Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.22 n.2 Ciudad de México Apr./Jun. 2018
Original research
Articular noise in patients rehabilitated with removable partial dentures
* Assistant Professor, Clinical Prosthesis Chair I. School of Dentistry, UNNE (National Northeastern University), Corrientes. Argentina.
§ Assistant Professor, Dentomaxillary Surgery II Chair. School of Dentistry, UNNE (National Northeastern University), Corrientes. Argentina.
II Dean, Professor, Chair of Surgery I, surgical and anesthetic techniques. School of Dentistry, UNNE (National Northeastern University), Corrientes. Argentina.
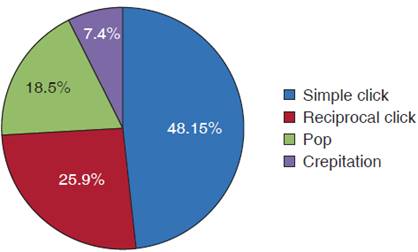
Mandibular noises, along with mandibular restrictions, constitute classical signs of temporomandibular joint disorders (TMJD) which can be accompanied with painful symptomatology. Its multifactorial etiology encompasses emotional stress, trauma, deep pain, parafunctional activity and occlusal problems. The aim of the present transversal and descriptive study was to determine frequency and types of articular noises and their relationship with Kennedy’s classes, as well as presence or absence of painful symptomatology. A total of 50 patients attending the course of prosthesis clinical chair 1 were examined, they were subjected to tactile exploration and temporomandibular Joint (TMJ) auscultation. Frequency of articular noises was 48%, simple clicks 48.15%, reciprocal clicks 25.9%, pops 18.5% and crepitations 7.4%. Clinical history revealed presence of pain in 14% of cases. Coincidence of both signs (pain and noise) occurred in 25%. High incidence of simple clicks related to Kennedy’s class II was observed.
Key words: Temporomandibular disorders; temporomandibular joint (TMJ); temporomandibular joint disorders (TMJD)
Los ruidos articulares constituyen junto a las restricciones mandibulares, los signos clásicos de los trastornos temporomandibulares (TTM) que pueden ir acompañados por sintomatología dolorosa. Su etiología multifactorial reconoce estrés emocional, traumatismo, dolor profundo, actividad parafuncional y problemas oclusales. El objetivo de este estudio descriptivo transversal fue determinar la frecuencia y tipos de ruidos articulares y su relación con las clases de Kennedy y la presencia o ausencia de sintomatología dolorosa. Se realizó exploración táctil y auscultación de la articulación temporomandibular (ATM) a 50 pacientes concurrentes a la Cátedra Clínica de Prótesis I curso. La incidencia de ruidos articulares fue del 48%: clics simples 48.15%, clics recíprocos 25.9%, pop 18.5%, y crepitaciones 7.4%. La anamnesis mostró presencia de dolor en un 14%. La coincidencia de ambos signos (dolor y ruido) coincidió en un 25%. Se presentó la alta incidencia de clics simples relacionada con la clase II de Kennedy.
Palabras clave: Desórdenes temporomandibulares; articulación temporomandibular (ATM); trastornos temporomandibulares (TTM)
Introduction
Temporomandibular joint biomechanics is a complex system, since these articulations are connected to the lower jaw, and each works separately.1,2 Functional changes can appear at one or both sides of the articulation, even more, there could be alterations without the patient noticing them.
TMJ disorders have been identified through the years with different nomenclature,3 they were first described by otolaryngologist James Costen in 1934, for this reason it was called «Costen’s syndrome». After 67 years from its first description, this group of symptoms have received different names such as: temporomandibular dysfunction pain syndrome, described by Schwartz (1955), temporomandibular joint dysfunction syndrome, (Shore 1959), temporomandibular joint functional alterations (Ramjford and As), myofacial dysfunction syndrome (Laskin 1969), chronic lesion of the meniscus, myofacial dysfunction pain, temporomandibular arthralgia, and presently, craniomandibular disorders, among others; nevertheless standardization of definition, diagnosis and treatment have not yet been achieved. Due to the amount of terms used in literature to describe it, it is difficult to determine it and know it as a single entity, therefore, the American Dental Association has adopted the term temporomandibular joint disorders (TMJD), considering this includes TMJ as well as all disorders associated to masticatory system functions.4
Masticatory function can result affected by some type of alteration, in cases when it is important and overcomes the physiological tolerance of the subject, creating a response within the system. This response can manifest itself with the presence of different clinical symptoms related to TMJD : articular noise caused by alterations of condyle movement on the disk, pain caused by TMJ alterations, pain caused by muscle spasm of the masticatory muscles, decrease in amount of mouth opening, limitation of mandibular movements and mandibular deviation.
