Introduction
Wunderlich syndrome, or spontaneous renal hematoma, first described in 1856,1 is a rare entity consisting of spontaneous bleeding into the perirenal space. Its origin is neoplastic in 60% of cases and renal angiomyolipoma is the most common benign cause.2 Collision tumors are uncommon conditions in which 2 different histologic types of neoplasms coexist. There are currently very few reports of a collision tumor composed of clear cell renal cell carcinoma and angiomyolipoma.
Case presentation
A 29-year-old man with a past medical history of autism and unclassified, self-limited epilepsy was admitted to the emergency department due to macroscopic hematuria of one-hour progression. Vital signs upon admission were 21 breaths per minute, HR of 90 beats per minute, BP of 80/60 mm Hg, temperature of 36ºC, and pulse oximetry of 93% at room air. Physical examination showed a constitutionally ill-looking, conscious patient, who understood and obeyed simple commands but lacked verbal response due to his autism. Skin examination revealed a cephalic fibrous plaque, oral fibromas, facial angiofibromas, and melanotic macules on the face and extremities, apparently chronic in nature (Figure 1, Figure 2). Abdominal examination showed decreased peristalsis, abdominal distension due to ascites, and a non-tender palpable mass in the right flank with dull percussion at the right abdominal quadrants. Other aspects of physical examination were unremarkable.

Figure 2 Upper image: Fibrous and hypomelanotic plaques. Middle image: Fibrous plaques. Lower image: Oral fibromas
Laboratory findings upon admission were: hemoglobin 4.58 g/dl, MCV 96 fl, MCH 29 pg/cell, white blood count 17.1 K/mm3, neutrophils 91.3%; platelets 236 K/mm3; BUN 14 mg/dl, Cr 1.7 mg/dl, albumin 2.8 g/dl, and corrected Ca 8.16 mg/dl. Urinalysis showed cloudy, dark red urine, with specific gravity of 1.027, pH 6.5, negative nitrites, positive leukocyte esterase, abundant non-dimorphic erythrocytes per HPF, and 0-1 leukocytes per HPF. Blood gases, electrolytes, and other laboratory tests were within normal parameters.
Urology consultation was carried out due to anemia-related hematuria. Initial management included IV fluids, 2 units of packed red blood cells, and a 3-way transurethral Foley catheter with continuous 0.9% saline irrigation. After initial IV fluid resuscitation and blood transfusion, hemoglobin rose to 7 g/dl and blood pressure improved. An abdominal CT-scan with IV contrast identified a 140 × 120 × 180 mm right renal mass and a 75 × 75 × 63 mm left renal mass (Figure 3, Figure 4). On the patient’s right side, a heterogeneous retroperitoneal hematoma in retroperitoneal zone 2 was observed, along with a 30 × 30 × 50 mm paraaortic adenopathy. There were disseminated hypodense lesions in the liver, as well as free intraperitoneal fluid. An image in the urinary bladder, measuring 49 HU, was suggestive of an intravesical clot. A hyperdense image on the thoracic spine, on T6 and T8, was consistent with osteoblastic lesions.
Assessment by the dermatology service was carried out. Diagnosis of tuberous sclerosis complex was made through clinical criteria: hypomelanotic macules, fibrous cephalic plaque, oral fibromas, and facial angiofibromas (Figure 1, Figure 2). Initial diagnoses included: 1) Autism 2) Tuberous sclerosis complex 3) Suspected angiomyolipoma with Wunderlich syndrome 4) Intractable hematuria 5) Acute kidney injury AKIN II and 6) Suspicious hepatic angiomyolipomas versus metastasis.
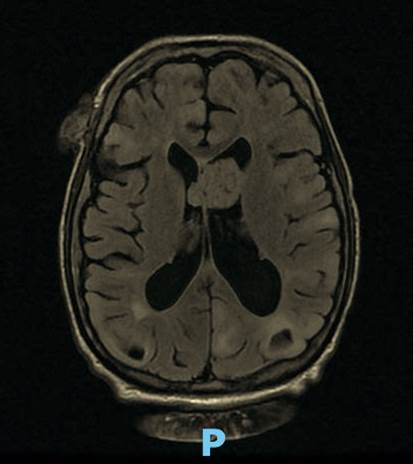
Our first management step included the angioembolization of the right renal artery. We decided on that approach due to the risk of intraoperative bleeding. After initial angioembolization, hematuria was controlled, and hemoglobin was stabilized. Further assessment by other services was conducted. The evaluation by the genetics department determined tuberous sclerosis from the clinical criteria, in agreement with the dermatology service. The patient’s major features included hypomelanotic macules, angiofibromas, ungual fibromas, and angiomyolipoma, whereas the only minor feature was intraoral fibromas. Diagnosis is considered definite when there are two major features or one major feature plus two or more minor features, and so no further genetic testing was conducted on our patient. Other services reported no remarkable findings. The ophthalmologic examination identified no retinal hamartomas and dental examination revealed no dental enamel pits. Neurosurgery conducted a gadolinium contrast brain MRI, documenting a 31 × 24 × 26 mm supratentorial interventricular lesion on T1-T2, consistent with a giant cell astrocytoma (Figure 5).
