Services on Demand
Journal
Article
Indicators
Related links
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.21 n.3 Ciudad de México Jul./Sep. 2017
Original works
Periodontal disease and its relationship with clinical and sociodemographic variables in adult patients treated in a service/teaching institution
1 School of Dentistry, University of Antioquia, Medellin, Colombia.
Objective:
To determine prevalence of periodontal disease and related clinical and sociodemographic factors.
Material and methods:
An observational, descriptive and retrospective study was undertaken. Criteria to select patients were as follows: ≥ 35 years of age, full clinical history and periodontal chart and a minimum of ten teeth present in the mouth. Clinical periodontal and sociodemographic variables were examined; periodontal diagnosis was established according to two classification systems (AAP and CDC-AAP). χ2 was calculated in order to analyze differences among sociodemographic and clinical variables with respect to periodontitis severity. Median test was used for quantitative variables.
Results:
Periodontitis frequency was 67.2% (severe periodontitis 43.2%). Gingivitis frequency was 32.8%. In 155 cases there was concordance of two observers in cases of severe periodontitis. CDC-AAP classification established more cases of moderate periodontitis and only 47 cases in concordance with AAP system. Periodontitis patients exhibited greater bleeding upon probing, insertion loss and periodontal pockets (p < 0.001). Patients with periodontitis lost more teeth that patients with gingivitis. Periodontitis was more frequent in males than in females (p = 0.025). Patients with periodontitis exhibited lower educational levels, suffered systemic diseases, were addicted to tobacco and alcohol use and had encountered problems with their affiliation to social security services.
Conclusions:
Periodontitis frequency in studied population was high (60%), and found to be related to systemic diseases, tobacco use, affiliation to social security services and educational level. Periodontitis frequency was determined by used classification system.
Key words: Periodontitis; gingivitis; sociodemographic variables; tobacco use; diabetes; education
Objetivo:
Determinar la prevalencia de enfermedad periodontal y los factores sociodemográficos y clínicos relacionados.
Material y métodos:
Se diseñó un estudio observacional, descriptivo y retrospectivo. Se incluyeron historias clínicas con los siguientes criterios: ≥ 35 años de edad, historia clínica y ficha periodontal completa y mínimo 10 dientes presentes en boca. Se analizaron variables sociodemográficas y clínicas periodontales y se estableció el diagnóstico periodontal de acuerdo con dos sistemas de clasificación (AAP y CDC-AAP). Se calculó el χ2 para analizar las diferencias entre variables sociodemográficas y clínicas con relación a la severidad de la periodontitis. Para variables cuantitativas se utilizó la prueba de la mediana.
Resultados:
La frecuencia de periodontitis fue 67.2% (periodontitis severa 43.2%) y gingivitis fue 32.8%. En 155 casos hubo acuerdo entre las dos clasificaciones cuando la periodontitis fue severa. La clasificación CDC-AAP produjo más casos de periodontitis moderada y sólo 47 casos en concordancia con el sistema AAP. Los pacientes con periodontitis presentaron mayor sangrado al sondaje, pérdida de inserción y bolsas periodontales (p < 0.001). Los pacientes con periodontitis perdieron más dientes que pacientes con gingivitis. La periodontitis fue más frecuente en hombres que en mujeres (p = 0.025). Los pacientes con periodontitis tuvieron un nivel educativo más bajo, enfermedades sistémicas, consumo de cigarrillo y alcohol y problemas de afiliación a la seguridad social.
Conclusiones:
La frecuencia de periodontitis en la población de estudio fue muy alta (60%) y se encontró relacionada con enfermedades sistémicas, cigarrillo, afiliación a la seguridad social y nivel educativo. La frecuencia de periodontitis se ve determinada por el sistema de clasificación que se utilice.
