Introduction
The appendiceal mucinous neoplasm (LAMN) is an obstructive dilation of the appendicular lumen with accumulation of mucus, caused more frequently by epithelial proliferation1. It is part of a rare and heterogeneous group of diseases with challenging clinical management decisions. This anomaly represents 0.5-1% of all cancers known and from 0.2% to 0.3% of all appendectomies realized2; however, its incidence is increasing3,4. Its diagnosis represents a challenge since it can manifest as a pelvic mass and in most of the cases it is diagnosed as an acute appendicitis4. Approximately 23-50% of diagnosed patients are asymptomatic, and lesions are discovered incidentally during surgery, radiological evaluations, or endoscopic procedures5. There are currently at least six different diagnostic classifications6, and there is no consensus on which one should be used. Most accepted is the one established in 2010 by the WHO7. In recent years, the name of Appendicular Mucinous Cystic Neoplasm has been accepted, referring to cases such as those mentioned. This entity is divided into two categories; the first one is low-grade neoplasms, for lesions that look like a dilated (sausage-shaped) appendix, which may be associated with a peritoneal pseudomyxoma. The second type is known as mucinous adenocarcinoma or high-grade (conventional) mucinous neoplasm, and its most significant difference is its clinical course and management8,9.
Clinical case
A 45-year-old female patient presented with no significant family history, laparoscopic cholecystectomy 5 years ago without complications, G2, and P2. She went to the emergency department with the presence of colicky abdominal pain (visual analog scale, 9/10) of 48 h of evolution. This pain began in the mesogastrium with subsequent migration to the right iliac fossa and did not yield to the ingestion of butylhioscine. Symptoms such as nausea, diarrhea, non-quantified fever, anorexia, and dysuria were identified. The patient was admitted with the following data: blood pressure 115/70, heart rate 129 beats x’ (bpm), respiratory rate 21 breaths x’ (rpm), temperature 36.9°C, and body mass index 31.3 kg/mt2. On examination: patient calm, Glasgow 15 points. Complaining, afebrile, referring to nausea, with tachycardia 129 bpm, cylindrical neck, mobile, without adenopathy. Rhythmic cardiopulmonary, no rales or other aggregates are heard. Distended abdomen, peristalsis decreased in frequency and intensity, without metallic noises, soft, depressive, painful on mid-palpation in the mesogastrium and right iliac fossa. No masses presence or lymph nodes, psoas +, McBurney +, positive rebound, involuntary positive wall defense with clear evidence of peritoneal irritation. Whole, eutrophic limbs and capillary filling present in 3 sec. Laboratory test were requested where the results showed alterations in the Cell Blood Count: No anemia data, lymphocytes 12.1%, monocytes 9.6%, eosinophils 1%, and neutrophils 11.1 (10 ^ 3/μL), bands 13%, and segmented 65%. No alterations in blood chemistry. Liver function tests with elevation of total bilirubin (1.57 mg/dL), direct bilirubin (0.49 mg/dL), and indirect bilirubin (1.08 mg/dL), aminotransferases in normal values. A multislice tomography study was performed from the diaphragmatic domes to the symphysis pubis (Fig. 1A-C). The study reported an acute appendicular inflammatory process, mild hepatic steatosis, and the absence of a gallbladder with staples in its bed, for which it was decided to enter for venous access placement, hydration, pain management, and surgical protocol.

