Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.16 n.4 Ciudad de México Oct./Dec. 2012
Case report
Camouflage orthodontic treatment of skeletal class II malocclusion with dental-facial asymmetries and missing teeth. Clinical case report
Hugo Alberto Vásquez Estrada,* Rolando González López§
* Graduate, Orthodontics Specialty, Research and Graduate School, National School of Dentistry, National University of Mexico (UNAM).
§ Professor, Orthodontics Specialty, Research and Graduate School, National School of Dentistry, National University of Mexico (UNAM).
ABSTRACT
Camouflage orthodontics is a treatment alternative based upon rendering moderate or light dental-skeletal anomalies less evident through instauration of merely dental-alveolar movements. Mandibular asymmetries are a special group of maxillary anomalies which develop at embryonic stage as well as after birth. They can be due to hyper- or hypo- growth of a hemi-mandible, or by a combination of both. Retained canines are a relatively common dental eruption anomaly in general population. This represents, among other collateral problems, a root integrity risk for adjacent teeth. Therefore, a decision must be made to perform traction to move them towards the dental arch, or, alternatively, it can be decided to surgically extract them so as to avoid complications during treatment. Missing teeth can represent a challenge for the orthodontist, when designing treatment plan. He must decide whether to preserve space for a future prosthesis or to close spaces through orthodontic movement of adjacent teeth, which will in turn functionally substitute missing teeth. This article presents camouflage orthodontic treatment performed on a 29 year old female patient. Diagnosis emitted for this patient was as follows: skeletal Class II malocclusion, moderate dental-facial asymmetry, retained upper right canine and left lower third molar, as well as absence of left lower first molar. To this effect a Pro-torque slot .0128 x .025 straight wire appliance was used. Three first premolars and retained canine were extracted and left lower second and third molars were subjected to mesialization.
Key words: Camouflage orthodontics, skeletal class II malocclusion, dental-facial asymmetry, retained canine, retained third molar.
INTRODUCTION
Shape and position of jaws are genetically predetermined; together with softer sections surrounding them they greatly influence facial aesthetics as well as stomatognathic system function. Alterations of shape or size of maxillary bone bases entail alterations of facial harmony, therefore, uniform development is the base for adequate facial aesthetics and function.1
In most cases, facial asymmetry can only be detected when comparing homologue sections of the face. Facial asymmetry becomes the patient' s main concern when this is observed in the mirror or in photographs. According to Proffit, most individuals present a slightly larger right side when compared to the left one.2-4
After adolescent maximum growth peak, severe asymmetries can take place, more frequently due to growth excess rather than to growth deficiency. They can occur either before or during this development phase, but do not become apparent until the point when maximum growth has come to conclusion. In cases when hyper-activity takes place before adolescence, growth can derive into severe deformities.5
A study conducted between 1976 and 1996, at the Dental-Facial Clinic, North Carolina University with a sample composed of 1,460 patients, showed that 495 patients (34%) presented apparent asymmetry, and 75% presented lower third facial deviation.4
Mandibular asymmetries are a special group of jaw anomalies. They develop at embryonic phase, as well as during post-natal stages, during general growth periods, or, occasionally, after growth period is completed. They can be due to hypo-growth of one side of the jaw (hemi-mandible), the hyper-growth of the other side, or a combination of both; emitting diagnosis of these cases is therefore a very complex procedure. Affected areas can be the condyle, the neck, body, as well as mandibular ramus. The patient regularly attends orthodontic service due to clear facial asymmetries with mandibular deviation, malocclusion, and, in some cases TMJ symptoms. These defects are normally detected during the patient's second and third decades of life. This abnormal condition must be differentiated from other processes which cause facial asymmetries such as hemi-facial microsomia, hemi-facial atrophy, ankylosis and bone tumors.6,7
