Introduction
Cerebrovascular disease has been identified as part of the COVID-19 spectrum. Ischemic stroke has been reported in almost 5% of cases, cerebral venous thrombosis in 0.5%, and hemorrhagic stroke (HS) in 0.5%1-3. Debate has emerged between whether there is a casual or causal relationship between HS and SARS-CoV-2 infection. Due to the history of other pandemic coronaviruses, where the increased risk of stroke was demonstrated; etiopathogenic mechanisms of the virus, the human-induced immune response, and neurotropism, COVID-19 is postulated at least as a triggering factor for HS in a risk patient4-7.
In our practice during the SARS-CoV-2 pandemic, we have identified two different patterns of presentation of HS associated to COVID-19. The first pattern, patients who assisted to an emergency room (ER) with pulmonary symptoms and later develop HS, and a second pattern, patients who begin with neurological symptoms and as part of their approach the SARS-CoV-2 infection was identified, developing or not pulmonary symptoms later. Therefore, our objective is to know the differential characteristics associated with each of these presentation patterns.
Methods
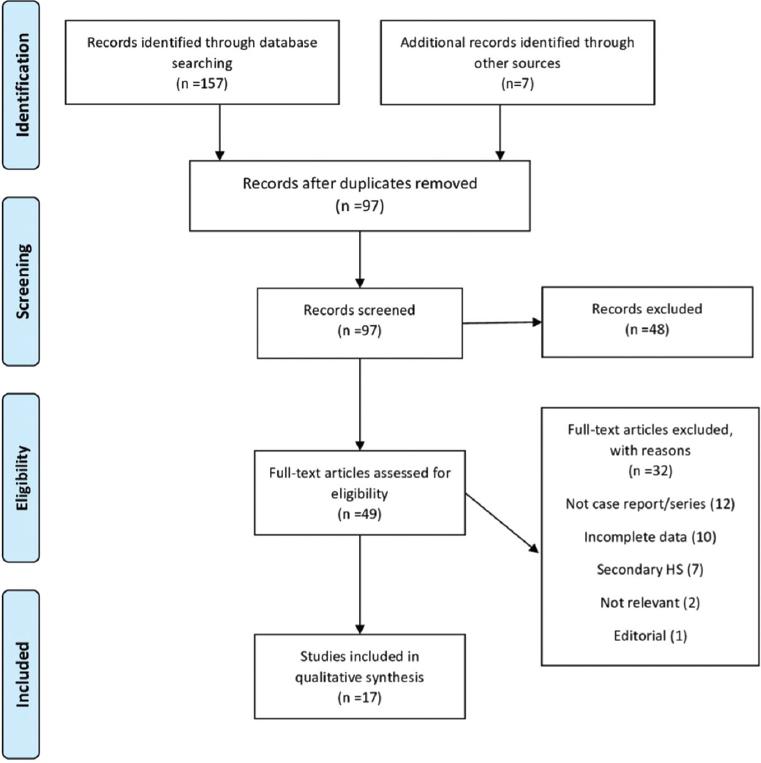
We performed a rapid systematic review based on PRISMA guidelines8 through an exhaustive search in PUBMED of human case series or case reports available up to January 20, 2021, with the English terms: <<COVID-19>> OR <<SARS-CoV-2>> AND <<intracranial hemorrhage>> OR <<hemorrhagic stroke>> separated or in association. PUBMED function “related articles” was used to optimize the search. We included those studies with patients with confirmatory reverse transcription-polymerase chain reaction test for SARS-CoV-2 and who had evidence by computerized axial tomography scan of the skull of HS during their hospitalization. Patients with underlying structural causes (tumors, vascular malformation, and aneurysms), and with history of trauma, or if they were under extracorporeal membrane oxygenation due to the severity of the COVID-19 pneumonia were not considered for the present analysis considering all these secondary etiologies.
From our literature search, we identified 57 patients from 17 registries that met the inclusion criteria9-25. To this sample, we added 13 patients from our own cohort. From March 23, 2020, to January 20, 2021, 2418 patients with COVID-19 had been hospitalized in our center. During this period, the neurosurgery department was assigned to urgent neurosurgical procedures and to solve potential neurosurgical complications for COVID-19 patients.
For the purposes of this report, it was obtained demographic data, clinical characteristics, laboratory, and image results of patients, as well as their evolution. To determine differences between presentation patterns, we divided patients in two groups: respiratory symptoms onset or neurologic symptoms onset. IBM SPSS Statistics 24 software was used for all results in this report. Analyses of differences between categorical variables were performed with the Chi-square test. Student t-test was used for the comparison of parametric quantitative variables for independent groups. We perform a generalized linear model (GLM) for random factors to homogenize the values from different sources. p < 0.05 was considered statistically significant. All analyses were two-tailed. All values are shown as mean ± standard deviation (SD). The Local Ethical Committee approved the conducting of this study.
