Introduction
The majority of global blindness and moderate and severe visual impairment is found in women, who are at a higher risk of cataract blindness than men1,2. Women have a longer life expectancy than men, so their risk of developing cataract is greater, and the prevalence of cataract blindness in women can be double of that of men in developing countries3-6. The degree to which cataract surgical services meet the needs of the population is measured by the global eye health indicator, cataract surgical coverage (CSC), defined as the proportion of people with bilateral cataract eligible for cataract surgery (at 3/60 and 6/18 level, equivalent to 20/400 and 20/60 levels, respectively) who have been operated on in at least 1 eye6.
Unfortunately, global data demonstrate gender inequity in CSC in low- and middle-income countries, with less women undergoing cataract surgery than men7-9. Not only is there inequality in CSC among women and men, but women tend to have worse postoperative visual outcomes, compared to men.9 The reasons for the inequity in CSC may be attributed to gender-defined roles in patriarchal societies (such as when women have less control over finances and less disposable income then men), costs, the need to travel far to access surgery, and lack of awareness7,10-13.
Health inequities in Latin America are among the greatest in the world14,15. However, gender inequity does not appear to be an issue for eye health in Latin America. The prevalence of blindness in men and women is the same for the age group 50 years and older (1.6%) and for all ages (0.4%)16. A 2012 meta-analysis using a random effects model evaluated CSC data from 11 epidemiological studies in 11 Latin American countries and did not find gender inequity existed in terms of receiving cataract surgery17. A similar finding was reported in an assessment of CSC in 7 recent Latin American studies14. We performed an updated meta-analysis of CSC data reported in Latin American epidemiological studies since 2011 to confirm that gender equity exists in terms of receiving cataract surgery in the region.
Materials and methods
This meta-analysis study adhered to the Declaration of Helsinki and was not approved by an Institutional Review Board, because the retrospective data extracted from the literature only existed in deidentified format.
Study selection
Earlier ophthalmic epidemiological studies used the Rapid Assessment of Cataract Surgical Services (RACSS) methodology, but this methodology was updated and became the Rapid Assessment of Avoidable Blindness (RAAB) methodology, which is now the preferred standardized methodology to collect CSC data6,18,19. Because study designs must be similar with comparable outcomes for pooling data in meta-analysis,17 and RACSS studies are no longer performed, we searched for new RAAB studies for inclusion in this updated meta-analysis. Therefore, an updated literature search was performed on PubMed to identify any new RAAB studies from Latin American countries that were published from January 1, 2011 through September 2, 2019. The search terms employed were “RAAB”, “Rapid Assessment of Avoidable Blindness”, “ERCE”, and “Evaluación Rápida de Ceguera Evitable” in combination with “Argentina”, “Bolivia”, “Brazil”, “Brasil”, “Chile”, “Colombia”, “Costa Rica”, “Cuba”, “Dominican Republic”, “la República Dominicana”, “Ecuador”, “El Salvador”, “Guatemala”, “Honduras”, “Mexico”, “México”, “Nicaragua”, “Panama”, “Panamá”, “Paraguay”, “Peru”, “Perú”, “Uruguay”, and “Venezuela”. We also searched the RAAB Repository (http://raabdata.info/repository/), a public online database of RAAB studies, where study authors have the option to upload RAAB data, study reports, and related publications. We combed through RAAB studies for age and sex-reported CSC data for individual men and women for pinhole visual acuity (VA) at 3/60 and 6/18 and at <20/400 and 20/60.
After selecting the new RAAB studies for analysis, we next selected older studies (published before 2011) analyzed in the previous meta-analysis17 for inclusion in the updated meta-analysis. Any RAAB or RACSS study that was published through December 31, 2010 and based in a Latin American country that did not have a newer study with newer data published after December 2010 was included in the updated meta-analysis.
Data extraction and calculations
Summary-level CSC data for individuals only were extracted from all eligible studies using visual acuity levels of 3/60 (equivalent to 20/400) and 6/18 (equivalent to 20/60). For the purposes of analysis, we used the metric VA levels of 30/60 and 6/18. Calculations and assumptions followed the previous meta-analysis, with the exception that intraclass correlation coefficient (ICC; to determine the probability that, if one eye had cataract, the other eye would develop cataract) was not done, because the results of the previous meta-analysis strongly demonstrated that eye correlation in Latin America was not an issue, with the ICC <3.0.17 The DE was set to 1.6 for x, y, and z factors. The x values were calculated by solving for x in the following equation: CSC (%) = (x + y)/(x + y + z) *100. where x = number of persons with 1 operated and 1 visually impaired eye due to cataract, y = number of persons with bilateral (pseudo)aphakia, and z = number of persons bilaterally visually impaired by cataract (pinhole VA<3/60 or <6/18).
