Introduction
Heterotopic ossification (HO) is an extremely rare benign condition, which consists in abnormal differentiation of mesenchymal cells into osteoblastic cells. It may affect musculoskeletal system, skin, fascia, abdominal midline, and intraabdominal structures1. The exact causes for the development of this pathology are not well known; however, several cases have been associated with previous musculoskeletal and abdominal trauma (including surgical procedures), gastric carcinoid tumor, appendiceal mucocele, and colonic polyps1. Intraabdominal HO may involve mesentery, abdominal wall or peritoneum, been the last one the least frequent2. Patients generally present with clinical manifestations of intestinal obstruction, but in our case, the patient also developed frozen abdomen, which consists in adhesions between the abdominal viscera and the undersurface of the anterior abdominal wall3. We report a case of small bowel obstruction complicated with midline heterotopic peritoneal ossification, which occurred after the fourth laparotomy associated with previous adhesions.
Case report
A 54-year-old Mexican man presented to the emergency department in our institution with small bowel obstruction secondary to adhesions, with prior history of laparotomy due to acute complicated appendicitis with peritonitis 19 years ago, with a second intervention due to small bowel obstruction secondary to adhesions after 24 h of the first operation.
In this occasion, after 48 h of conservative management and without showing any clinical improvement, he went through laparotomy with adhesiolysis of multiple firm adhesions, mainly in the terminal ileum; he was left with an open abdomen, which was closed on the 5th post-operative day. His post-operative evolution was torpid, presenting the next 14 days with intolerance to solid diet, abdominal distention, and intermittent liquid evacuations. An abdominal computed tomography (CT) with double contrast was conducted, identifying mechanical small bowel obstruction due to probable new adhesions figure 1.

Figure 1 Abdominal computed tomography scan showing peritoneum calcification at the midline incision (arrow).
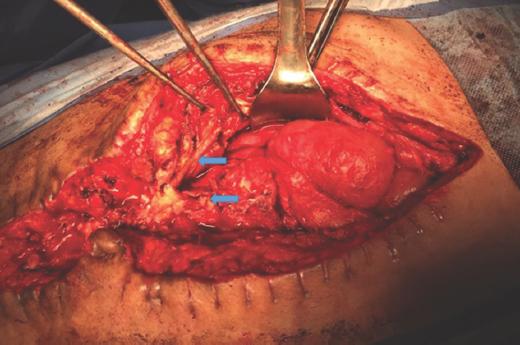
A second laparotomy was performed, finding a frozen abdomen with the parietal peritoneum abnormally firm, thickened, petrified at the intraabdominal midline, which made it impossible to liberate, having as an only choice to perform a jejunostomy at the level of the abdominal wall incision figure 2.
A biopsy of the parietal peritoneum was sent to histopathology reporting extensive metaplastic bone deposition with osteoblastic activity without atypia or evidence of malignancy.
The patient developed short bowel syndrome requiring permanent parenteral nutrition and correction of electrolytic disturbances and acute renal failure. After 2 months, he was discharged. During his follow-up, he has remained stable, with mild malnutrition and without electrolytic disturbances, being strictly followed in consult by multiple specialties figure 3A and B.

Figure 3 A-B: in both images, extensive immature trabecular bone with an osteoblastic rim is surrounded with adipose tissue. The panoramic view (×1) shows peripheral reparative fibrosis. The inflammatory component was irrelevant. There was not atypia or neoplastic elements (hematoxylin and eosin, ×1 and ×40).
Discussion
Primary HO is a rare condition where bone develops in a tissue, which does not normally undergo ossification4.
Also known as intraabdominal myositis ossificans, it consists on deposition of organized calcium-containing osteoblasts and structured bone layers. There are three types of HO: myositis ossificans circumscripta, myositis ossificans progressiva, and traumatic myositis ossificans being the last one present in our patient5. This pathology is a rare and benign form of ossification related to previous abdominal trauma and/or abdominal surgery. The physiopathology of HO is not clear yet; however, it can be explained by two theories: (1) implant of osteogenic cells from perichondrium, periosteum of pubic symphysis or sternum, who have migrated during laparotomy or trauma and (2) process of osteoblastic metaplasia of pluripotent mesenchymal cells in response to severe inflammatory environment due to trauma or repetitive surgical manipulation of the tissue. Bone formation generally occurs within weeks or days after the surgery6-8.
This entity has a male prevalence within the age of 22-80 years old. In most of the reported cases, abdominal trauma or previous surgery is the trigger event, clinically behaving as small bowel obstruction with oral intolerance, distension, and abdominal pain2,9.
CT scan imaging provides evidence of peritoneal ossification guided by the value of Hounsfield units; however, in this specific case, the osteogenic tissue was not demonstrated. Diagnosis is generally made as a transoperative finding9.
It has a good prognosis without evidence of malignancy and if the patient's general condition allows it, we should aim for conservative management; nevertheless, in the presence of asymptomatic patient or clinical deterioration, surgical intervention is required9.
In this case, having a history of multiple surgeries causing intestinal obstruction secondary to adhesions, not resolving with medical management, we decided surgical intervention, performing an exploratory laparotomy9. The findings were extensive intestinal adhesions; hence, we made an adhesiolysis which predisposed a new acute inflammatory process. In addition, he was left with a temporarily open abdomen handled with Bogota bag to monitor the possibility of intestinal perforation, exposing the viscera and leading to fluid and heat loss10. Regardless of the method used, the ongoing loss of peritoneal fluid is associated with a net loss of protein. Since the total daily volume of fluid removed can be over 1 l, the net loss of protein per day can lead to protein-calorie malnutrition, resulting in delayed healing, constant inflammatory stimuli, and therefore deficient tissues10.
In our case, abdominal wall ossification occurred due to repetitive surgical injuries, as reported in the literature, with constant inflammatory stimulus until bone formation5. Open abdomen has not been described as a risk factor for HO; however, in this specific case, we considered that this entity and therefore the abdominal inflammatory wall response, probably contributed to the process of abdominal wall ossification.











 text new page (beta)
text new page (beta)