Results
Study identification and screening
We found 164 records. After a first screen based on title, 67 records appeared to be duplicated and were excluded from the study. Later, applying the inclusion criteria, 49 full-text articles were selected and finally, due to lack of data, study design, or a secondary cause of HS 32 articles were excluded from the study. Only 57 cases that met all the inclusion criteria from 17 records were considered for final analysis. Ten studies were from United States of America, two from China, and one from United Kingdom, Iran, Brazil, Korea, and Spain each. We found ten case reports and seven case series (Fig. 1).
Baseline characteristics
Seventy patients with HS associated to COVID-19 were pooled for the present analysis. Patients presented to ER with pulmonary symptoms in 68.6% of the cases. The average duration between the onset of COVID-19 symptoms and the cerebrovascular insult was 15.6 days (SD = 9.5). In the other group, 31.4% of patients presented with neurologic symptoms. Most patients were men 63.5% (Table 1).
Table 1 Baseline characteristics cataloged by presentation patterns
| Total | Pulmonary symptoms | Neurologic symptoms | p value | |
|---|---|---|---|---|
| Number of patients | 70 | 48 (68.6%) | 22 (31.4%) | |
| Men, % | 63.5 | 63.6 | 63.2 | 0.60 |
| Age, year, mean (SD) | 59 (13.9) | 59 (11.4) | 61 (18.6) | 0.62 |
| Diabetes, n (%) | 29 (41.4) | 19 (39.6) | 10 (45.5) | 0.41 |
| Hypertension, n (%) | 45 (64.3) | 30 (64.6) | 13 (63.6) | 0.57 |
| Hyperlipidemia, n (%) | 21 (30.0) | 17 (35.4) | 4 (18.2) | 0.11 |
| Smoking, n (%) | 10 (14.3) | 6 (12.5) | 4 (18.2) | 0.38 |
| Obesity, n (%) | 10 (14.3) | 8 (16.7) | 2 (9.1) | 0.33 |
| Atrial fibrillation, n (%) | 4 (5.7) | 3 (6.3) | 1 (4.5) | 0.63 |
| Prior anticoagulant use, n (%) | 3 (4.3) | 1 (2.1) | 2 (9.1) | 0.23 |
| Anticoagulant use during hospitalization, n (%) | 37 (52.9) | 37 (77.1) | 0 | 0.00 |
| Hypertension during hospitalization, n (%) | 24 (34.3) | 13 (27.1) | 11 (50) | 0.05 |
Regarding the history of vascular risk factors, there were not significant differences between the groups. The use of anticoagulants was associated with HS in patients with pulmonary symptoms as it was indicated in 77.1%, while hypertension during hospitalization was more frequent in the group of neurological symptoms (p < 0.05) (Table 1).
Laboratory and imaging characteristics
Almost all the strokes were lobar intracerebral (n = 67), followed by subarachnoid hemorrhage and in only two cases subdural hematomas. In respect to location, frontal (n = 8) and parietal (n = 5) lobar hemorrhages were the most frequent, followed by deep supratentorial location with 17 cases in basal ganglia (24.3%). Interestingly, multifocal location was significantly associated with the group of pulmonary symptoms (p < 0.05), while the infratentorial location (dentate nucleus n = 10 and brainstem n = 4) was more frequent in the group of neurological symptoms (31.8% vs. 14.6%) but without statistical significance (p = 0.09). Ventricular irruption and typical location of hypertensive HS were more frequent in the group of neurological symptoms than in the group of pulmonary symptoms, 59.1% versus 39.6% and 63.6% versus 43.8%, respectively (Table 2) (Figs. 2 and 3).