Contemporary studies recommend use of four factors to establish diagnosis and follow TMJD’s evolution.5-7
Factor 1: Composed by movement limitation as well as pain during lateral movements and capsular palpation.
Factor 2: Lateral deviation, mandibular rigidity, bilateral replicable clicks during opening or closure and fine bilateral crepitus.
Factor 3: Bilateral reciprocal clicks, replicable in laterality.
Factor 4: Strong bilateral crepitus
Study of TMJD shows complex and multifactorial etiology which could be grouped with respect to its origins.
Predisposing factors (increase risk and create suitable environment for dysfunction).
Precipitating factors (include macro and micro trauma).
Perpetuating factors (preserve the problem and hinder treatment).
Previously, occlusal disharmony was considered the sole responsible factor for TMJD, where TMJ exerts a totally passive activity,8 Campos,9 reinforces this theory, calling it «occlusal disease». Vartan Behsmila10 is also a part of this trend of thought, he explained that occlusal disharmony is always the cause for clicks in the TMJ. This author reports that occlusal rehabilitation as single intervention improves articular function. Dawson,11 in the same trend, suggested that harmonization of occlusion almost invariably resulted in correction of the alteration, the noise disappears as soon as occlusion is corrected.
Presently, there is no direct cause-effect relationship between occlusal disharmony and articular alteration, nowadays it is accepted that TMJD’s origin is multi-factorial.12-15 Okeson proposed that there are five factors associated to these conditions: occlusal conditions, trauma, emotional stress, deep pain and parafunctional activity. Echeverry Guzman reported that, in order for an alteration to exist at articular level, there must be a conjunction of psychological and physiological factors, since, if only one factor were to act, the body could tolerate it.
Four occlusal characteristics are frequently found In TMJD patients: presence of a skeletal anterior open bite, sliding from retruded contact position to maximum upper intercuspation position at 2 mm, extrusion greater to 2 mm and absence of four or more posterior teeth lost and never substituted.
Material and methods
The sample was composed of 50 patients suffering partial bi-maxillary tooth loss. Patients attended facilities of Prostheis 1 Clinic Chair, belonging to the School of Dentistry, National Northeastern University during school year 2015. During interview, patients were instructed on the reason for the study, their authorization was then requested by means of an informed consent form.
In a brief clinical history, patient’ s personal data and history of bruxism, trauma, and TMJ or close areas’ surgery were recorded since they could have triggered TMJD.
A visual examination was then conducted where present status of remaining teeth and prosthetic area was established determining type of existing edentulousness according to Kennedy´s classification.
Maximum oral opening was measured with a milimeter ruler, recording distance between incisal edges of upper and lower central incisors. Openings ranging 53 to 58 mm were considered normal. In lower values ranges, end-feed test was conducted on top; this test is conducted when placing the thumb over upper incisors and index finger over lower incisors applying soft but constant pressure in order to try to passively increase inter-incisal distance. A soft end-feel is the case when the aforementioned increase could be achieved, it is generally assumed that in this case the etiology of restriction is muscular, a hard end-feel is when this target was not reached, in which case the origins belong to intra-capsular causes.
In order to observe oral opening symmetry, patients were observed from the front, they were requested to open and close without further commentaries, this is due to the fact that when patients were requested to open slowly or to a certain degree, they tried to control movements, interfering thus with their natural movements and altering results. Symmetry is preserved when the lower jaw descends following the sagittal line of the face during the whole movement. Mandibular deflection was considered when the jaw described a trajectory away from the midline as it progressed towards the opening, conversely closing, a deviation is considered when during oral opening the lower jaw moves away from the sagittal line up to a certain point, only to return to it with its progress; the inverse procedure would take place during closure.