Palabras clave: Periodontitis; gingivitis; variables sociodemográficas; cigarrillo; diabetes; educación
INTRODUCTION
The fact that plaque accumulation around teeth results in periodontal disease is universally accepted. Among these diseases, gingivitis (G) is very frequent, and can reach prevalence of over 70% in young subjects.1 On the other hand, chronic periodontitis (CP) approximately affects 47% of North America's adult population.2 Unlike gingivitis, CP can be sub-classified according to the degree of severity found in insertion loss. Bearing this parameter in mind, it is possible to see that moderate CP (30%) is the most frequent, followed by mild (8.7%) and severe (8.5%) degrees. Worldwide, severe CP is approximately 11%.3 In Colombia CP prevalence is 61.8%, moderate CP being the most prevalent (43.4%).4 This shows the magnitude of the problem found in the population, and thus it can be concluded that, although not all subjects suffer severe chronic periodontitis, there are other factors, different from bacterial plaque, which might affect this disease's progress.
Although bacterial plaque is a necessary factor, it is not sufficient for the development of periodontal disease. Other factors such as age, systemic conditions -an possible drugs used or consumed for treatment of these conditions- educational level, habits such as tobacco or alcohol consumption, as well as socioeconomic status play a determining role in the development of periodontal disease. Thus it has been suggested that periodontal disease is more frequent in low income and low education populations with restricted access to health services. Likewise, it has been observed that CP prevalence increases with age.5,6,7
The School of Dentistry of the University of Antioquia is an institution forming individuals in oral health. Under a teaching-service model, in the different undergraduate and graduate clinics, it treats subjects of different socioeconomic levels and backgrounds. This represents an ideal context to achieve characterization of determinant factors associated to periodontal disease, with the aim of propose strategies based on comprehensive treatment in social reality and found requirements.
Bearing the aforementioned in mind, this study purported the objective of determining prevalence of periodontal disease and related clinical and sociodemographic factors found in population treated at this institution in the period 2011-2016.
MATERIAL AND METHODS
A retrospective, descriptive and observational study was designed. Anonymity of information included in clinical histories was guaranteed; it was considered a risk-free study since it was a data secondary analysis. The research project was approved by the Bioethics Committee of the School of Dentistry. University of Antioquia (Affidavit No 6, 2014).
Clinical histories of the Faculty's files dated 2011-2016 were reviewed, only files meeting the following criteria were included: patients aged ≥ 35 years, full clinical history and periodontal chart, presence of at least 10 teeth in the mouth excluding third molars. In order to obtain sociodemographic information. A form with previously coded variables was used, variables were age, gender, affiliation to health social security services -in Colombia this affiliation functions in two regimes: contributory and subsidized. Subjects with financial means such as workers, pensioners and their families, must adhere to the contributory system, subsidized regime is for citizens lacking payment capacity and who receive health services by means of a subsidy offered by the state-. In Colombia, dwellings are classified into six socioeconomic strata called: 1: low-low, 2: low, 3: medium-low, 4: medium, 5: medium-high, 6: high, school degree accomplished, use of tobacco or alcohol, systemic diseases (blood diseases, diabetes, rheumatoid arthritis, HIV/AIDS) and medication consumption. Information on periodontal condition was extracted based on the periodontal chart in this manner: plaque index (%), bleeding upon probing (%) number of locations with insertion loss clinical attachment loss (CAL) ≥ 4 mm, numbers of location with probing depth (PD) ≥ 4 mm, number of present and absent teeth excluding third molars. Periodontal chart includes information on CAL, PD and bleeding upon probing in six locations (mesial, central, and distal from vestibular and lingual aspect) of each tooth.
Periodontal diagnosis was determined using classification systems with comparative purposes (Table I). The first one is the one recorded in the clinical history at the moment of treatment, it corresponds to American Academy of Periodontics (AAP) which classifies chronic periodontitis as mild, moderate and severe as well as gingivitis.8,9 The second diagnosis was conducted according to the most recent classification of the Center for Disease Control and the American Academy of Periodontics CDC-AAP as mild, moderate and severe periodontitis and non-periodontitis.10 In this case, periodontal chart was analyzed and diagnosis was established by a previously standardized and gauged evaluator following classification criteria. Nevertheless, the standard reference point of periodontal diagnosis for data analysis was AAP classification, which is the most accepted at the present time.
Table I Periodontal diagnosis definition according to classification system.

CAL = clinical attachment loss; PD = probing depth.
