 kg/m2. Physical examination revealed abdominal distension with epigastric tenderness and rebound.
Blood test was normal except for elevated blood cell count (30.000/mm3) and neutrophilia (90%). The abdominal radiography showed massive gastric distention. The computed tomography (CT) scan described a markedly distended esophagus, stomach, and duodenum with emphysema of the gastric and duodenum wall, portal venous gas, and abdominal free fluid (Figs. 1-3).

Figure 1 Coronal section view of the abdominopelvic computed tomography scan showing markedly distension of the stomach and gas within the gastric wall.
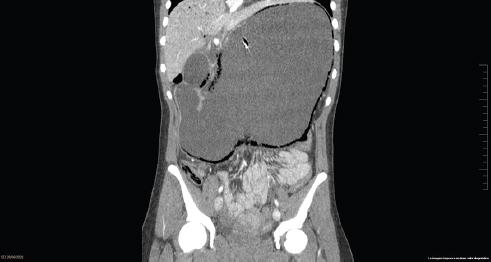
Figure 2 Coronal section view of the abdominopelvic computed tomography scan showing markedly distension of the stomach, gas within the gastric wall and portal vein gas.
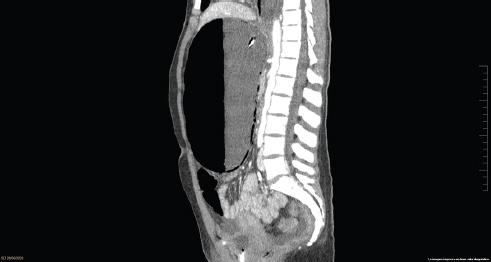
Figure 3 Sagittal section view of the abdominopelvic computed tomography scan showing an extremely distended stomach within gas in the gastric wall. Adequate distance between abdominal aorta and superior mesenteric artery.
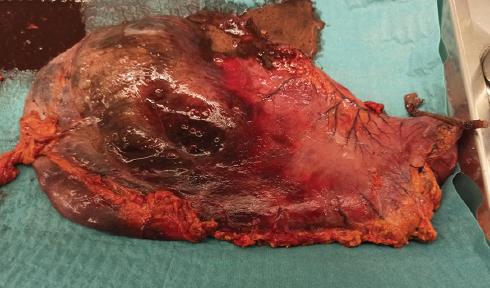
She was treated with nasogastric tube (NG) decompression, proton pump inhibitors (PPI), intravenous fluid resuscitation, and antibiotics but after a few hours the patient became hemodynamically instable. Emergency surgery with total gastrectomy with roux-en-y esophagojejunostomy was performed. During the intervention, necrosis was found affecting the fundus and the gastric body in both anterior and posterior surfaces (Fig. 4). The specimen analysis described necrosis in an 80% of the gastric wall with necrotizing gastritis and emphysematous (Fig. 5). Besides, small and medium vessels thrombosis was found. S. ventriculi was recognized in the biopsies of the gastric specimen. Post-operative course was uneventful, on the 5th postoperative day, the integrity of the anastomosis was assessed by a contrast esophagogram. The patient was discharged on the 10th day of hospitalization with adequate oral intake. She was followed-up on clinics 1 month after discharge and then she came consequently every 3 months for consultation. 1 year after surgery she underwent a CT-scan with oral and intravenous contrast without any significant findings. She is currently having follow-ups every 6 months.
Discussion
Acute gastric distension is a rare entity, firstly described by Duplay et al. in 1833. AMGD is the extreme presentation of this pathology with gastric distension covering from the diaphragm to the pelvis. This entity is mainly related to alimentary disorders with binge eating behavior, psychiatric problems, and alcohol or drug abuse1,2 all of them absents in our patient. Nevertheless, it may also appear in healthy patients. Superior mesenteric artery syndrome must also be discarded3. Furthermore, Brinton et al., in 1859, explained that long-term starvation periods cause atony and muscular atrophy, and a sudden ingestion of food may weaken the stomach4.