Meta-analysis
The numerators and denominators used in the meta-analysis were the same as those calculated for the CSC, representing both a CSC rate and a probability that a person received cataract surgery. Men and women were the comparator groups for each study. In the event a country had data from multiple, regional studies (as opposed to data from 1 national survey), data from the regional studies were pooled for data entry. A random effects model was chosen for meta-analysis to account for some heterogeneity between studies with respect to variation in geographic region and demographics. To be able to compare between studies, the effect measure was odds ratio (OR).
The data were analyzed using Medcalc software (19.0.3; Ostend, Belgium) to calculate the OR, 95% confidence intervals (CIs), and p values using a random effects model. Meta-analysis was done for all studies published since 2011 and for all eligible studies included at VAs of <3/60 and <6/18. The I2 (inconsistency) statistic and the Cochran Q statistic estimated the statistical heterogeneity17.
Results
Sixteen RAAB publications were extracted from the literature search; 4 were excluded for being reviews, resulting in 12 new RAAB publications and their study reports included in the meta-analysis20-44. A 2014 national RAAB survey in Bolivia45 and a 2016 nationwide RAAB survey in Cuba were also listed on the RAAB Repository; however, the Cuban study was excluded from this analysis because the data were not published in the repository and are not available. The Guatemala article had insufficient data, and the study reported was not available to download on the RAAB Repository; thus, a study author was contacted who provided the study report (Personal E-mail Communication, Furtado JF, September, 3, 2019). Therefore, 13 new RAAB studies were included in this analysis. Among the new studies, there were 3 Mexican studies conducted in 3 different states;25-27, 38-40 data from these 3 studies were pooled for meta-analysis.
Three older RACSS studies46-48 and 3 RAAB studies49-51 that were included in the previous meta-analysis were also included in the updated meta-analysis, because they were in countries that have not had new RAAB data released since 2011. Therefore, a total of 19 studies from 17 countries were included in the updated meta-analysis (Table 1). Thirteen studies were national RAAB surveys. The sample size among the studies varied widely from 1,132 persons in Bolivia to 6,300 in Queretaro, Mexico. Coverage also varied from 76.6% in Costa Rica to 97.7% in Guatemala. The CSC for persons with cataract blindness (VA <3/60) varied drastically from 29.5% in Guatemala to 97.1% in Argentina.
Table 1 Study characteristics. All studies were Rapid Assessments of Avoidable Blindness, unless otherwise identified by an asterisk (*) as a Rapid Assessment of Cataract Surgical Services
| Country | Study Year | Location, Type | Sample Size | Survey Coverage | CSC<3/60, for All Persons | CSC<6/60, for All Persons |
|---|---|---|---|---|---|---|