Table 2 Hemorrhagic stroke imaging characteristics and outcome stratified by presentation patterns
| Total | Pulmonary symptoms | Neurologic symptoms | p value | |
|---|---|---|---|---|
| ICH location | ||||
| Lobar, n (%) | 24 (34.3) | 18 (37.5) | 6 (27.3) | 0.28 |
| Deep supratentorial, n (%) | 23 (32.9) | 14 (29.2) | 9 (40.9) | 0.24 |
| Infratentorial, n (%) | 14 (20) | 7 (14.6) | 7 (31.8) | 0.09 |
| Multifocal, n (%) | 9 (12.9) | 9 (18.8) | 0 | 0.02 |
| CT findings | ||||
| Intracerebral hemorrhage, n (%) | 67 (95.7) | 45 (93.8) | 22 (100) | 0.31 |
| Subarachnoid hemorrhage, n (%) | 22 (31.4) | 18 (37.5) | 4 (18.2) | 0.08 |
| Subdural hematoma, n (%) | 2 (2.9) | 2 (4.2) | 0 | 0.46 |
| Ventricular irruption, n (%) | 32 (45.7) | 19 (39.6) | 13 (59.1) | 0.07 |
| Hypertensive location, n (%) | 35 (50) | 21 (43.8) | 14 (63.6) | 0.09 |
| Glasgow outcome scale (GOS) | ||||
| GOS 1, n (%) | 41 (58.6) | 29 (60.4) | 12 (54.5) | 0.41 |
| GOS 2, n (%) | 5 (7.1) | 5 (10.4) | 0 | 0.14 |
| GOS 3, n (%) | 8 (11.4) | 1 (2.1) | 7 (31.8) | 0.01 |
| GOS 4, n (%) | 11 (15.2) | 8 (16.7) | 3 (13.6) | 0.52 |
| GOS 5, n (%) | 5 (7.1) | 5 (10.4) | 0 | 0.14 |

Figure 2 Illustrative cases of hemorrhagic stroke associated to COVID-19 in our center that debuted with neurological symptoms. A-D: brain-computerized axial tomography (CT) of a patient with left thalamic hemorrhage and ground-glass pattern in chest CT. E-H: brain CT of a patient with a brainstem hemorrhage and ground-glass pattern in chest radiography I-L: brain CT showing a massive deep lobar hemorrhage with ventricular irruption and ground-glass opacity in subpleural areal in lung CT

Figure 3 Illustrative cases of hemorrhagic stroke associated to COVID-19 in our center that debuted with pulmonary symptoms. A-D: brain-computerized axial tomography (CT) of a patient with right thalamic hemorrhage and consolidation areas in chest CT. E-H: brain CT of a patient with a deep seated hemorrhage and ground-glass pattern in chest radiography. I-L: brain CT showing a massive deep cerebellar right hemorrhage with brainstem infarction and secondary obstructive hydrocephalus; subpleural effusion; and consolidation in chest CT
Levels of D-dimer, Ferritin, and lactate dehydrogenase (LDH) were significantly higher in the group of patients with pulmonary symptoms both in the univariate and GLM analysis.
Elevated hemoglobin level was higher it the group with neurological symptoms (p < 0.05) (Table 3).
Table 3 Laboratory findings in hemorrhagic stroke COVID-19 patients
| Total | Pulmonary symptoms | Neurologic symptoms | p value UA | p value GLM | |
|---|---|---|---|---|---|
| Platelets, × 103/uL, mean (SD) | 222 (124) | 231 (133) | 201 (99) | 0.38 | 0.49 |
| Hemoglobin, g/dL, mean (SD) | 11.5 (2.84) | 10.8 (2.9) | 13.1 (1.7) | 0.02 | 0.40 |
| White blood cells, × 103/uL, mean (SD) | 12.1 (6.44) | 12.1 (6.1) | 11.9 (7.1) | 0.90 | 0.43 |
| C-reactive protein, mg/L, mean (SD) | 93.8 (95.6) | 96.8 (99.9) | 85.6 (85.8) | 0.67 | 0.33 |
| D-dimer, ug/mL, mean (SD) | 9021 (12284) | 13570 (11711) | 3822 (11531) | 0.05 | 0.00 |
| Ferritin, ng/mL, mean (SD) | 803 (974) | 1182 (1070) | 184 (179) | 0.00 | 0.00 |
| Lactate dehydrogenase, U/L, mean (SD) | 406 (288) | 582 (220) | 205 (223) | 0.01 | 0.00 |
| International normalized ratio, mean (SD) | 1.59 (1.12) | 1.69 (1.00) | 1.48 (1.31) | 0.36 | 0.09 |
| Partial thromboplastin time, s, mean (SD) | 41.7 (37.4) | 45.2 (40.9) | 33.1 (26) | 0.17 | 0.19 |
UA represents the p value of univariate analysis and GLM the p value of general linear model. SD: standard deviation, GLM: generalized linear model
Outcome
Most of the patients with HS associated with COVID-19 had a poor prognosis (77.1%), being higher in the group that debuted with neurological symptoms (86%). Overall mortality was 58.6% with no significant differences between groups (Table 2).
Discussion
In this retrospective analysis of patients with HS associated to COVID-19 reported in the world literature, we found interesting differences in radiological and laboratory tests when separated by presentation pattern, this may indirectly imply different, but known, etiopathogenic mechanisms.
