Introduction
The emergence of a new disease is disturbing to health sevices due to its epidemiologic complexity, mainly if its transmission mechanism and spread favor its evolution to an epidemic or a pandemic. On december 8th of 2019, in Wuhan, Hubei, China, there were diverse cases of pneumonia reported with an unknown etiology, all of them characterized by the development of severe symptons of acute respiratory infection and even acute respiratory distress syndrome (ARDS)1,2,3. On January 30th of 2020, the World Health Organizations (WHO) declared these cases as a public health emergency of international interest; and, after the search of an etiological agent, the Chinese Center for Disease Control and Prevention discovered a newfound virus belonging to the Coronaviridae family as the cause, and named it Wuhan Coronavirus or novel 2019 (2019-nCov); shortly after, the International Committee on Taxonomy of Viruses (ICTV) stablished its name as SARS-CoV-2, and the disease as COVID-194,5.
To January 2021, the WHO reported 43, 843, 324 confirmed cases and 1,009, 286 deceases due SARS-CoV-2. In Mexico, the first confirmed case of SARS-CoV-2 was reported on february 27th of 2020, according to the information emitted by the Health Secretary, and as of January 31st of the present year, there have been 1,864,260 confirmed cases and 158,536, defunctions due to SARS-CoV-2. In the state of Tabasco, there have been reported 49,248 confirmed cases and 3,415 deceases, with an incidence rate of 205.6 cases for every 100,000 people6,7.
It has been demonstrated that the SARS-CoV-2 is transmitted via person to person, identifying clusters of intrafamiliar cases and health workers transmission8, being fever, cough, fatigue, myalgia, headache, anorexia, shortness of breath, hemoptysis and sputum production the most frequent symptoms9,10.
As of right now, there is no protocol to eradicate COVID-19 and because of it several research studies are being held at a worldwide level, with the objective of obtaining an specific treatment and the development of an effective vaccine in order to diminish COVID-19 spread and the number of defunctions11,12,13.
There have been developed different diagnostic tests for SARS-CoV-2, such as Reverse Transcription Polymerase Chain Reaction (RT-PCR), Real Time PCR, Real Time Reverse Transcription Quantitative Polymerase Chain Reaction (rRT-qPCR), COVID-19-RdRp/Hel Real-Time Reverse Transcription-PCR Assay, Point of Care Tests, Loop- Mediated Isothermal Amplification (RT-LAMP), Complete Genome Analysis with New Generation Sequentiation.(NGS), Fluorescence Based Quantitative Polymerase Reaction Assay, Enzyme Linked Immunosorbent Assay (ELISA), Computed Tomography Scans and X-rays14,15,16,17,18.
On the other hand, the Instituto de Seguridad Social del Estado de Tabasco (ISSET), as part of the National Health System, is not only obliged to show its job against COVID-19 but also to share all the data gathered from the epidemiological experiences live, in virtue of that, this study has as a main objective the epidemiological caracterization of COVID-19 cases presented in the ISSET during the period between march 1st of 2020 and january 18th of 2021.
Materials and Methods
A descriptive, cross-sectional, retrospective study was conducted in the Instituto de Seguridad Social del Estado de Tabasco (ISSET), in Mexico, between march 1st of 2020 and january 18th of 2021. All beneficiaries with respiratory symptomatology that requested for medical attention at any of the ISSET medical units were included. The definitions of suspected COVID-19 case, confirmed case, and contact with COVID-19 case were all according to the operational definition of the National Commitee for Epidemiological Surveillance (CONAVE), including 11, 486 suspected cases.
Data was collected from the Respiratory Disease Surveillance System platform (SISVER), the census concentrations and the daily reports from de Epidemiology Department. Data gathered included: age, genre, subjacent comorbidities, SARS-CoV-2 tests with SARS-CoV-2 Real Time Polymerase Chain Reaction (rt-PCR-SARS-CoV-2), and defunctions in hospitalized patients by epidemiological week, aswell as confirmed cases of SARS-Cov-2 in health personnel.
The numerical data was expressed as count proportions in percentages for categorical data. Incidence rate and lethality rate were calculated from obtained data. Due to the design and characteristics of the research, there was no informed consent signing required, for the analyzed variables did not interfere with the life nor prognosis of any of the patients. For its execution we counted with the approval of the Teaching, Research, Training and Ethics Committee of the Institution with file number 004-2020, which considered this protocol as of low risk for the patients.
