Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.22 no.2 Ciudad de México abr./jun. 2018
Original research
Epidemiological profile of ameloblastoma affected patients subjected to surgery at a tertiary hospital in the state of Sao Paulo
* Mandaqui Hospital Compound, Sao Paulo, Brazil.
§ Faculty of Dentistry, University of Sao Pablo, Brazil. Institute of Nuclear and Energy Research (PEN/CEN), University of Sao Paulo, Brazil.
Ameloblastoma is a locally invasive, odontogenic tumor of difficult early diagnosis. Treatment can vary from simple enucleation, enucleation associated to curettage and/or cryotherapy up to extensive surgical resections. The present study used epidemiological data of patients such as name, age, gender, type of ameloblastoma, region and type of treatment. Aforementioned data were collected from clinical histories of patients treated at the Mandaqui Hospital Compound during the period 01/01/ 2010 to 08/30/2016. Data were transcribed for the forms used every day in hospital, and were presented in tables and graphs. Out of 11 selected clinical histories, six patients were male and five female, average age was 32 years. According to collected data, mandibular region was the most compromised (91%). Radiographically, the most frequently image was multilocular (64%), presence of single-cyst ameloblastoma was detected in four cases (36%). In three cases (27%) treatment consisted on decompression followed by curettage, in one case (9%) segmented resection was performed, in two cases (18%), segmented resection followed by reconstruction was achieved, in three cases (27%) enucleation followed by curettage, in two cases (18%), curettage and application of Carnoy solution. Maximum follow up period was five years, no recurrence was observed in that period, nevertheless, there was follow up loss in these patients. Based on data obtained from studied population, it was concluded that average age varied from 10 to 66 years, mean age 32 years; on the other hand, male gender was the most compromised (55%), multilocular lesions were the most frequently found lesions (64%). Finally the most affected mandibular area was the posterior region of the lower jaw (73%), most frequent type of treatment was debridement (27%).
Key words: Ameloblastoma; ameloblastoma surgery; ameloblastoma treatment
El ameloblastoma es un tumor odontogénico localmente invasivo cuyo diagnóstico precoz es difícil. El tratamiento puede variar desde una enucleación simple, una enucleación asociada a curetaje y/o crioterapia hasta amplias resecciones quirúrgicas. En este presente estudio se utilizaron los datos epidemiológicos de los pacientes tales como nombre, edad, género, tipo de ameloblastoma, región y tipo de tratamiento. Éstos fueron colectados a partir de las historias clínicas de los pacientes tratados en el Conjunto Hospitalar del Mandaqui durante el periodo de 01/01/2010 al 30/08/2016. Los datos fueron transcritos para el formulario usado cotidianamente en el hospital y presentados en tablas y gráficos. De las 11 historias clínicas seleccionadas, seis pacientes pertenecían al sexo masculino y cinco al sexo femenino, con un promedio de edad de 32 años. La región mandibular fue la más comprometida según los datos recolectados (91%). Radiográficamente, la imagen visualizada en una mayor frecuencia fue la multilocular (64%), y por otro lado, la presencia del ameloblastoma uniquístico fue detectada en cuatro casos (36%). El tratamiento consistió en la descompresión seguida de curetaje en tres casos (27%), resección segmentar en un caso (9%), resección segmentar seguida de reconstrucción en dos casos (18%), enucleación seguida de curetaje en tres casos (27%), curetaje y aplicación de solución de Carnoy en dos casos (18%). El periodo máximo de acompañamiento fue de cinco años, no presentándose recidiva en este periodo; sin embargo, hubo pérdida de acompañamiento de estos pacientes. Con base en los datos obtenidos en la población estudiada, se concluyó que la edad promedio varió de 10 a 66 años con una media de 32 años; por otro lado, el sexo masculino fue el más comprometido correspondiendo al 55% de la muestra, siendo el tipo radiográfico de la lesión más encontrado el multilocular (64%). Finalmente, el área mandibular más afectada fue la región posterior de la mandíbula (73%) y el tipo de tratamiento con mayor prevalencia fue el desbridamiento (27%).