Data analysis
Data cleansing was accomplished in order to review information inconsistencies. A descriptive analysis of all the study variables' frequencies was undertaken; periodontal disease frequency was calculated according to a classification system and concordance between both systems. In the case of qualitative variables, absolute and relative frequencies were presented, for quantitative variables, mean, median and standard deviation were calculated as well as interquartile range. χ2 was calculated to observe differences in percentile distributions in each of the clinical and sociodemographic variables, with respect to periodontitis severity. Median test was used for quantitative variables. Information was processed with statistical software SPSS version 21.0 (IBM).
RESULTS
Out of 3,864 clinical histories reviewed, 467 meet inclusion criteria. Sample analysis was composed of 112 (24%) males and 355 (76%) females. Age average was 53.3 ± 9.7 years, 13.5% of all patients informed of tobacco use and 24% consumed antihypertension drugs. From the socio-demographic perspective, almost half of them belonged to middle financial stratus; 51.6% was affiliated to social security contributory regime; 26.8% reported not having attended school and 34.3% only attended primary school.
Table II shows frequency of periodontal disease. Two classification systems were employed; they provided contrasting results: most patients were diagnosed with periodontitis, nevertheless, frequency was (92.1%) higher when CDC-AAP classification was used, in comparison to AAP classification (67.2%). According to severity degree, AAP classified most cases as severe periodontitis (43.2%) when compared to CDC-AAP classification, where most cases were of moderate periodontitis (48.4%). Prevalence difference is most noticeable in cases of non periodontitis/gingivitis (AAP 32.8% versus CDC-AAP 7.9%).
Table III shows concordance between two periodontal disease classification systems: in 155 cases there was agreement between both classifications when periodontitis was severe, showing greater concordance degree. Nevertheless, CDC-AAP classification produced more cases of moderate CP and with only 47 cases in concordance with AAP system. The greatest lack of concordance was observed in cases of gingivitis and non-periodontitis. These differences were statistically significant (p < 0.001).
Table III Periodontal diagnosis concordance between two classifications of periodontal disease.

Underlined black figures represent cases where there was concordance between both classification systems, p < 0.001.
Periodontal disease is described in table IV. Patients with periodontitis exhibited greater bleeding upon probing, loss of insertion (CAL ≥ 4 mm) and periodontal pockets (PD ≥ 4 mm); this difference was statistically significant (p < 0.001). Nevertheless, some patients with gingivitis exhibited sites with pre-existing insertion loss, but lacking ≥ 4 mm periodontal pockets. Patients had lost five teeth and in some cases close to 10 teeth. In general, patients with periodontitis lost more teeth than patients with gingivitis, nevertheless, this difference was not statistically significant. Tooth loss was greater in females with mild periodontitis (Table V).
Table IV Periodontal clinical variables.

AAP classification (1999) was used as reference standard for analysis.
IQR = interquartile range; CAL = clinical attachment loss; PD = probing depth; Mann Whitney U test = *p < 0.001; **p < 0.05.
Table V Analysis of present and absent teeth according to diagnosis.

AAP classification (1999) was used as standard reference for the analysis.
Me = median; IQR = interquartile range.
Table VI shows relationship between periodontal disease and sociodemographic variables. Periodontitis was more prevalent in males than in females (statistically significant, p = 0.025) and in middle and high socioeconomic strata (statistically significant p = 0.021), nevertheless, gingivitis was more frequently present in lower sociodemographic strata. Patients with periodontitis more frequently reported belonging to lower educational level, and consuming tobacco and alcohol. Systemic diseases such as diabetes, respiratory and blood conditions, arthritis and under pharmacological treatment were more frequent in patients with periodontitis.
Table VI Bivariate analysis between periodontal disease and sociodemographic variables.