| Argentina20,32 | 2013 | National | 4,100 | 92.0% | 97.1% | 83.7% |
| Brazil | ||||||
| São Paulo46* | 2003 | Regional, urban | 2,224 | 92.7% | 88.9% | 82.2% |
| Bolivia45 | 2015 | National | 1,132 | 95.9% | 57.1% | 51.2% |
| Chile | ||||||
| Region VI49 | 2006 | Regional, urban and rural | 3,000 | 97.2% | 75.8% | 71.0% |
| Costa Rica21,33,34 | 2015 | National | 3,255 | 76.6% | 88.9% | 76.6% |
| Cuba | ||||||
| Havana48* | 2004 | Regional, urban | 2,760 | 98.4% | 73.0% | 65.0% |
| Dominican Republic51 | 2008 | National | 3,873 | 96.9% | 62.5% | 50.3% |
| Ecuador50 | 2009 | National | 4,012 | 95.5% | 82.3% | 62.4% |
| El Salvador22,35 | 2011 | National | 3,800 | 89.4% | 59.1% | 43.6% |
| Guatemala23 | 2015 | National | 3,850 | 97.7% | 29.5% | 17.4% |
| Honduras24 | 2013 | National | 3,150 | 95.2% | 75.2% | 66.5% |
| Mexico | ||||||
| Chiapas25 | 2010 | Regional, urban and rural | 3,300 | 87% | 69% | 63.% |
| Nuevo Leon26 | 2014 | Regional, urban and rural | 5,460 | 92.6% | 85.2% | 68.2% |
| Queretaro27 | 2015 | Regional, urban and rural | 6,300 | 94.2% | 91.7% | 78.5% |
| Panama28 | 2014 | National | 4,200 | 98.2% | 66.8% | 59.2% |
| Paraguay29 | 2011 | National | 3,000 | 95.4% | 90% | 78% |
| Peru30 | 2011 | National | 5,000 | 97.0% | 66.9% | 57.4% |
| Uruguay31 | 2011 | National | 3,956 | 94.3% | 91.3% | 86.0% |
| Venezuela47* | 2004 | National | 3,317 | 97.6% | 70.2% | 58.75% |
CSC=cataract surgical coverage
For CSC rates on an individual basis from studies published since 2011, the ORs at a VA of <3/60 and <6/18 were not statistically significant at 0.99 (95% CI: 0.74-1.33) and 1.07 (0.90-1.26), respectively (Tables 2 and 3 and Figures 1 and 2). There was no heterogeneity encountered among studies. Therefore, in Latin American RAAB studies published since 2011, there were no significant differences between men and women in terms of CSC at any VA level.
Table 2 Results of meta-analysis for odds ratio obtaining cataract surgery for individuals at a pinhole visual acuity of < 3/60 from studies published since 2011
| Study (-ies) | Women | Men | Weight | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| Events | Total | Events | Total | |||
| Argentina20,32 | 72 | 74 | 58 | 60 | 2.4% | 1.24 (0.17-9.08) |
| Bolivia45 | 8 | 16 | 4 | 6 | 2.5% | 0.50 (0.07-3.55) |
| Costa Rica21,33,34 | 56 | 63 | 28 | 33 | 6.2% | 1.43 (0.42-4.91) |
| El Salvador22,35 | 24 | 41 | 26 | 44 | 12.7% | 0.98 (0.41-2.32) |
| Guatemala23,36 | 14 | 46 | 9 | 30 | 8.7% | 1.02 (0.38-2.78) |
| Honduras24,37 | 34 | 49 | 26 | 36 | 10.6% | 0.87 (0.34-2.25) |
| Mexico25-27,38-40 | 135 | 162 | 146 | 166 | 24.5% | 0.69 (0.37-1.28) |
| Panama28,41 | 76 | 96 | 79 | 107 | 22.2% | 1.35 (0.70-2.59) |
| Paraguay29,42 | 22 | 24 | 20 | 23 | 2.7% | 1.65 (0.25-10.91) |
| Peru30,43 | 34 | 52 | 24 | 39 | 12.8% | 1.18 (0.50-2.80) |
| Uruguay31,44 | 49 | 55 | 27 | 29 | 3.4% | 0.61 (0.11-3.21) |
| Total | 524 | 678 | 447 | 573 | 100.0% | 0.99 (0.74-1.33) |
CI = Confidence Interval
Heterogeneity: Q = 3.89; df = 10 (P = 0.95); I2 (95% CI) = 0.0% (0.00-0.00)
Test for overall random effect: Z = -0.088 (P = 0.93).