Further urologic treatment included right nephrectomy after the first 24 hours of angioembolization (Figure 6). Intraoperative findings included a giant renal tumor and 4 liters of free abdominal fluid. The anatomopathologic diagnosis of the renal tumor was a Fuhrman 4 collision angiomyolipoma and clear cell renal cell carcinoma, which could explain the suggestive distant metastatic lesions in the liver and brain. Neurosurgery performed tumor resection and the anatomopathologic findings were a grade I (WHO) subependymal giant cell astrocytoma, adding another major criterion to the tuberous sclerosis complex diagnosis.
Further treatment was carried out by the oncology service with everolimus for the remaining angiomyolipoma. Estimated treatment time is one year.
Discussion
The symptoms of tuberous sclerosis complex (TSC) are heterogeneous and involve almost all tissues, including the nervous system, skin, kidney, lungs, and heart. The estimated prevalence is 8 per 100,000 persons. TSC is underestimated by up to 50% due to low clinical suspicion among health providers.3
The TSC1 and TSC2 genes encode hamartin and tuberin, respectively. TSC pathophysiology is associated with a decreased or absent expression of those proteins.4 A two-hit mechanism is hypothesized, in which two mutations are needed for a phenotypic change. As a result, regulatory functions are lost and the mTor receptor (rapamycin receptor) is activated, providing an anabolic pathway that causes a dysregulated production of nuclear acids and proteins, manifested by cell enlargement, hypertrophy, and hyperplasia.5
The TSC diagnostic criteria were updated at the International Tuberous Sclerosis Complex Consensus Conference in 2012. Genetic testing criteria have been included as a definite diagnosis (pathogenic mutation of TSC1 or TSC2), but clinical criteria are sufficient for diagnosing TSC. The definite diagnosis includes either two major features or one major feature plus two minor features. Major features include hypomelanotic macules (>3, at least 5 mm diameter), angiofibromas (>3) or the presence of a fibrous cephalic plaque, ungual fibromas (>2), a Shagreen patch, multiple retinal hamartomas, cortical dysplasias, subependymal nodules, subependymal giant cell astrocytoma, cardiac rhabdomyoma, lymphangioleiomyomatosis, or angiomyolipomas (>2). Minor features include “confetti” skin lesions, dental enamel pits (>3), intraoral fibromas (>2), a retinal achromic patch, multiple renal cysts, or nonrenal hamartomas.6
TSC is highly variable in each patient. All tissue types can be compromised, and the central nervous system is the most affected site. Cellular hyperplasia is the main pathologic finding. The paraventricular astrocytes of the lateral and third ventricles are involved in nearly 80% of patients. Lesions correlated with epileptogenic foci can manifest as seizures of any kind during early childhood.6 Eighty percent of those patients develop epilepsy during the first three years of life, presenting as different types of seizures (infantile spasms or tonic, atonic, or tonic-clonic seizures). Almost 30% of the patients present with drug-resistant epilepsy during their lifetime.7
Angiomyolipoma (AML) is associated with a high risk of death due to bleeding. Said risk depends on AML size, given that it is higher in tumors > 4 cm. Aneurysms present in 80% of AML, and when > 9 mm, are predictors of rupture.8 Wunderlich syndrome refers to an acute episode of bleeding into the subcapsular or perinephric space, and spontaneous rupture of an AML is its most common cause. Other etiologies for acute bleeding into the subcapsular space include vasculitis, neoplasms, and hematologic disorders. Treatment depends on the individual patient, clinical conditions, and hospital resources.9 Renal artery embolization is as effective as nephrectomy and is associated with reductions in pain, gross hematuria, and retroperitoneal hemorrhage. Interventional procedures have shown fewer postoperative complications of ileus, pain, or infection, compared with nephrectomy.10
Everolimus is an mTor inhibitor used as a gold standard to treat asymptomatic AML. In a controlled trial (EXIST-2), there was a 50% reduction in the baseline volume at 24 weeks of treatment, compared with a 0% percent reduction in the patients receiving placebo.11
Conclusions
In the present case report, we performed angioembolization prior to radical nephrectomy in a clinically stable patient with retroperitoneal hematoma, who responded well to intravenous fluids and blood transfusion. Although both kidneys had angiomyolipoma, we decided to carry out right nephrectomy exclusively, because the hematoma could be contained, there would be a lower risk for bleeding, and because the patient was admitted to the emergency department with anemia-related hematuria. Follow-up with palliative care is recommended, given that prognosis is poor in cases with the histologic findings of a collision tumor composed of angiomyolipoma and clear cell renal cell carcinoma.
Given a clinical scenario, such as the one described herein, we propose angioembolization of the renal artery before nephrectomy, to reduce the risk for intraoperative bleeding. The most interesting elements of the present case were the multisystemic presentation of the disease and the histologic results of a collision tumor made up of angiomyolipoma and clear cell renal cell carcinoma, a rare entity in the medical literature.











 text new page (beta)
text new page (beta)