Results
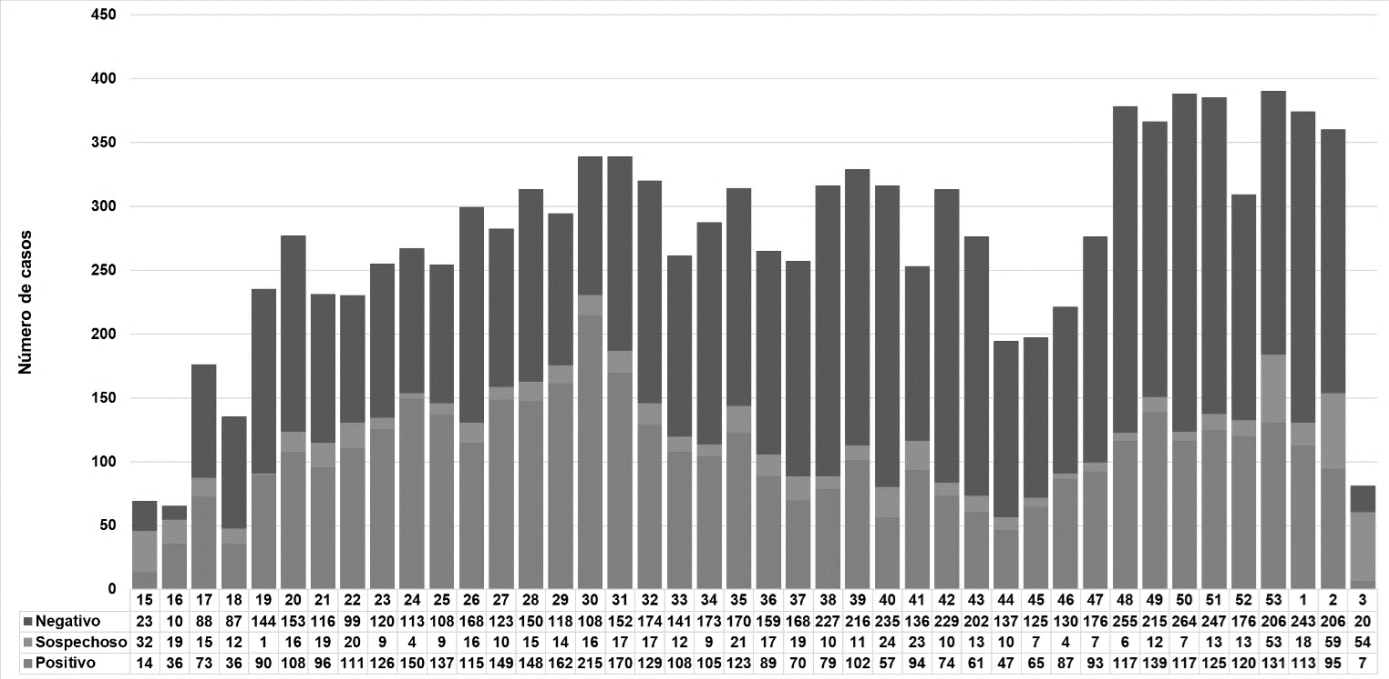
As from the collected data from the Respiratory Disease Surveillance System platform (SISVER), a total of 11,486 people with respiratory symptomatology that requested for medical attention was obtained, to which art PCR-SARS- CoV-2 test was made, with a sampling rate of 31.9 for every 1,000 people, of which 4,283 were confirmed cases, with a proportion of 2,186 (51.04%) females and 2,097 (48.96%) males, obtaining an incidence rate of 225.9 cases for every 10,000 people (Table 1). Moreover, the larger number of confirmed cases and cases with symptomatology was observed on week 30 (july 19th to july 25 of 2020) with 215 cases (Figure 1).
Table 1 Characteristics of ISSET beneficiaries in the period from march 1st of 2020 ton january 18th of 2021.
| SARS-CoV-2 positive cases | |||||||
|---|---|---|---|---|---|---|---|
| Total | n | % | Females | Males | |||
| n | % | n | % | ||||
| rt-PCR Tests | 11,486 | 4,283 | 37.28 | 2,186 | 51.03% | 2,097 | 48.96 |
| Sampling rate | 60.60° | ||||||
| Incidence rate | 225.90* | ||||||
| Lethality rate | 7.70# | ||||||
| Defunctions | 475 | 328 | 7.65 | 138 | 3.22 | 190 | 4.43 |
rt-PCR, Reverse Transcription Polymerase Chain Reaction; n, Sampling number, %, Percentage; *, Incidence for every 10,000 people; °, Sampling for every 1,000 people; #, Defunctions for every 10,000 people. Source: SISVER platform cut from 03/01/2020 to 01/18/2021.