Figure 1 A: simple coronal section tomography: an image is identified at the level of the right iliac fossa that seems to be dependent of the cecum, with defined edges and heterogeneous inside. B: simple axial slice tomography shows striation of the adjacent fat, without air or free fluid. C: simple axial slice tomography: an image is identified that gives the impression of being dependent on the cecum, with defined edges, and heterogeneous inside. Measures 93.4 × 56.8 mm with a Houndsfield density of 22. May be compatible with an abscess.
Surgical technique
Previous asepsis and antisepsis with patient in supine position under anesthesia. It begins by incising the abdominal wall in the infraumbilical midline and dissection is performed by planes, until it enters the abdominal cavity. Scant free inflammatory fluid was found and a large tumor was observed, approximately 11 × 6 cm in its largest diameter (longitudinal) dependent on the cecum and appendicular region which compromised the ileocecal valve (Fig. 2). The incision was widened to incise Toldt’s fascia and the artery, iliac vein, and right ureter were visualized and preserved. The hepatic flexure was reached and the colon and mesocolon were dissected. The mesocolon was incised until reaching the lesser sac to place the hemostat clamp 15 cm from the ileocecal valve. Both incisions were closed with a negative mechanical maneuver. Ileo-transverse lateral anastomosis was performed in two planes. The right ureter was properly verified, as well as hemostasis, gauze count and complete material. The specimen was sent for histopathological analysis, (hemicolectomy) weighing 590 g. In the site corresponding to the cecal appendix, there was a region with significant dilation, the external surface at this level presented fibrinous and dark brown remains (Fig. 3). After cutting the piece, the mucosa of the ileum was preserved, and it was confirmed that the appendix was the one that presented dilatation with mucinous content, without evident rupture. The portion of union with the cecum presented wall thickening of 1.5 cm. 11 pericolic nodes were dissected. The histopathological report shows the following: ileum (18 cm), colon (9 cm), cecum and appendix (right hemicolectomy) - omentum - compatible with low-grade appendicular mucinous neoplasm (LAMN), with chronic periappendicitis at the site of the injury. Appendix size: 10.0 cm × 5.5 cm × 5.0 cm; wall integrity: intact margins, surgical margins without dysplasia and mucin (Fig. 4). Histopathologic diagnosis was consistent with “low grade appendiceal mucinous neoplasm” with chronic periapendicitis. Chronic and acute inflammation in the omentum was described. Finally, 11 pericolic nodes with reactive sinus and follicular hyperplasia were reported.
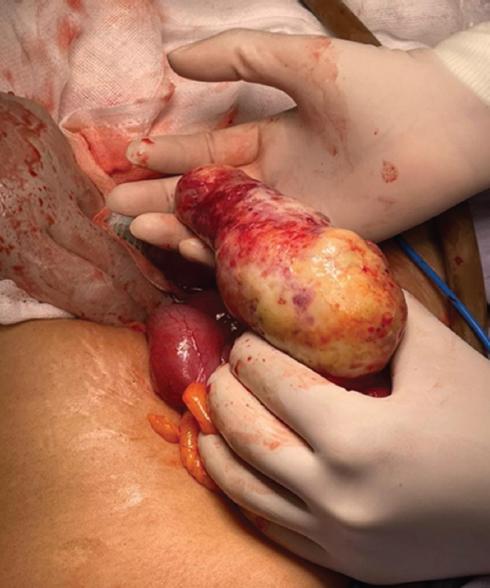
Figure 2 Dependent tumor on the cecal appendix, without the presence of perforation, approximately 12 cm in length, which compromises the ileocecal valve.

Figure 3 Surgical specimen product of a right hemicolectomy, covering approximately 5 cm of the ileum with the presence of a dependent tumor of the cecal appendix.
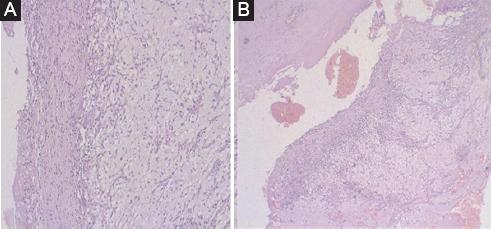
Figure 4 A-B: consistent findings with low-grade appendiceal mucinous neoplasm with chronic periappendicitis site of injury.
The patient was followed up 30 days after discharge, with determination of the carcinoembryonic antigen (CEA) and Ca 19-9 tumor markers, which were at normal values.
Discussion and conclusion
The appendix is an anatomical structure that appears approximately in the 8th week of gestation10 and can be found in different locations among the abdomen and pelvis, thanks to its descent during organogenesis. As various authors reported, the incidence of tumors in this area is minimum, representing 0.4-1.4% among gastrointestinal neoplasms9. Due to its rarity and biological heterogeneity, the guidelines for the primary appendicular tumor are based on scant evidence, which does not generate strong recommendations. In the case presented here, while the tumor mass and part of the omentum were removed, 11 pericolic nodes were removed as well, showing sinus hyperplasia. Hiroshi Takeyama et al. conducted a retrospective study11 that explored factors related to prognosis, including the timing of lymph node dissection. They conclude that lymph node metastasis was an independent prognostic predictor after surgical resection with lymphadenectomy. They also describe that neither the depth of the tumor nor the histological type were predictors of prognosis, but they were predictors of lymph node metastasis12. We have also agreed on the frequency by gender, which, according to other authors, occurs mostly in women. However, we could differ from the age established as risk (sixth decade of life), since our patient was 45-years-old, so the possibility of presenting this pathology at younger ages should be considered. Although we know that the pathology is rare, in the last decade we have verified its appearance in an increasingly younger population13. Therefore, it is recommended to suspect its existence, as well as to document the cases in subsequent studies.
It is considered of utmost importance to know with certainty the existence or not of extra-appendicular neoplastic epithelium. Thus, the histopathological study becomes of vital importance for the detection of tumor cells, their histological type, the margins of resection free of malignant cells, the basal or distal involvement of the appendix and the size of the tumor. This includes its invasion in the different layers of the organ, when determining the definitive therapy. In the case of our patient, it was a LAMN with free edges whose conduct required surgical extraction and its follow-up with tumor markers.
The clinical implication of these neoplasms is the subsequent development of peritoneal pseudomyxoma14. Appendix tumors are extremely rare and, although they have been increasing, their frequency remains low; because of this they are often incidental findings. Its diagnosis is difficult due to the non-specificity of the symptoms. The imaging test of choice is computed tomography and, it should be noted, that it is important to perform it due to its usefulness at detecting the presence of localized peritoneal pseudomyxoma.











 text new page (beta)
text new page (beta)