In order to relate mandibular movements with pain, the patient was requested to report symptomatology in his own words, then, targeted questions were used to complete information on pain location, intensity, duration and origin.
After this, masticatory muscles’ palpation was undertaken (masseter, temporal, lateral pterygoid and medial pterygoid) sternocleidomastoid, posterior cervical muscles, as well as retro-distal region. Masseter muscles were bilaterally palpated at their upper and lower insertions by placing fingers on the cygomatic arches and moving them to the lower insertions located in the lower ridge of the mandible. Temporal muscles were palpated bimanually, respectively, above cygomatic arch, temporomandibular joint and external aspect of the skull. Tendon insertions at the coronoid apophyses were palpated by placing the finger of one hand within the mouth, at the anterior ridge of the ascending ramus, and the finger of the other hand in the same area outside of the mouth.
Palpation of lateral pterygoid muscles was conducted through functional manipulation, requesting the patient to perform a protrusion movement against resistance created by the operator, who exerted an anterior-posterior force at the level of the chin, for the medial pterygoid muscle, large cotton pads were placed in both arches, and the patient was instructed to bite onto them in order to assess presence of pain when performing these movements. Sternocleidomastoid muscles and posterior cervical muscles were simply palpated in order to ascertain presence of trigger points, describing these trigger points as foci of a deep painful stimulus which might cause central excitatory effects , that is to say, they will transmit pain to different regions, and in this case to the TMJ.
Finally, a bi-manual tactile exploration was conducted, (with index fingers simultaneously placed on the condyles) and TMJ auscultation by placing in the condylar zone the stethoscope´s great diaphragms (Rappaport, model BK3003, MELIPAL) (adult) on one side and then the other; the patient was then requested to perform lateral, protrusion, retrusion as well as opening and closing movements. Presence of noise was characterized according to sound, simple click was described as the sound perceived during jaw opening or closing, similar to the sound caused when replacing the lid of a highlighting pen. Nevertheless, when the same sound was found during opening and closing movements, it was called reciprocal click. Onset of a more intense and brusque freely heard noise was called pop, even to the point of bewildering auscultation operator. On the other hand, crepitation can be described as the crunchy noise created when rubbing two bricks. At a later point, coincidence of nose onset with pain was ascertained.
Frequency of articular noise onset in partially edentulous patients was determined with this examination, as well as characterization of different articular noises, most prevalent type of articular noise, presence or absence of painful symptomatology during noise onset, and relationship of articular noise presence with Kennedy´s classification.
Results
Out of the 5 patients recorded in clinical histories, 34 were female (68%) and 16 were male (32%).
Average oral opening was 42.4mm, with maximum 55 mm and minimum 28 mm.
Oral opening remained symmetrical in only 32% of cases, 50% of cases exhibited at least minimum deflection and the remaining 18% exhibited deviation.
Articular noise incidence was 48%.
Figure 1 exhibits found type of noise characterization, among which, 48.1% were simple clicks, 25.9% were reciprocal clicks, 18.5% were pop sounds, and 7.4% were crepitations. No preference was found for one particular side, sounds were fairly distributed between both articulations.
Articular sounds were proportionally more frequently found in females (47%) with respect to males (43%).
Clinical history revealed that 14% of total patients reported TMJ pain, six of them additionally reported articular pain in the affected articulation. Bearing in mind that a total of 24 patients with articular noises were recorded, it can be proposed that both temporomandibular disorder signs and symptoms coincided in 25% (Figure 2).
Fourteen per cent of total patients reported history of trauma, and 100% developed some sort of articular noise. Some even reported that onset of noise coincided with suffering trauma.
Only three patients reported having experienced a surgical intervention in zones surrounding TMJ. One of them reported a pop in the right temporomandibular articulation, after corrective surgery to treat lesions sustained during a car accident. One patient had been subjected to surgical interventions in both ears, and during palpation undertaken in opening movements, it was detected that both condyles abnormally «jumped» in an anterior-inferior direction, and that this was undetectable with the stethoscope.
Of all studied patients, 54% exhibited some sign/symptom of bruxism.