Regarding age, the group with more positive cases was the one between 50 and 54 years, with 586 cases, 282 females (6.58%) and 304 males (7.09%). Regarding genre, the female age group with more positive cases was the one beteween 45 and 49 years, and in males the one between 50 and 54.
Of all the attended cases in the registered period, the largest number of beneficiaries consisted on 1,988 (46.41%) direct beneficiaries and 748 (17.46%) ISSET enclosed employees, which included nurses, medical doctors, laboratory workers and others, nurses being the most affected group with 260 (6.07%), followed by medical doctors with 198 (4.62%) (Table 2). In accordance to procedence, the largest number of positive cases was from the municipality of Centro with 3,212 (74.99%) followed by Nacajuca with 377 (8.80%) confirmed cases (Figure 2).
Table 2 ISSET attended beneficiaries positive to SARS-CoV-2.
| n | % | |
| Beneficiaries | 1,988 | 46.41 |
| Others | 890 | 20.77 |
| Other health workers | 267 | 6.23 |
| Nurses | 260 | 6.07 |
| Other professionals | 208 | 4.85 |
| Medical doctors | 198 | 4.62 |
| Students | 162 | 3.78 |
| Retirees/Pensioners | 158 | 3.68 |
| Teachers | 96 | 2.24 |
| Drivers | 33 | 0.77 |
| Laboratory workers | 18 | 0.42 |
| Dentists | 5 | 0.11 |
| Total | 4,283 | 100 |
Source: SISVER platform cut from 03/01/2020 to 01/18/2021.

Figure 2 SARS-CoV-2 positive cases by municipality. Source: SISVER platform cut from 03/01/2020 to 01/18/2021.
On the other hand, percentage distribution of comorbidities in patients with COVID-19 was presented in the following way: 1,619 cases presented some King of comobordity, mainly hypertensive disease with 852 (19.98%) cases, followed by diabetes with 694 (16.20%) cases and obesity with 503 (11.74%) cases (Figure 3).
From march 1st of 2020 to the cut date, january 18th of 2021, there are 4,283 COVID.19 positive cases and 328 COVID-19 defunctions reported in ISSET, obtaining a lethality rate of 7.70 defunctions forever 10,000 (Table 1), of which 138 were females and 190 were males (Table 3). Observing the largest number of mortality in the age group population from 60 to 64 years old with 56 (17.07%) defunctions, regarding genre the largest number of mortality was in males in the age group between 60 to 64 years old with 36 (10.97%) defunctions, followed by females in the age group of 55 to 59 years old with 24 (7.31%) defunctions. Also, the main comorbidities associated to COVID-19 were hypertension with 138 (42.07%) cases and type 2 Diabetes with 121 (36.89%) cases.
Table 3 Defunctions acording to age group, genre and diagnosis.
| Suspected | Positive | |||||||||
| Age range | Total | Females | Males | Females | Males | |||||
| n | % | n | % | n | % | n | % | n | % | |
| <1 years old | 1 | 0.21 | 0 | 0 | 0 | 0 | 1 | 0.21 | 0 | 0 |
| 25 - 29 years old | 2 | 0.42 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0.42 |
| 30 - 34 years old | 3 | 0.63 | 1 | 0.21 | 1 | 0.21 | 0 | 0 | 1 | 0.21 |
| 35 - 39 years old | 7 | 1.47 | 0 | 0 | 2 | 0.42 | 3 | 0.63 | 2 | 0.42 |
| 40 - 44 years old | 17 | 3.58 | 1 | 0.21 | 1 | 0.21 | 3 | 0.63 | 12 | 2.53 |
| 45 - 49 years old | 36 | 7.58 | 2 | 0.42 | 10 | 2.11 | 10 | 2.11 | 14 | 2.95 |
| 50 - 54 years old | 52 | 10.90 | 6 | 1.26 | 14 | 2.95 | 17 | 3.58 | 15 | 3.16 |
| 55 - 59 years old | 77 | 16.20 | 10 | 2.11 | 13 | 2.74 | 24 | 5.05 | 30 | 6.32 |
| 60 - 64 years old | 77 | 16.20 | 14 | 2.95 | 7 | 1.47 | 20 | 4.21 | 36 | 7.58 |
| 65 - 69 years old | 59 | 12.4 | 12 | 2.53 | 8 | 1.68 | 17 | 3.58 | 22 | 4.63 |
| 70 - 74 years old | 47 | 9.89 | 6 | 1.26 | 11 | 2.32 | 15 | 3.16 | 15 | 3.16 |
| 75 - 79 years old | 42 | 8.84 | 4 | 0.84 | 8 | 1.68 | 9 | 1.89 | 21 | 4.42 |
| 80 - 84 years old | 35 | 7.37 | 3 | 0.63 | 7 | 1.47 | 12 | 2.53 | 13 | 2.74 |
| >85 years old | 20 | 4.21 | 2 | 0.42 | 4 | 0.84 | 7 | 1.47 | 7 | 1.47 |
| Total | 475 | 100 | 61 | 12.8 | 86 | 18.1 | 138 | 29.10 | 190 | 40 |
Source: SISVER platform cut from 03/01/2020 to 01/18/2021.