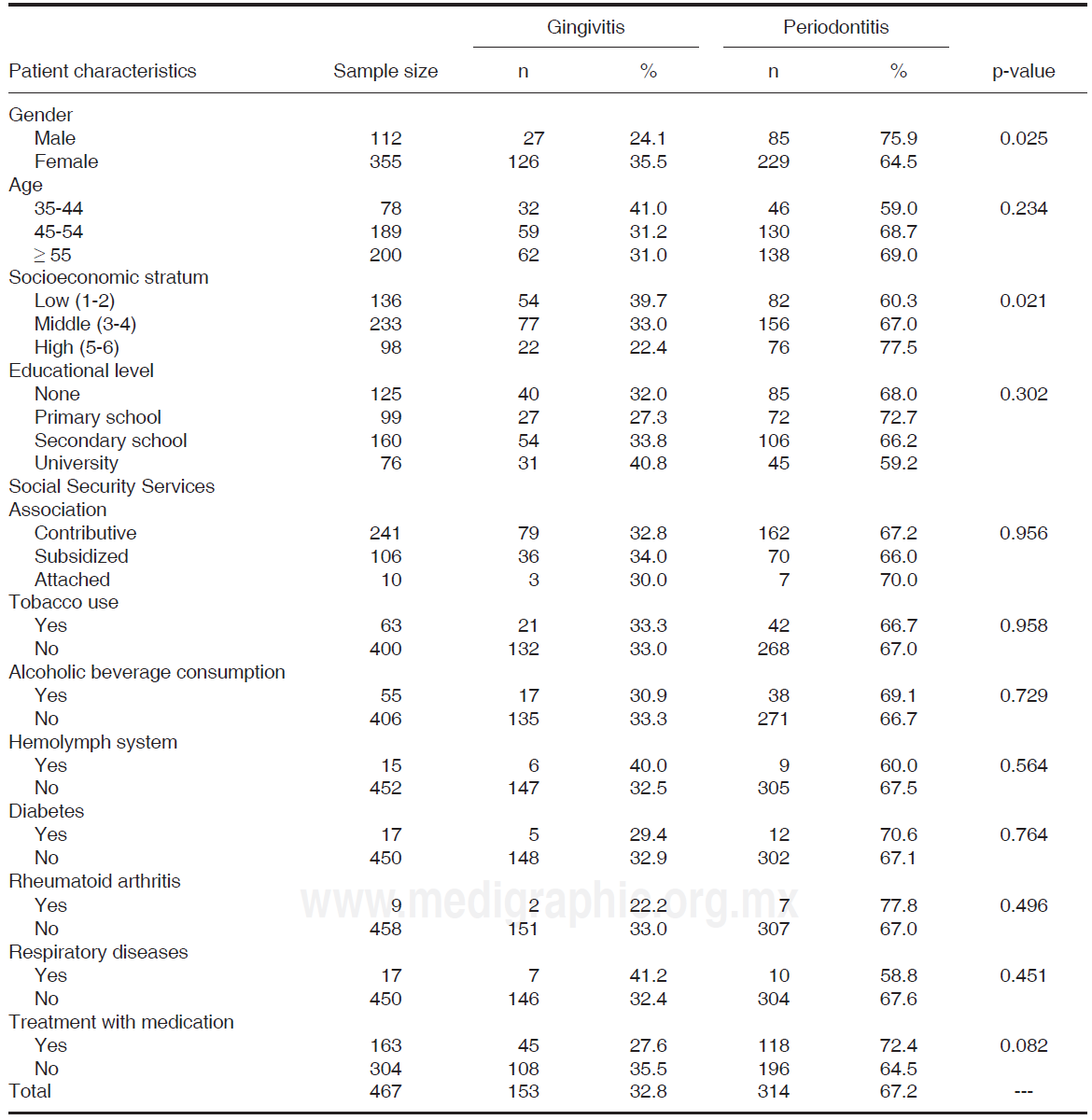
AAP classification was used as standard reference for the analysis. Lost values: education level (n = 7), affiliation to social security services (n = 110), tobacco use (n = 4) and alcoholic beverage consumption (n = 6).
DISCUSSION
The School of Dentistry of the University of Antioquia bases its functioning system in a model of teaching and service. This has been stipulated in Official Decree 2376 (2010). This facilitates development of human talent joining academic training with health services provision. This model allows comprehensive care of patients in aspects such as: diagnosis, design and execution of treatment plan under the supervision of trained teaching personnel. Main findings of this research provide information on periodontal circumstances of patients included in the study in relation to different clinical and sociodemographic variables which might prove to be decisive.