Palabras clave: Ameloblastoma; cirugía de ameloblastoma; tratamiento del ameloblastoma
Introduction
Odontogenic tumors are lesions derived from the oral epithelium and/or ectomesenchyme of teeth’s development components or associated structures; they represent barely 1% of all tumors found in the mandible.1 Ameloblastoma is one of the most common benign odontogenic neoplasia affecting upper and lower jaws. It is a locally invasive tumor of uncertain epithelial origin, representing close to 14% of all cysts and tumors of the mandible; it is more prevalent in developing countries.2
Decades ago, researchers tried to uncover the real origin of this neoplasia, presently, studies indicate the possibility that this tumor might originate from cell remnants of the enamel organ, of epithelial lining of odontogenic cysts and possibly from epithelial cells in the basal stratum of the oral mucosa.3-5
According to their clinical and radiographic characteristics, ameloblastoma can be classified into three subtypes: they can be solid or multi-cystic, single-cystic or peripheral. When emitting diagnoses, subtypes must be recognized and differentiated, since diagnosis and treatment will depend according to the different types.6
Most common histopathological patterns are follicular and plexiform. The least common are the acanthomatous, of granular cells, dermoplastic and basal cell patterns.7
According to their characteristics, tumors can infiltrate within trabeculate bone and thus compromise the whole extension. This type of tumor is generally diagnosed when an oral and cortical expansion is detected, causing facial asymmetry. In this last condition, bone structure is already partially compromised, thus limiting conservative treatments, leaving few options other than removing great sections of affected bone structure so as to avoid recurrence; this type of lesions are thus candidates for radical treatments.8
Within established treatments, two schools can be identified: conservative and radical schools. Conservative school treats the patient by removing all the lesion, nevertheless decreasing the possibility of performing extensive mutilations. Within proposed treatments we can count, among others, the following: simple enucleation, enucleation associated to curettage, enucleation associated to cryotherapy, surgical extraction by means of osteotomy, marsupialization associated to enucleation, among others.
Conservative treatment approach to treat ameloblastoma ranks it as a benign condition to be treated accordingly. Thus, even though the possibility of tumor recurrence remains latent, in principle, surgical rescue is possible, and most cases success can be achieved without great mutilations. On the other hand, the radical school defends the objective of total lesion removal with free security margins, thus removal is conducted through segment or bloc resection, trying to achieve a final solution at the first and hopefully only, surgical intervention.
This behavior is supported by the fact that ameloblastoma turn into infiltrative and destructive lesions. The fact that the biological character of some types of ameloblastoma is associated to high recurrence levels, becomes a solid argument for the surgeon to undertake a more radical posture with respect to treatment.9
The present study had the purpose of conducting an epidemiological count of ameloblastoma afflicted patients, subjected to tumor removal surgery in a tertiary hospital of the city of Sao Paulo, Brazil.
Material and methods
The present study was subjected and approved by the Ethics Committee at the Research Center of the Mandaqui Hospital, northern region of Sao Paulo, with final approval number 61144616.1.0000.5551.
Data collection with respect to patient’s name, age, gender, and type of ameloblastoma, as well as topography and treatment type, were based on clinical histories of surgically treated patients, during the timeframe 01 January 2010-30 August 2016. Data were transcribed for the pathology questionnaire devised for this research project. After data analysis, information was presented in tables and graphs.
Study population and sample were formed by patients with initial ameloblastoma diagnosis, who attended the facilities in search of treatment, as well as clinical histories of ameloblastoma patients who were treated within the timeframe of 01 January 2010 to 30 August 2016.
Inclusion criteria for patient selection were the following:
Patients with ameloblastoma diagnosis who had been operated at the SUS (Single Health System, Sao Paulo, Brazil).
Suitably completed clinical histories of patients.
Patients who received postoperative follow-up for at least a year.
Patients who agreed with and signed an informed consent form to participate in the present study.
Data were collected according to aforementioned collecting instruments, with information deemed relevant to the study. Data were made available at a later point in the manner of graphs.