Table 3 Results of meta-analysis for odds ratio obtaining cataract surgery for individuals at a pinhole visual acuity of<6/18 from studies published since 2011
| Study (-ies) | Women | Men | Weight | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| Events | Total | Events | Total | |||
| Argentina20,32 | 98 | 137 | 59 | 91 | 9.4% | 1.36 (0.72-2.41) |
| Bolivia45 | 10 | 27 | 4 | 10 | 1.4% | 0.88 (0.20-3.90) |
| Costa Rica21,33,34 | 64 | 116 | 34 | 67 | 8.4% | 1.2 (0.65-2.18) |
| El Salvador22,35 | 29 | 106 | 33 | 111 | 8.8% | 0.89 (0.49-1.61) |
| Guatemala23,36 | 20 | 189 | 13 | 175 | 5.4% | 1.48 (0.71-3.06) |
| Honduras24,37 | 40 | 99 | 30 | 78 | 8.3% | 1.09 (0.59-1.99) |
| Mexico25-27,38-40 | 151 | 265 | 158 | 250 | 24.4% | 0.77 (0.54-1.10) |
| Panama28,41 | 100 | 179 | 98 | 197 | 18.5% | 1.28 (0.85-1.92) |
| Paraguay29,42 | 27 | 41 | 23 | 43 | 3.9% | 1.68 (0.70-4.05) |
| Peru30,43 | 41 | 102 | 31 | 93 | 8.9% | 1.34 (0.75-2.41) |
| Uruguay31,44 | 55 | 117 | 34 | 63 | 8.1% | 0.76 (0.41-1.40) |
| Total | 635 | 1,378 | 517 | 1,178 | 100.0% | 1.07 (0.90-1.26) |
CI = Confidence Interval
Heterogeneity: Q = 8.84; df = 10 (P = 0.55); I2 (95% CI) = 0.0% (0.0-55.2)
Test for overall random effect: Z = 0.74 (P = 0.46).
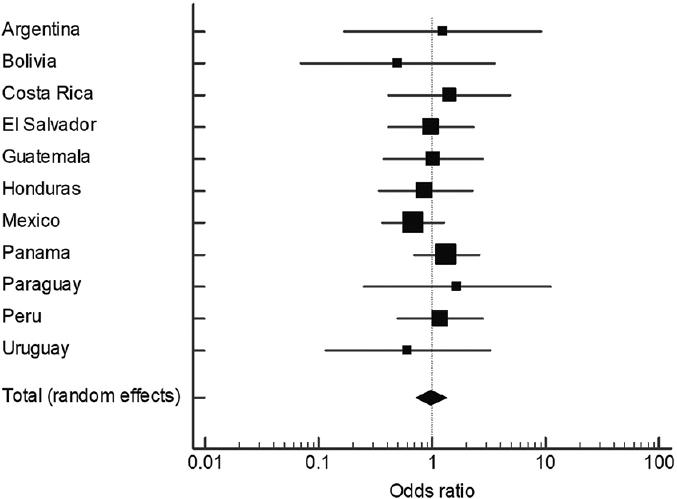
Figure 1 Forest plot of odds ratio (OR) of obtaining cataract surgery for individuals at a pinhole visual acuity of <3/60 from studies published since 2011. ORs <l mean women have worse cataract surgical coverage (CSC), and ORs >1 mean that women have better CSC, compared to men.
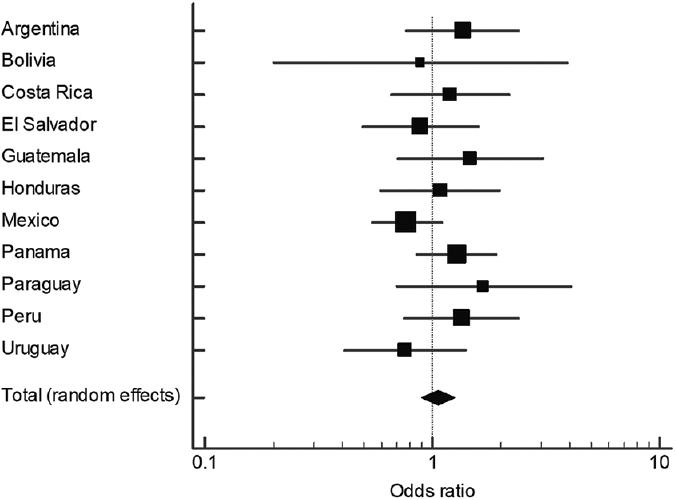
Figure 2 Forest plot of odds ratio (OR) of obtaining cataract surgery for individuals at a pinhole visual acuity of <6/18 from studies published since 2011. ORs <l mean women have worse cataract surgical coverage (CSC), and ORs >1 mean that women have better CSC, compared to men.
Meta-analysis results for all eligible studies included were similar to those of more recent studies, with non-statistically significant ORs at a VA of <3/60 and <6/18 of 1.04 (95% CI: 0.82-1.32) and 1.04 (95% CI: 0.90-1.19), respectively (Tables 4 and 5 and Figures 3 and 4). Again, there was no heterogeneity. Thus, in all RAAB and RACSS studies analyzed, there were no significant differences between men and women in terms of CSC at any VA level.