Periodontal disease frequency was established in this retrospective study. In the selected sample it was found that the majority of patients (67.2%) exhibited periodontitis in varied degrees of severity. Nevertheless, severe periodontitis was the most prevalent (43.3%). Data of other research projects conducted in varied countries were considerably different from that found in the present study. In Korea, periodontitis exhibits 29.4% prevalence in adult population.11 On the other hand, a study conducted in northern Jordan found that, in 66 examined 40-49 year old patients, 21.2% of them (that is to say 14 patients) exhibited chronic periodontitis, and that in 30 patients over 50 years, 53% presented this condition.12
In the present study, reported global frequency of periodontitis is comparable to values reported for this country (ENSAB IV [National Study of Oral Health], 2013-2014),4 where most individuals suffer moderate periodontitis (43.4%), and a smaller percentage (10.6%) is attributed to severe periodontitis. In the present study, severe periodontitis frequency was higher.
As shown beforehand, obtained data can vary among countries and studies, that is to say, from one study to the next. This could be due to the fact that many patients consult a dentist at the time their disease becomes more evident, or is at a more advance stage. On the other hand, differences in results might be due to periodontal disease classification system used in each case as well as clinical and sociodemographic variables included in the studies. Different patient inclusion and exclusion criteria for all studies must also be considered, as well as habits and cultural aspects germane to each population. Bearing this in mind, a comparison was established between diagnosis determined by an AAP classification8,9 and the more recent CDC-AAP classification.10 Difference in periodontitis prevalence was 25 percentile points, and it was greater (92%) when CDC-AAP classification was used. In cases of gingivitis and non-periodontitis, lesser concordance was found between both classifications. This is due to the fact that CDC-AAP criteria do not specify whether non periodontitis cases are periodontically healthy or gingivitis cases. Additionally, the CDC-AAP system does not provide universally accepted diagnostic criteria such as bleeding upon probing, and increased simultaneous depth upon probing (4 ≥ mm) and insertion loss (≥ 3 mm). In this respect, a national health study conducted in Chile revealed that 93-97% of all adults (35-74 years) in the study exhibited at least one site with insertion loss measuring > 3 mm.13 This is important since there can be interproximal sites with insertion level of ≥ 3 mm which do not present periodontal pockets of bleeding upon probing; therefore, it could be assumed that the case was being over-estimated. Furthermore, the cutting point is at least two sites with characteristics established by the system. This system does not mention extension (localized, generalized) and this affects case determination. In contrast, AAP classification does not only stratify insertion loss as mild, moderate or severe, it also recommends careful analysis of the case bearing in mind periodontal disease's clinical signs and symptoms.
Results were comparable to those of Costa et al (2009) study14 where periodontitis prevalence was determined using five different periodontitis definitions; they found that prevalence and extension results varied from 13.8 to 65.3% and from 9.7 to 55.6% respectively. In contrast, van del Velden's definition of periodontitis takes into account and determines that subjects must be classified according to when they present periodontal pockets measuring ≥ 4 mm with simultaneous insertion loss and bleeding upon probing at the same site.15 This last definition can be considered closer to reality when attempt is made to classify a subject as case or non- case in clinical practice, and for this reason it must be carefully taken into consideration when considering results. For this reasons, values reported in this periodontitis prevalence study as well as their analysis correspond to the AAP classification.
In the present study it was found that variables such as education level and type of affiliation to Health Social Security Services bear indirect influence on the onset of periodontal conditions and their later progress. This statement becomes evident when we observe greater indexes of periodontitis in patients lacking education, or with basic primary education (68 and 72.7% respectively). According to Jiang et al (2013),16 risks of suffering disease in the mouth increase when patients belong to lower levels of study or academic training, or lack health insurance affiliation; in these cases patients even suffer tooth loss. This fact is also reported by Ababneh et al (2012);12 he stated in his study that this relationship could be associated to difficulties to access health services and other help for the preservation of suitable oral health. Borrell et al (2006)17 stated that subjects with lower school educational levels were three times more susceptible to suffer periodontitis that those with a higher education level.