Results
Based on data collected from all patients, epidemiological analysis of all information was conducted according to the following variables considered in the present study. Figure 1 shows percentages of patients with ameloblastoma attending the Mandaqui Hospital Compound during January 2010-august 2016 according to patient’s gender.
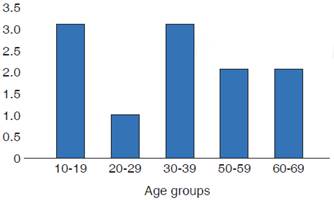
Figure 2 shows patient distribution according to age; higher prevalence was found for the 10-19 years age group, and 30-39 years group, with less compromise in the group 50-69 years, followed by the 20-29 years group.
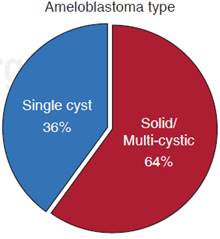
With respect to radiographic pattern of ameloblastoma visualized in x ray analysis, it was found that solid or multi-cystic subtype was most frequent, affecting 64% of evaluated population. On the other hand, single-cyst ameloblastoma was found in almost 36% of the sample. This information is shown in Figure 3.
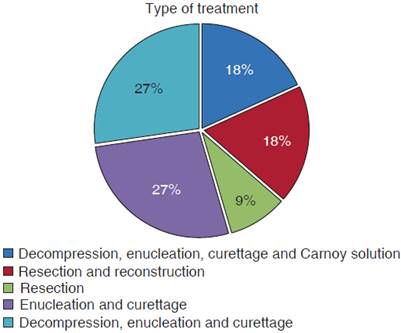
With respect to applied treatment, it was observed that 27% of cases were treated with decompression, enucleation and curettage of lesions; 27% were treated with enucleation of lesion and curettage, resection with reconstruction was found in 18% of cases, as was the case of the combined use of decompression, enucleation, curettage associated to use of CARNOY solution (18%). Treatment performed with only lesion resection was observed in 9% of cases (Figure 4).
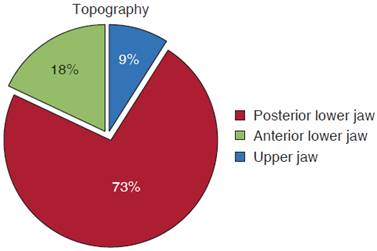
With respect to lesion implantation site, it was observed that 73% of all cases were detected in the posterior section of the lower jaw, 18% located at the anterior region of the mandible and 9% of all cases were found in the upper jaw, as shown in Figure 5.
Discussion
Ameloblastoma is the odontogenic neoplasia with greatest clinical significance due to its prevalence, clinical behavior and treatment difficulty, as well as controversies related to lesion treatment.3-5
According to the present study, and bearing in mind its inherent limitations, it was impossible to expose in accurate quantities the condition’s evolution time, this same situation was presented in a former study.10
Tumors’ own characteristics can be described as exhibiting slow and progressive growth, generally asymptomatic, and with the ability of causing marked facial deformities.
Although it is difficult to determine an exact initial time of lesion development, facial alterations occur only after bone marrow is compromised and advanced expansion of bone cortical plates,10 these characteristics were confirmed by the surgical team operating in the hospital of the present study.
According to most recent literature reports with respect to ameloblastoma prevalence in patients according to gender is still controversial. Some authors do not find differences in neoplasia incidence according to gender.11,12 Nevertheless, according to formerly conducted research projects,12,13 this condition is more prevalent in females. In the present study, a 56% male prevalence was found concurring with results of previous studies.12,14,19 Reviewed literature did not report evidence of patient’s gender predilection, thus a non existence of biological correlation could be established between presence of tumor and affected gender.