Table 4 Results of meta-analysis for odds ratio obtaining cataract surgery for individuals at a pinhole visual acuity of < 3/60 from all studies included for analysis
| Study (-ies) | Women | Men | Weight | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| Events | Total | Events | Total | |||
| Argentina20,32 | 72 | 74 | 58 | 60 | 2.4% | 1.24 (0.17-9.08) |
| Bolivia45 | 8 | 16 | 4 | 6 | 2.5% | 0.50 (0.07-3.55) |
| Costa Rica21,33,34 | 56 | 63 | 28 | 33 | 6.2% | 1.43 (0.42-4.91) |
| El Salvador22,35 | 24 | 41 | 26 | 44 | 12.7% | 0.98 (0.41-2.32) |
| Guatemala23,36 | 14 | 46 | 9 | 30 | 8.7% | 1.02 (0.38-2.78) |
| Honduras24,37 | 34 | 49 | 26 | 36 | 10.6% | 0.87 (0.34-2.25) |
| Mexico25-27,38-40 | 135 | 162 | 146 | 166 | 24.5% | 0.69 (0.37-1.28) |
| Panama28,41 | 76 | 96 | 79 | 107 | 22.2% | 1.35 (0.70-2.59) |
| Paraguay29,42 | 22 | 24 | 20 | 23 | 2.7% | 1.65 (0.25-10.91) |
| Peru30,43 | 34 | 52 | 24 | 39 | 12.8% | 1.18 (0.50-2.80) |
| Uruguay31,44 | 49 | 55 | 27 | 29 | 3.4% | 0.61 (0.11-3.21) |
| Total | 524 | 678 | 447 | 573 | 100.0% | 0.99 (0.74-1.33) |
CI = Confidence Interval
Heterogeneity: Q = 3.89; df = 10 (P = 0.95); I2 (95% CI) = 0.0% (0.00-0.00)
Test for overall random effect: Z = -0.088 (P = 0.93).
Table 5 Results of meta-analysis for odds ratio obtaining cataract surgery for individuals at a pinhole visual acuity of<6/18 from all studies included in analysis
| Study (-ies) | Women | Men | Weight | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| Events | Total | Events | Total | |||
| Argentina20,32 | 98 | 137 | 59 | 91 | 5.9% | 1.36 (0.72-2.41) |
| Bolivia45 | 10 | 27 | 4 | 10 | 0.9% | 0.88 (0.20-3.90) |
| Brazil46 | 52 | 70 | 42 | 51 | 2.4% | 0.62 (0.25-1.52) |
| Chile49 | 35 | 73 | 18 | 48 | 3.5% | 1.54 (0.73-3.23) |
| Costa Rica21,33,34 | 64 | 116 | 34 | 67 | 5.3% | 1.2 (0.65-2.18) |
| Cuba48 | 53 | 145 | 45 | 105 | 7.3% | 0.77 (0.46-1.28) |
| Dominican Republic51 | 28 | 108 | 30 | 102 | 5.2% | 0.84 (0.46-1.54) |
| Ecuador50 | 85 | 183 | 81 | 184 | 11.3% | 1.10 (0.73-1.66) |
| El Salvador22,35 | 29 | 106 | 33 | 111 | 5.5% | 0.89 (0.49-1.61) |
| Guatemala23,36 | 20 | 189 | 13 | 175 | 3.6% | 1.48 (0.71-3.06) |
| Honduras24,37 | 40 | 99 | 30 | 78 | 5.2% | 1.09 (0.59-1.99) |
| Mexico25-27,38-40 | 151 | 265 | 158 | 250 | 15.3% | 0.77 (0.54-1.10) |
| Panama28,41 | 100 | 179 | 98 | 197 | 11.6% | 1.28 (0.85-1.92) |
| Paraguay29,42 | 27 | 41 | 23 | 43 | 2.5% | 1.68 (0.70-4.05) |
| Peru30,43 | 41 | 102 | 31 | 93 | 5.6% | 1.34 (0.75-2.41) |
| Uruguay31,44 | 55 | 117 | 34 | 63 | 5.1% | 0.76 (0.41-1.40) |
| Venezuela47 | 43 | 80 | 25 | 51 | 3.9% | 1.21 (0.60-2.44) |
| Total | 931 | 2,037 | 758 | 1,719 | 100.0% | 1.04 (0.90-1.19) |
CI = Confidence Interval
Heterogeneity: Q = 13.32; df = 16 (P = 0.65); I2 (95% CI) = 0.0% (0.0-41.33)
Test for overall random effect: Z = 0.51 (P = 0.61).