With respect to socioeconomic stratum, although presence of gingivitis was much higher at strata classified as lower, in concordance with other studies,12,16 presence of periodontitis was greater at middle and high strata. Possible explanations for this might reside in the fact that there are many neighborhoods and dwellings which are difficult to classify, and living in a particular stratum does not guarantee that subjects be in favorable social and financial circumstances. Another explanation is that these subjects are those looking for complex periodontal treatments which are not covered by benefit plans of the General System for Health of the Social Security. New studies should incorporate variables such as income level, type of occupation and employment circumstances.
A study conducted in Spain18 with 5,130 workers, showed that 38.4% exhibited periodontal pockets measuring 4.5 to 6 mm in depth, which significantly increased in patients > 45 years of age. Insertion loss (CAL) of 4-5 mm corresponds to 13.7% of the study group, meanwhile, 7.7% of studied population exhibited CAL of > 6 mm, with significant increase in severity in patients aged > 45 years. Periodontal disease of the sample studied in Spain became more unfavorable in patients with basic primary education and low income (this study was conducted under the codes of the Community Periodontal Index CPI. Meanwhile, Abahneh et al (2012) 12 confirm in their study that subjects with academic training of 12 years or more could exhibit gingivitis, but only 3.2% exhibited periodontitis; it was also observed that periodontal disease prevalence was higher in rural areas when compared to urban areas.
Tobacco use is one of the most determining risk factors in periodontitis, patients who smoked exhibited 66.7% periodontitis compared to 33.3% gingivitis. Studies conducted in the United States and other countries report a 6- to 7- fold increase of alveolar bone loss in patients who smoked, when compared to non-smoking patients. Moreover, dental insertion loss was three to five times greater in smokers than in non-smokers.19,20,21 In the case of Northern Jordan an 8.4% periodontitis prevalence was reported and was associated to patients observing active smoking habit, 17.6% for patients with history of smoking and 7.3% for non-smoking patients.12 In general, results reported in the present study are consistent with others that assess this risk factor.12,22
It is general knowledge that systemic diseases might represent a risk factor for periodontitis, or at the same time, the fact that systemic disease might be affected by periodontitis is a two-way relationship. For example, in the case of diabetes mellitus (DM) where ill-controlled diabetic patients exhibit greater degree of periodontitis severity, and in turn, this uncontrolled periodontitis bears influence in glycemia control in these diabetic patients.23,24,25
In the present study, this statement is confirmed since it was found that most diabetic patients of the studied sample exhibited periodontitis (70.6%), while only 29.4% suffered gingivitis. In the United States, periodontitis prevalence was 39% and was much lesser (< 3%)26 when compared to prevalence found in non-diabetic patients.
With respect to fortitudes and weaknesses of the present study, it is worth mentioning that a strict control was observed in inclusion and exclusion criteria, as well as inclusion of different clinical and sociodemographic variables, such as comparison between two classification systems, which enabled consistency in found results. Nevertheless, design of the present study did not allow establishment of causal relationships or calculation of epidemiological association measures, since healthy patients were not included. Likewise, since the present was a study encompassing secondary data, information depended upon quality of clinical histories (since missing data were found in them). New studies with longitudinal designs and use of primary data might allow to overcome these limitations.
In conclusion, presence of periodontitis in studied population was very high (60%) and was found to be related to systemic diseases, tobacco habit, affiliation to social security services and educational level. Periodontitis frequency is determined by the classification system employed.