With respect to age group, patients’ ages ranged from 10-66 years, with average of 32 years. Most prevalent age groups were first and third decade of life, these data concurred with previous studies.12,14-17,20-22 This finding seems to exhibit direct association with tumors aggressiveness and deformation caused by them. As was mentioned before, ameloblastoma, within its main characteristics, exhibits slow and painless growth, in some cases, its presence is only noticed after expansion of bone cortical plates, and in consequence, will cause volume increase in the compromised region as well as decurrent facial asymmetry. Diagnosis in the first decade of life is related to accelerated growth, expansive tumors,23 on the other hand, tumors in the third decade of life exhibit slow and less expansive growth. Nevertheless, they are not infrequently found at more advanced ages such as the fifth decade of life.
Literature reports manifested unanimity when stating that ameloblastoma’s most frequent location was the lower jaw, mainly in the posterior section. An exception to these findings is a study described by Chidzonga24 who described the symphyses as the ameloblastoma main affected region in African children. In the present research and according to reviewed and analyzed clinical histories, a greater number of cases with lower jaw compromise was found, with a total of 10 clinical histories (91%), on the other hand, only one case was found for the upper jaw (9%). These findings concurred with literature reports.14,15,20
Radiographically, ameloblastoma appear as a radiolucid, unilocular or multilocular, expansive lesions, frequently exhibiting cortical bone plate fenestrations. Involved teeth are normally displaced, and routinely exhibit root resorption, more so than in other lesions affecting the jaws. According to reviewed and analyzed clinical histories, radiographic characteristics of patients in the present study revealed that most lesions represented by seven cases (64%) exhibited multilocular aspect, and four cases (36%) belonged to the unilocular type. Similar results were found in another study.16 Recent literature confirms prevalence of multilocular imaginological roster when compared to unilocular findings.11,14
As reported in recent literature, treatment of ameloblastoma is a very controversial and discussed subject. There are two main trends with respect to the therapeutic approach to treat these lesions. Radical treatment supports bloc resection of the tumor with a security margin, so that that there be no exposition of tumor cells to the surgical field, this technique elicits the possibility of causing a continuity defect in the mandibular bone. On the other hand, the conservative treatment is based on tumor resection with maximum preservation of underlying bone; this technique can be (or not) associated to adjuvant therapies.5
Conservative treatment consists of a surgical approach with lesser morbidity rate. Nevertheless recurrence rate tends to be higher in this group of patients,6 notwithstanding, when this recurrent lesion appears, surgical approach tends to be of lesser proportions, which would justify use of this treatment philosophy , encouraging surgeons to be more conservative, with a rigorous follow-up of operated patients.17
The present study consisted on a review of clinical histories of patients with initial ameloblastoma diagnosis treated by the Buccal-Maxillary-Facial Trauma and Surgery team of the Mandaqui Hospital Complex (northern region of the city of Sao Paulo, Brazil). In this study a clear trend towards choice of conservative treatment was observed as initial therapy for ameloblastoma. Out of the 11 analyzed clinical histories, a sample was found in which three cases (27%) of patients were treated with marginal and segment resection; on the other hand, eight cases (73%) were treated following conservative technique. If we bear in mind that in the present study conservative technique consisted in: simple lesion enucleation, curettage-associated enucleation, cryotherapy associated enucleation, surgical exeresis through conservative osteotomy, marsupialization associated to enucleation. Only one case (9%) was associated to conservative technique with joint application of Carnoy solution.
Since it was the initial treatment mode, average follow-up time of these patients (69.6 months) was longer than that observed for the curettage group (55.5 months). During follow-up of these patients, it was observed that, in spite of an apparent low recurrence rate, many local complications occurred simultaneously, probably associated to cryotherapy. Within these complications formation of bone sequestration, pathological fracture of the lower jaw, and one case of osteomyelitis were noticed.
Among adjuvant preoperative treatments, marsupialization of extensive cystic tumors was undertaken. This approach, substantiated and defended in literature18,25 was executed on bone neoformation, which could induce individualization of alveolar nerve underneath the tumor as lesion size decreased.
Previously conducted research projects10,25 highlighted the importance of avoiding mandibular resections in children, due to resulting future esthetic, functional and psychological alterations. Conservative resection, preceded (or not) by decompression must be treatment of choice, as long as there is a possibility of patient follow-up.