Discussion
Overall, the results of this updated meta-analysis for both the most recent RAAB studies (Tables 2-3) (Figures 1 and 2) and all eligible studies (Tables 4-5) (Figures 3 and 4) are fairly similar to results from the original meta-analysis, which previously demonstrated ORs of 1.12 (95% CI: 0.78-1.63) and 0.94 (95% CI: 0.77-1.15) for women receiving cataract surgery at a VA of <3/60 and <6/18, respectively, compared to men.17 The main difference between the 2 meta-analyses was that the previous study reported some heterogeneity for results at a VA of <3/60 (I2 = 30%), while there was no heterogeneity encountered in the current study. The updated meta-analysis demonstrates that the majority of Latin American countries continue to demonstrate gender equity in terms of CSC.
Both the original and updated meta-analyses included unpublished data to avoid publication bias. It should be noted that the original meta-analysis included data from 11 studies from 11 countries, whereas the current study included data from 19 studies in 17 countries. Also noteworthy is that among the 13 new studies included, 5 studies presented newer, updated data in 5 countries, 4 of which had only prior regional data before undertaking a national RAAB survey. Therefore, a stronger representation of the Latin American region was observed in the current study.
These CSC findings for Latin America contrast sharply with gender inequity in terms of receiving cataract surgery in other developing countries and regions7-13. For example, a recent systematic review of data from 22 studies in India found that although women had a 69% higher odds of being cataract blind (OR: 1.69, 95% CI: 1.44-1.95), they had a 27% lower odds of receiving cataract surgery (OR: 0.73, 95%: 0.45-1.01). Where gender inequity in terms of CSC is present, it is not adequate to merely provide eye health services equally to men and women, when the burden of cataract is greater for women. It has been suggested that to achieve gender equity in terms of receiving cataract surgical services, up to 65% of cataract surgeries should be performed on women, which would decrease the incidence of global blindness by 12.5%4,5.
As with the original meta-analysis of CSC in Latin America, the findings of the updated meta-analysis must be taken into consideration with the possibility that there may be gender inequity in countries lacking RAAB surveys, or there may be inequity in parts of some countries (although the majority of the most recent surveys were national surveys), or there may be inequity reported by epidemiological surveys excluded from this meta-analysis that used methodologies different than the RAAB17. This last point is especially important because the sample size calculation used in the RAAB methodology is not powered to detect statistically significant gender differences in CSC. Although the provision of cataract surgery is used to measure the overall provision of eye care services,6 we do not know from this study if gender inequity exists in terms of the quality of cataract surgery (i.e., postoperative outcomes) or in terms of receiving treatment for other eye diseases.17 The RAAB methodology now includes a diabetic retinopathy component that has been used in select studies in Latin America that measures coverage for patients with diabetic eye disease,25-27 and an effective CSC indicator has been developed to assess surgical quality9. Future analysis could explore gender inequity in terms of surgical outcomes and eye care among patients with diabetes, as more relevant data become available.
Although we did not perform a systematic review that assessed the quality of the studies analyzed, the results from this meta-analysis are reliable due to the fact that the studies followed a standard design recommended by the World Health Organization for obtaining ophthalmic epidemiology data,6 with analysis of original study data done using the same software. Thus, there was no variation in the quality of data used in this meta-analysis17. However, for the more comprehensive analysis of all eligible studies, we did use data from studies that are over 10 years old, which may not reflect the actual situation of CSC in those countries and regions. Therefore, it is possible that the results of the meta-analysis of studies published since 2011 are more reliable.
Conclusions
This updated meta-analysis of CSC data obtained from ophthalmic epidemiological studies done in Latin America continues to support the finding that gender inequity in terms of receiving cataract surgery is not an issue in the region. The results of this study do not provide further insight into gender inequity in terms of the quality of cataract surgery and other types of eye care services. As more regional data become available, a more robust analysis of gender inequity in eye care could be done in the future.











 text new page (beta)
text new page (beta)