Previous HS associated with COVID-19 retrospective analysis, report 11-41% (1.26-29) of patients who presented with neurological symptoms; in our review, it was 31.4%. This leads us to the recommendation for clinicians to raise the suspicion of COVID-19 in a patient with apparently unidentified cause of HS, as part of the approach, to prioritize the care of these patients, and to protect medical team.
Regarding the differences that we found in association with the group of neurological symptoms, the presence of hypertension during hospitalization and the subsequent finding of typical location of hypertensive hemorrhage (putamen, caudate nucleus, thalamus, and dentate nucleus) stands out. It can be inferred that the main mechanism of HS in patients with COVID-19 who present with neurological symptoms could be related to a hypertensive crisis. This phenomenon could be explained at the beginning of the disease and before developing pulmonary symptoms due to the trophism of SARS-CoV-2 by endothelial cells that express the angiotensin converting enzyme 2 (ACE2) receptor4,30,31. The loss of ACE2 receptors, due to the entry of the virus, leads to a dysregulation of the Renin-Angiotensin system through an increase in circulating angiotensin II (vasoconstriction, pro-inflammatory, and profibrotic) without the counterbalance of the angiotensin 1-7 pathway (vasodilation, anti-inflammatory, and antifibrotic) and consequently increased vasoconstriction, renal reabsorption of sodium, and water with the consequent increase in blood pressure32-35.
In the group of patients with pulmonary symptoms, we found a significant association with the use of anticoagulants during hospitalization, multifocal location, and elevated levels of D-dimer, ferritin, and LDH. This leads us to assume various pathophysiological mechanisms that may contribute to the development of HS. Anticoagulant use is a well-known predisposing factor for the development of HS. A recent study by Melmed et al. found 5-fold increased risk of HS in COVID-19 patients36. Given that thrombotic events in patients with COVID-19 are common, the use of anticoagulants has almost always been indicated based on D-dimer levels as prophylaxis; however, the individual risk of HS must be weighed when starting treatment18,28,37,38.
Acute-phase reactants (C-reactive protein, ferritin, LDH, and D-dimer) reflect the inflammatory response in the context of infectious diseases, including SARS-CoV-2 infection31,39. Uncontrolled immune response-mediated by interleukin (IL)-6 and IL-8 leads to a cytokine storm responsible for activation of matrix metalloproteinases that degrade components of vascular wall increasing risk of rupture and bleeding26,31,40. D-dimer that reflects the activity of the coagulation and fibrinolytic systems has been previously described as a major risk factor for intracranial hemorrhage and death, also some microthrombi can cause hypoxia and local necrosis in the vessel walls, increasing the risk of bleeding41,42. Elevated ferritin has been associated with severity and poor functional outcome in HS patients, presumably by overregulating secondary brain damage increasing perihematomal edema43,44. The fact that these processes occur in the microvascular environment could also favor the multifocal location. It has been previously shown that critically ill patients may be predisposed to HS, due to hypoxia, disseminated intravascular coagulation, sepsis, and among others, but these mechanisms could not be explored in the present study21,36. Results of this review are consistent with the previous studies in patients with COVID-19, in which a significant decrease in hemoglobin levels has been found, especially in those critically ill. It has been postulated that it could be related to the inhibition of hematopoiesis in the bone marrow or by hemophagocytosis within the pulmonary hilum or lymph nodes; however, there are insufficient data to support these theories45-47.
Mortality was 58.6%, which is higher than retrospective studies carried out in this regard, Nawabi et al. 44%27, Melmed 51.5%36, and Dogra et al. 42.4%28, this could be easily explained by the different inclusion criteria. Although we did not find differences between groups regarding mortality, the patients who debuted with neurological symptoms had a worse outcome (Glasgow outcome scale [GOS] 1-3) percentage 72.9% versus 86.3%.
This study has multiple limitations, the main ones being the heterogeneity of the information as it is based on multiple case reports and cohort studies with different approach and treatments according to each, in addition to its retrospective nature. On the other hand, to the best of our knowledge, it is the first to explore the differences between the presentation patterns of HS associated with COVID-19. We hope that in the future, other centers with experience will be able to prospectively explore these differences to consolidate our observations.
Conclusion
Although HS associated with COVID-19 is a clinical entity with increasing evidence, it is necessary to establish that there are two forms of presentation with their own characteristics; the one that begins with neurological symptoms that seems to be related to hypertension and the one that begins with pulmonary symptoms that late, in the context of a critically ill patient with anticoagulation and with an altered immune response can develop HS through mechanisms different to hypertension. HS should be considered as differential diagnosis in cases of neurological impairment in a previous stable patient and should prepare neurosurgery teams around the world for the timely and appropriate treatment of HS COVID-19 patients.











 text new page (beta)
text new page (beta)