Nevertheless, in spite of the unequal distribution of the different Kennedy classes for each jaw, when adding obtained figures, it was found that, excepting class IV which was only recorded twice, all Kennedy classes were found to appear with almost with same frequency: 32 class I, 36 class II and 30 class III. Nevertheless, noise distribution was not so equitable (Table I).
Table I Noise distribution according to Kennedy class.
| Kennedy class | Simple click | Reciprocal click | Pop | Crepitation |
| I (12) | xxxx | xxxxx | xxx | |
| II (20) | xxxxxxxxxxxxxx | xxx | xxx | |
| III (21) | xxxxxxx | xxxxxx | xxxx | xxxx |
| IV (1) | x |
Thus, high incidence of simple clicks related to Kennedy´s class II were observed. In addition, in class III almost same amount of articular noises were recorded than in class II, but with a more balanced distribution.
Table II was drafted using the same method to relate TMJ without articular noises with Kennedy’ s classes.
Table II Kennedy class relationship without presence of articular noises.
| Kennedy class | TMJ without articular noises |
| I (21) | xxxxxxxxxxxxxxxxxxxxx |
| II (18) | xxxxxxxxxxxxxxxxxx |
| III (12) | xxxxxxxxxxxx |
| IV (1) | x |
Once class IV was discarded due to its low frequency, and considering both tables, it can be inferred that Kennedy’s class III is the lesser linked to articular noises, nevertheless, it must not be forgotten that in mandibular cinematic process two temporomandibular articulations come into play as well as two dental arches ,which might exhibit different total or partial edentulism pattern.
Most notable alterations observed were:
- Clearly decreased oral opening along with mandibular deviation.
- Presence of articular noises was bilateral in most cases.
- Noise was more frequently found in females.
- Presence of noise was not directly related to articular pain presence.
- High bruxism frequency in edentulous patients, especially in the posterior sector (class I and II).
Discussion
Okeson, after a long bibliographic recompilation of different epidemiologic studies, concluded that 50% of the world population exhibited at least one symptom of temporomandibular disorders, and that 20 to 30%16-19 exhibited noise or vibrations in the joint and approximately 41% exhibited painful symptoms. Studies20 conducted with 739 university students aged 18-25 years, revealed that 76% exhibited one or many signs associated to TMJD, nevertheless, only 26% of all students reported presence of one symptom related to these disorders. In other words, 50% of the group exhibited signs which had not been detected by the patient; it was also observed that only 10% exhibited symptoms that warranted a request for treatment.
Within local causes that can be responsible for TMJD, Ash, names occlusal interferences of support and ill-designed connectors of a removable dental prosthesis, which prevent centric occlusion and/or eccentric movements (laterality and protrusion). He achieved a bibliographic recompilation of influence of shortened dental arches, and he concluded that loss of all molars was compatible with aesthetics, but not with occlusal instability. There are studies where no increase of TMJD was found as long as all premolars were present:21 Nevertheless, other reports22-25 suggest that loss of posterior teeth may play an important role in the demise of the temporomandibular joint.
Sadowsky26 determined that extraction of premolars for orthodontic reasons increases onset of articular noises, but these do not necessarily cause problems that would warrant alterations in TMJ’s normal functioning.
An interesting datum is provided by a study where it was determined that 21.4% of subjects with ages ranking 15-54 years used prostheses; in the group 55-64 years old, they wore removable partial dentures. Among partially edentulous subjects who did not wear prostheses, the probability that missing teeth were on the lower jaw was six times higher than for the upper jaw. Conjunction of this study and those which highlighted relationship between absence of teeth and temporomandibular disorders fosters the increase of preventive and conservative measures of oral/dental health and hygiene. Therefore, loss of more than five teeth, especially in the posterior area, is a characteristic present in patients with some sort of TMJD. This last characteristic was present in most recorded patients, since Kennedy’s classes I, II and III represented 98% of all cases found in the studied population.