The present study included three cases of patients in growth phase, therefore, treatment of choice was decompression followed by enucleation and curettage; treatment elicited initial tumor regression from the moment of decompression as well as preservation of the mandibular skeleton, thus decreasing surgical damage related to function and development of the maxillary- mandibular complex.
Mandibular resection is the ameloblastoma treatment usually recommended by different authors, especially in lesions that cause destruction of bone cortical plates surrounding the mandibular ramus.11,14,26,27 Security margin advocated for resection varies from 1 to 3 cm in healthy bone.14,21 Sachs28 considered that, in order to obtain this margin, barely small lesions could be treated without causing mandibular discontinuity, and that presence of cortical plate seems to be the most important factor in terms of anatomical barrier when compared to the distance itself. For Nakamura18 this approach is usually indicated, but is nevertheless associated to important esthetic and functional sequels, especially in children. In the present project, three cases of total resections were studied. In two cases there was resection followed by reconstruction. It must be considered that quality of life and stomatognathic system function will result clearly damaged when suitable reconstruction is not undertaken. On the other hand, there is the need for a surgical team with wide extensive expertise and training to suitably proceed in reconstruction cases, since it is considered that,28 in addition to ameloblastoma subtype and its biological behavior, criteria to be considered for accurate therapeutic and surgical plans are the following: diagnosis, patient’s age, size of lesion and anatomical location.
Conclusion
Based on obtained results of the present study, it was concluded that male gender was most affected representing 55% of assessed cases. Moreover, with respect to age, this type of lesion was found in an age range of 10-66 years, with average age of 32 years; this would correspond to prevalence of age group in the third decade of life. Most prevalent X ray image pattern of the lesion was multilocular, mainly located at the posterior section of the mandible, representing 73% of studied population. Finally, most frequent treatment performed in this hospital for ameloblastoma patients was enucleation followed by curettage, representing 27% of studied cases. Conservative treatment of these lesions was highlighted so as to increase patient’s quality of life after surgery.
Referencias
1. Gupta S, Sexana S, Bhagwat S, Aggarwal P, Gupta PK. Clinicopathological characteristics of ameloblastomas in Western Uttar Pradesh population: An institutional study. Indian J Cancer. 2015; 52 (1): 57-60. [ Links ]
2. Oginni FO, Stoelinga PJ, Ajike SA, Obuekwe ON, Olokun BA, Adebola RA et al. A prospective epidemiological study on odontogenic tumours in a black African population, with emphasis on the relative frequency of ameloblastoma. Int J Oral Maxillofac Surg. 2015; 44 (9): 1099-1105. [ Links ]
3. Neville BW. Patologia oral e maxilofacial. Rio de Janeiro: Guanabara Koogan; 1998: p. 711. [ Links ]
4. Campos GM. Ameloblastoma, a behavioral and histologic paradox. Braz Dent J. 1990; 1 (1): 5-15. [ Links ]
5. Gomes ACA, Dias E, Gomes DO, Paraíso DP, Nascimento GJF, Cabral RAA. Ameloblastoma: tratamento cirúrgico conservador ou radical? Rev Cir Traumatol Buco-Maxilo-Fac. 2002; 2 (2): 17-24. [ Links ]
6. Ferretti C, Polakow R, Coleman H. Recurrent ameloblastoma: report of 2 cases. J Oral Maxillofac Surg. 2000; 58 (7): 800-804. [ Links ]
7. Neville BW, Damm DD, Allen CM, Bouquot JE. Cistos e tumores odontogênicos. Rio de Janeiro: Guanabara Koogan; 2004; Cap. 15, pp. 566-616. [ Links ]