AMGD is one of the main causes of gastric ischemia. The stomach is highly vascularized due to a great collateral blood flow with multiple anastomosis. If the intragastric pressure increases, exceeding 20 cm H2O, the intramural flow can be reduced causing ischemia, necrosis, and even perforation. When this last option occurs, it is usually located along the fundus and the greater curvature, as in our patient. Nevertheless, the lesser curvature and the pylorus are rarely affected4,5.
Gastric ischemia may also cause infection of the gastric wall by local bacterial invasion, due to ulceration, or from hematogenous spread and develop emphysematous gastritis (EG)6,7. EG is a rare entity because the vast gastric vascularization and the acid environment prevent the development of infections8. There are several predisposing factors, all of them discarded in our patient, such as chronic alcohol consumption, emesis, steroids, and non-steroidal anti-inflammatory drugs intake, immunosuppression, and gastric wall corrosion with acid or alkali 6,9. It is important to difference between EG and gastric emphysema because the latter is a benign entity meanwhile, EG represents a serious and infrequent pathology with a high mortality rate ranging from 55% to 61%9,10. The main microorganisms associated are anaerobic bacterium (Staphylococcus spp, Streptococcus spp, Enterobacterium ) and sometimes fungi (Candida spp.)9.
S. ventriculi is a GRAM+ anaerobic bacterium that was identified in the biopsies of the patient’s specimen after surgery. This bacterium is associated with delayed gastric emptying because gastric content retention predisposes the growth of the organism, and it gives time to penetrate in the gastric wall. It is thought to cause EG and perforation. However, it is not clear whether Sarcina is a bystander or a pathogen because this bacterium was also found in gastric and feces specimens of healthy individuals, mostly vegetarian11-13. Therefore, there is no consensus regarding the type and the duration of the treatment. Besides, it is not clear whether treatment is necessary in all patients or only in critically ill11. Our patient received a broad-spectrum antibiotic (Piperacilina-Tazobactam) for 10 days covering among others S. ventriculi.
The main clinical symptoms of AMGD are mild epigastric tenderness with distension and emesis. Sometimes, coffee-ground vomitus are associated. However, in certain scenarios, emesis is absent because the massive gastric distention comprises the angulation of the gastroesophageal junction4,5. If fever and chills are present, EG must be suspected as the patient may rapidly decompensate with severe sepsis and shock7.
Because of its rarity, diagnosis is mostly delayed. Abdominal radiography detects gastric distention and pneumoperitoneum, but computed tomography (CT) is the gold standard technique. CT scan may help to identify the etiology, discard other abdominal pathologies, and diagnose complications such as pneumoperitoneum. Besides, in cases of EG, common CT scan findings are gas within the stomach wall and portal venous gas caused by intraluminal air or gas produced by the bacterium6,9.
Prompt diagnosis with rapid relief of gastric distension is crucial. Conservative management is mainly based on gastric decompression, PPI, nil per os, broad spectrum antibiotics, and intravenous fluid resuscitation. A NG tube should be placed but sometimes is inefficient due to the high density of semisolid gastric content. An early treatment may avoid the onset of necrosis and to disregard surgery because the necrosis of the gastric wall usually appears 24-h after the onset of the dilatation5.
If conservative management fails or the CT confirms the presence of necrosis or perforation, surgery should be performed because a delay in surgical treatment results in an 80% of mortality4,5. Regarding surgery, resection of the necrotic stomach is required and even a total gastrectomy if necessary. The gas in the portal territory usually has a favorable progress once the infection is solved with antibiotics and treatment.
Conclusion
AMGD is mainly related to eating or psychiatric disorders and may lead to gastric ischemia and necrosis. EG should be suspected in patients with risk factors and ruled out with CT scan. S. ventriculi might be related to EG but its pathogenic effect is still not clear. Both EG and necrotizing gastritis are rare entities related to gastric distention that must be suspected. An early treatment is crucial because conservative management can be effective, avoiding surgery. If patient does not show improvement despite treatment, surgery must not be delayed to reduce mortality.











 text new page (beta)
text new page (beta)