Teran and others conducted research on prevalence of functional disorders of the masticatory system in edentulous patients. Obtained results showed values somewhat higher to those found in the present study. According to this study, 67% of studied population presented signs of temporomandibular disorders, 56% exhibited articular sounds when opening and closing, mainly click sounds (21-26%)
On the other hand, Hittunen et al in the University of Helsinki studied occlusal unbalance and its relation to TTM in elderly patients suffering loss of tooth support. They classified cases according to area of the mouth and severity of tooth loss, and found no relationship between seriousness of TMJD and loss of dental support, they further observed lack of improvement with use of prostheses. Findings by Ortega showed significant tendency among greater number of lost teeth and TMJD frequency in healthy control patients. Loss of posterior dental support.
Loss of posterior dental support might favor greater TMJD incidence due to greater condyle mobility and posterior contraction of masticatory musculature. Nevertheless, although this association was significant among healthy control patients, no clear tendency was found to relate an increase of TMJD with greater number of lost teeth.
The complex biomechanics of the lower jaw forces both temporomandibular articulations to simultaneously and coordinately develop different activities with what Alonso calls «dental articulation». Many authors mention that this is the cause for TMJ alterations, nevertheless, not all patients suffer them.
Presently, it is believed that origins of temporomandibular disorders are of a multi-factorial nature. Okeson proposed that there are five factors associated to this type of condition: trauma, emotional stress, deep pain, parafunctional activities and occlusal circumstances (absence of teeth, premature contacts, poor tooth alignment, etcetera).
Conclusion
With the present research project it is concluded that temporomandibular alterations and noises present in the articulation are more frequently found in patients suffering edentulousness in the posterior areas of the jaw as well as patients within Kennedy’ s class I and II classification, where presence of noises was ascertained during auscultation.
We consider that all human beings are naturally endowed with two temporomandibular joints and two dental arches, therefore, it is inappropriate, able and complex, to directly relate one particular Kennedy class with the presence of a particular type of articular noise. This is due to the fact that one single patient might exhibit different Kennedy classes in each jaw and can thus present different articular noises in each articulation.
Rehabilitation shortly after edentulous stage allows better recovery of the chewing muscles, wich during the contraction bring the condyle to a more posterior and superior position in relation to the glenoid cavity, helping to preserve some functional aspects of the occlusion, and decreasing the possibility of TTM development.
Four traits were found in edentulous patients, which frequently appear in TMJD patients and are rare in the other group: presence of skeletal anterior open bite, sliding from retruded contact position to upper maximum intercuspation at 2 mm and absence of five or more posterior teeth. This last characteristic was present in most recorded patients, since Kennedy’s classes I, II and III constituted 98% of studied population cases.
Loss of posterior dental support could favor greater incidence of TMJD by increasing condyle mobility and later contraction of masticatory muscles. Nevertheless, no clear trend was found to relate increase of TMJD with greater number of lost teeth.
Referencias
1. Winkler S. Prostodoncia total. México: Editorial Limusa Noriega Editores, 2001, pp. 25-26, 554-555. [ Links ]
2. Okeson J. P. Tratamiento de oclusión y afecciones temporomandibulares. 5ta edición. España: Editorial Elsevier, 2003, pp. 147-364. [ Links ]
3. Perea PB. Patología de la articulación temporomandibular (ATM). En: IV Jornadas sobre valoración del daño corporal. Ed. Mapfre. Madrid. 2005. [ Links ]