REFERENCES
1. Botero JE, Rösing CK, Duque A, Jaramillo A, Contreras A. Periodontal disease in children and adolescents of Latin America. Periodontol 2000. 2015; 67(1): 34-57. [ Links ]
2. Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012; 91(10): 914-920. [ Links ]
3. Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe periodontitis in 1990-2010: a systematic review and meta-regression. J Dent Res.2014; 93(11): 1045-1053. [ Links ]
4. Colombia. Ministerio de Salud y Protección Social. IV Estudio Nacional de Salud Bucal. ENSAB IV: Para saber cómo estamos y saber qué hacemos. Bogotá: Ministerio de Salud y Protección Social 2013-2014; 2015: pp. 78-85. [ Links ]
5. Oppermann RV, Haas AN, Rösing CK, Susin C. Epidemiology of periodontal diseases in adults from Latin America. Periodontol 2000. 2015; 67(1): 13-33. [ Links ]
6. Heaton B, Dietrich T. Analytic epidemiology and periodontal diseases. Periodontol 2000. 2012; 58(1): 112-120. [ Links ]
7. Dye BA. Global periodontal disease epidemiology. Periodontol 2000. 2012; 58(1): 10-25. [ Links ]
8. Caton JG, Greenwell H, Mahanonda R, Williams R, Zappa U, Claffey N et al. Consensus report: dental plaque gingival diseases. Ann Periodontol. 1999; 4(1): 18-19. [ Links ]
9. Lindhe J, Ranney R, Lamster I, Charles A, Chung C, Flemmig T et al. Consensus report: chronic periodontitis. Ann Periodontol. 1999; 4(1): 38. [ Links ]
10. Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ. Update of the case definitions for population-based surveillance of periodontitis. J Periodontol. 2012; 83(12): 1449-1454. [ Links ]
11. Kim HS, Son JH, Yi HY, Hong HK, Suh HJ, Bae KH. Association between harmful alcohol use and periodontal status according to gender and smoking. BMC Oral Health.2014;14:73. [ Links ]
12. Ababneh KT, Abu Hwaij ZM, Khader YS. Prevalence and risk indicators of gingivitis and periodontitis in a multi-centre study in North Jordan: a cross sectional study. BMC Oral Health. 2012; 12: 1. [ Links ]
13. Gamonal J, Mendoza C, Espinoza I, Muñoz A, Urzúa I, Aranda W et al. Clinical attachment loss in Chilean adult population: first Chilean National Dental Examination Survey. J Periodontol. 2010; 81(10): 1403-1410. [ Links ]
14. Costa FO, Guimarães AN, Cota LO, Pataro AL, Segundo TK, Cortelli SC et al. Impact of different periodontitis case definitions on periodontal research. J Oral Sci. 2009; 51 (2): 199-206. [ Links ]
15. Baelum V, López R. Defining a periodontitis case: analysis of a never-treated adult population. J Clin Periodontol. 2012; 39(1): 10-19. [ Links ]
16. Jiang Y, Okoro CA, Oh J, Fuller DL. Sociodemographic and health-related risk factors associated with tooth loss among adults in Rhode Island. Prev Chronic Dis. 2013; 10: E45. [ Links ]
17. Borrell LN, Burt BA, Warren RC, Neighbors HW. The role of individual and neighborhood social factors on periodontitis: the third National Health and Nutrition Examination Survey. J Periodontol. 2006; 77(3): 444-453. [ Links ]
18. Carasol M, Llodra JC, Fernández-Meseguer A, Bravo M, García-Margallo MT, Calvo-Bonacho E et al. Periodontal conditions among employed adults in Spain. J Clin Periodontol.2016; 43(7): 548-556. [ Links ]
19. Westfelt E. Rationale of mechanical plaque control. J Clin Periodontol. 1996; 23(3): 263-267. [ Links ]
20. Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: Findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol. 2000; 71(5): 743-751. [ Links ]
21. Grossi SG, Zambon JJ, Ho AW, Koch G, Dunford RG, Machtei EE et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol. 1994; 65(3): 260-267. [ Links ]
22. Haffajee AD, Socransky SS. Relationship of cigarette smoking to attachment level profiles. J Clin Periodontol. 2001; 28(4): 283-295. [ Links ]
23. Palmer R, Soory M. Modifying factors. In: Lindhe J, Lang NP, Karring T, editors. Clinical periodontology and implant dentistry. Oxford: Blackwell; 2008. pp. 307-327. [ Links ]
24. Papapanou PN. Periodontal diseases: epidemiology. Ann Periodontol. 1996; 1(1): 1-36. [ Links ]
25. Mealey BL, Moritz AJ. Hormonal influences: effects of diabetes mellitus and endogenous female sex steroid hormones on the periodontium. Periodontol2000. 2003; 32: 59-81. [ Links ]
26. Mealey B, Oates T. Diabetes mellitus and periodontal diseases. AAP-commissioned review. J Periodontol. 2006; 77(8): 12921303. [ Links ]
** This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
Received: May 2016; Accepted: January 2017











 text in
text in 