8. Montoro JRMC, Tavares MG, Melo DH, Franco RL, Mello-Filho FV, Xavier SP et al. Ameloblastoma mandibular tratado por ressecção óssea e reconstrução imediata. Rev Bras Otorrinolaringol. 2008; 74 (1): 155-157. [ Links ]
9. De Souza-Kruschewsky L, Cincurá C, Alves-Teixeira F, De Mello-Filho FV. Ameloblastoma: aspectos clínicos e terapêuticos. Rev Bras Cir Craniomaxilofac. 2010; 13 (4): 241-245. [ Links ]
10. Al-Khateeb T, Ababneh KT. Ameloblastoma in young Jordanians: a review of the clinicopathologic features and treatment of 10 cases. J Oral Maxillofac Surg. 2003; 61 (1): 13-18. [ Links ]
11. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995; 31B (2): 86-99. [ Links ]
12. Sampson DE, Pogrel MA. Management of mandibular ameloblastoma: the clinical basis for a treatment algorithm. J Oral Maxillofac Surg. 1999; 57 (9): 1074-1077; discussion 1078-1079. [ Links ]
13. Arotiba JT, Ogunbiyi JO, Obiechina AE. Odontogenic tumours: a 15-year review from Ibadan, Nigeria. Br J Oral Maxillofac Surg. 1997; 35 (5): 363-367. [ Links ]
14. Olaitan AA, Adeola DS, Adekeye EO. Ameloblastoma: clinical features and management of 315 cases from Kaduna, Nigeria. J Craniomaxillofac Surg. 1993; 21 (8): 351-355. [ Links ]
15. Poon CSP, Wu PC, So MKP. Ameloblastoma in Hong Kong Chinese. Hong Kong Med J. 1996; 2 (2): 172-176. [ Links ]
16. Bataineh AB. Effect of preservation of the inferior and posterior borders on recurrence of ameloblastomas of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90 (2): 155-163. [ Links ]
17. Kim SG, Jang HS. Ameloblastoma: a clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91 (6): 649-653. [ Links ]
18. Nakamura N, Higuchi Y, Mitsuyasu T, Sandra F, Ohishi M. Comparison of long-term results between different approaches to ameloblastoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93 (1): 13-20. [ Links ]
19. Siar CH, Lau SH, Ng KH. Ameloblastoma of the jaws: a retrospective analysis of 340 cases in a Malaysian population. J Oral Maxillofac Surg. 2012; 70 (3): 608-615. [ Links ]
20. Curi MM, Dib LL, Pinto DS. Management of solid ameloblastoma of the jaws with liquid nitrogen spray cryosurgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84 (4): 339-344. [ Links ]
21. Martins RH, Andrade Sobrinho J, Rapoport A, Rosa MP. Histopathologic features and management of ameloblastoma: study of 20 cases. Sao Paulo Med J. 1999; 117 (4): 171-174. [ Links ]
22. Hong J, Yun PY, Chung IH, Myoung H, Suh JD, Seo BM et al. Long-term follow up on recurrence of 305 ameloblastoma cases. Int J Oral Maxillofac Surg . 2007; 36 (4): 283-288. [ Links ]
23. Gardner DG, Pecak AM. The treatment of ameloblastoma based on pathologic and anatomic principles. Cancer. 1980; 46 (11): 2514-2519. [ Links ]
24. Chidzonga MM. Ameloblastoma in children. The Zimbabwean experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 81 (2): 168-170. [ Links ]
25. Takahashi K, Miyauchi K, Sato K. Treatment of ameloblastoma in children. Br J Oral Maxillofac Surg. 1998; 36 (6): 453-456. [ Links ]
26. D’Agostino A, Fior A, Pacino GA, Bedogni A, Santis D, Nocini PF. Retrospective evaluation on the surgical treatment of jaw bones ameloblastic lesions. Experience with 20 clinical cases. Minerva Stomatol. 2001; 50 (1-2): 1-7. [ Links ]
27. Carlson ER, Marx RE. The ameloblastoma: primary, curative surgical management. J Oral Maxillofac Surg. 2006; 64 (3): 484-494. [ Links ]
28. Sachs SA. Surgical excision with peripheral ostectomy: A definitive, yet conservative, approach to the surgical management of ameloblastoma. J Oral Maxillofac Surg. 2006; 64 (3): 476-483. [ Links ]
Received: July 2017; Accepted: September 2017











 texto en
texto en