4. Pullinger AG, Seligman DA. The degree of which attrition characterizes differentiated patient groups of temporomandibular disorders. J Orofac Pain. 1993; 7 (2): 196-208. [ Links ]
5. McGrusson T. Etiología, diagnóstico y tratamiento del síndrome temporomandibular. Quintessense. 2003; 16 (1): 56-59. [ Links ]
6. Santos R. Terapias alternativas para desórdenes temporomandibulares. Rev Cubana Estomatol. 2002; 17 (36): 187-192. [ Links ]
7. Ohashi E, Paredes D, Balarezo JA. Análisis de los factores articulares para el diagnóstico de los desórdenes temporomandibulares en adultos jóvenes. Rev Estomatol Herediana. 2002; 12 (1-2): 15-20. [ Links ]
8. Sadowsky C, Muhl ZF, Sakols EI, Sommerville JM. Temporomandibular Joint Sounds related to orthodintic therapy. J Dent Res. 1983; 64: 1392. [ Links ]
9. Tallents RH, Catania J, Sommers E. Temporomandibular join findings in pediatric populatons and young adults: a critical review. Angle Orthod. 1991; 61 (1): 7-16. [ Links ]
10. Wabeke KB et al. Clicking: a literature overview. J Cranio Disord Facial Oral Pain. 1989; 3: 163. [ Links ]
11. Clark GT, Solberg WK. Perspective of temporomandibular disorders. Temporomandibular and Facial Pain Clinic, UCLA Dental Center. Chicago, Quintessence Plishing Co. 1987. [ Links ]
12. Solber WK, Woo MW, Houston JB. Prevalence of mandibular dysfunction in young adults. J Am Dent Assoc. 1979; 98 (1): 25-34. [ Links ]
13. Alonso AA, Albertini JS, Bechelli AH. Anatomía aplicada a la articulación tempormandibular. En: Alonso AA, Albertini JS, Bechelli AH. Oclusión y diagnóstico en rehabilitación oral. Editorial Médica Panamericana. Argentina, 2000. [ Links ]
14. Campos A. Oclusión y articulación temporomandibular. En: Campos A. Rehabiltacion oral y oclusal. Vol. I. Editorial Harcourt. Madrid, 2000. [ Links ]
15. Vartan B. Disfunciones del sistema estomatognático. En: Behsnilian V. Oclusión & Rehabilitación. Uruguay, 1971. [ Links ]
16. Dawson PE. Diagnóstico diferencial del síndrome temporomandibular. En: Dawson PE. Evaluación, diagnóstico y tratamiento de problemas oclusales. Editorial Mundi SAIC y F. Argentina, 1977. [ Links ]
17. Laerreta JA. Factores etiológicos de las patologías intraarticulares. En: Learreta JA. Compendio sobre diagnóstico de las patologías de la ATM. Editorial Artes Médicas Ltda. Brazil, 2004. [ Links ]
18. François R. Tratado de osteopatía craneal. Articulación temporomandibular análisis y tratamiento ortodóntico. Segunda edición. Editorial Médica Panamericana. Madrid, 2005, pp. 900. [ Links ]
19. Echeverry GE, Kovalski GS. Disfunción de la articulación temporomandibular. En: Echeverry E. Neurofisiología de la oclusión. Editorial Monserrate LTDA. Bogotá, 1993. [ Links ]
20. Ash MM, Ramfjord S. Trastornos de la oclusión y disfunción del sistema masticatorio. En: Major M, Sigurd R. Oclusión. Editorial McGraw-Hill Interamericana de México, 1996. [ Links ]
21. Käyser AF. Shortened dental arches and oral function. J Oral Rehabil. 1981; 8: 457-462. [ Links ]
22. Witter DJ, Van Elteren P, Käyser AF. Sing and symptoms of mandibular disfuntion in shortened dental arches. J Oral Rehabil. 1988; 15 (5): 413-420. [ Links ]
23. Budz-Jorgensen E, Luan W, Holm-Pedersen P, Fejerskov O. Mandibular dysfunction related to dental, oclusal and prosthetic condition in a señected erderly population. Gerodontics. 1985; 1: 28-33. [ Links ]
24. Kononen M, Wenneberg B, Kallenberg A. Craniomandibular disord in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. A clinical study. Acta Odontol Scand. 1992; 50 (5): 281-287. [ Links ]
25. Shcolte AM, Steenks MH, Bosman F. Characteristics and treatment outcome of diagnostic subgroup of CMD patient: retrospective study. Community Dent Oral Epidemiol. 1993; 21 (4): 215-220. [ Links ]
26. Sadowsky C. The risk of orthodontic treatment for producing temporomadibular disorders: a literature review. Am J Orthod Dentofacial Orthop. 1992; 101 (1): 79-83. [ Links ]
27. Carr A, McGivney G, Brown D. Epidemiología, fisiología y terminología del edentulismo parcial. En: McCracken. Prótesis parcial removible. Un décima edición. 11a. Ed. Editorial Elsevier Mosby. España, 2006. [ Links ]
Received: August 2017; Accepted: October 2017











 text in
text in