Discussion
The SARS-CoV-2 and COVID-19 disease recently emerged, represent a great threat to the world´s public health. The current appearance of COVID-19 is the third reported outbreak in humans in the last 2 decades19. 10 months have passed since the world heard about a novel coronavirus that would cause the world to be in a health emergence state, SARS-CoV-2 has quickly spread among travelers in more than 200 countries in the world, provoking more than 30 millions of confirmed cases and nearly one million of deaths in the entire planet20,21,22.
Since the first reported case of COVID-19, the total number of cases has been increasing in the entire country, increasing the population lethality rate. In the present study 4,283 SARS- CoV-2 positive cases were reported in the period between marchs 1st of 2020 and january 18th of 2021, with 51.03% of the total being females, and 328 COVID-19 associated defunctions, with a lethality rate of 15.6 for every 10,000 people, being higher in men between 65 and 69 years old. In Mexico, Villagrán-Olivas K.A. et al., 202023, reported the higher incidence in females, with a lethality rate of 31.25%, mainly in males older than 60 years old. In Argentina, Rearte A. et al., 2020, reported the highest number of cases in men, reaching a lethality rate of 65.31 for every 100,000 people older than 80 years old24.
Regarding the epidemiological week, the highest inciden of positive SARS-CoV-2 was in the week 30 (between july 19th and 25th) with 215 (5.01%) positive cases. The current trendings suggest the apparition of future outbreaks due to climatic changes and ecological conditions that can be associated with the contact with humans and animals. Factors such as occupation, age, comorbidities like diabetes, respiratory diseases, cardiovascular disease, obesity and even genre are associated to the predispostion of COVID-19 disease, increasing the risk of mortality 25,26,27,28,29.
Being considered a threath to the health sector, the virus exposure is more frequent in health workers, due to the number of contact cases, suspected cases and positive cases to which the health workers are exposed to. The inadequate use ,incomplete use, or lack of protecting gear for the health workers be it privect practice or public service is associated to an increase of cases, mainly in medical doctors and nursing body, which are the frontline contact.30,31,32,33,34,35.
Lastly, the presence of comobordities, such as diabetes, hypertension, obesity, renal disfunction, among others, has been associated with an increase in complication and lethality rate36,37. Bello-Chavolla et al., 2020, describe that the population with diabetes and obesity increases the SARS- CoV-2 contagion propability, aswell as the lethality rate38. While Li J et al, 2020, observed that hypertensive patients presented a more symptomatology, a higher prevalence of respiratory distress and a higher lethality rate39.
Conclusions
The incidence of SARS-CoV-2 cases has been in increment, in the period between march 1st of 2020 to january 18th of 2021 ISSET reported 4,283 SARS_coV-2 positive cases, mainly in female population between the age group of 50 to 54 years.
The mortality presented hereby is high, mainly in people older tan 60 years old, with associated chronic noncommunicable diseases, with atypical manifestations and catastrophic effects.
Of all positive cases, 21% belonged to the health personnel, mainly nursing body. This increase in health workers contagion is related to many factors, the lack of or inadequate protective gear, unefficient or poor control of infectious diseases, work overload and preexisting medical conditions all increase the risk of contagion in this population.











 text new page (beta)
text new page (beta)