Occasionally, excessive unilateral growth of the lower jaw occurs in individuals who appear to be metabolically normal. The exact reason for this anomaly is, as yet, not quite clear. It is more common in women with ages ranking from 15 to 20 years, but nevertheless it can occur, in both genders, at earlier ages like 10 years, or at a later stages like 30 years of age. This condition was formerly called condylar hyperplasia. Nevertheless, since the body of the mandible is also affected, currently the most appropriate terms used to describe these conditions are hemi-mandibular elongation (HE) or hemi-mandibular hypertrophy (HH).8,9
Dental-facial asymmetry diagnosis basically depends on patient history and physical examination, as well as assessment of malocclusion and TMJ symptoms.10 Paraclinical examinations are very helpful. The most frequent are radiographic examinations such as orthopantomography, lateral skull x-rays as well as anterior-posterior x-rays (AP). It is currently possible to gain help through a tri-dimensional observation of the patient's characteristics. This can be achieved through computerized axial tomography. Model analysis, as well as the study of intra or extra-oral clinical pictures will provide a broader panorama of the dental-facial asymmetry diagnosis.3,6,7,11,12
Once the dental-facial problem is determined, an important decision must be made about the best treatment plan. This is due to the fact that an evident skeletal asymmetry is involved and therefore, orthodontic treatment, by itself, will not fully remove the basic problem. There are two treatment possibilities which must be clearly explained to the patient before undertaking procedures: 1) orthodontic-surgical correction of the problem, with mandibular ramus osteotomy, to correct facial asymmetry,1-3 or, 2) asymmetry compensation with the help of camouflage orthodontic treatment which will correct malocclusion and also acceptably dissimulate bone defects. This second procedure might improve facial aesthetics, or, to the very least, it will not aggravate the problem.13 Some of the factors that influence patients into preferring camouflage orthodontic treatment over surgery are long term stability as well as cost-benefit and risk-benefit ratios4,5
The objective of this article was to present progress and final results of a camouflage orthodontic treatment performed on a patient with the following characteristics: skeletal class II malocclusion with moderate dental-facial asymmetry, upper right canine retention, lower left third molar retention as well as absence of lower left first molar.
METHOD (CASE PRESENTATION)
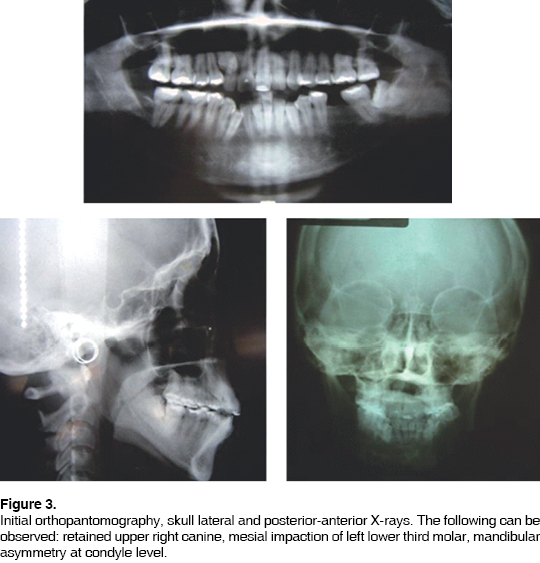
A 29 year old female patient sought attention at the Orthodontics Clinic, National School of Dentistry, National University of Mexico. The patient reported ''concern about her retained canine''. History was taken, as well as study models and extra-oral X-rays (orthopantomography, skull lateral, anterior-posterior). As medical history, she informed of pelvis fracture with surgical intervention as well as prescribed extraction of lower left first molar due to dental caries. Clinical diagnosis revealed dolychocephaly, oval face, convex profile, facial midline not matching upper dental midline, labial incompetence, 6mm gingival smile, moderate dental-facial asymmetry with left mandibular deviation (Figures 1 and 2). Cephalometric diagnosis revealed skeletal Class II due to moderate retrognathia, dolychocephalic biotype, excessive vertical growth and dental bi-protrusion. Radiographic examination revealed mandibular asymmetry due to elongation of right hemi-mandible, especially at condyle and condylar neck level. Retentions of upper right canine and left lower molar were present. Root parallelism was inexistent and many teeth presented short roots (Figure 3). The patient presented the following dental relationships: Right molar class III, left molar class not classified, right canine class not classified, left canine class II, slight anterior open bite, cross-bite at left premolar level, cusp-to cusp bite on second left molars, moderate upper and lower crowding, mismatched dental midlines, lower right canine with ectopic eruption, excessive wear of occlusal surfaces in posterior teeth. Model analysis revealed sagittal and transverse maxillary-mandibular collapse. These findings were supported by posterior-anterior X-rays, which reveled decreased inter-molar maxillary and mandibular widths, a 3.6mm mandibular midline deviation to the left with respect to maxillary midline, as well as edged occlusal plane.
The patient was offered two treatment options: 1) surgical-orthodontic treatment to correct asymmetry and malocclusion, 2) camouflage orthodontic treatment to eliminate malocclusion and attempting to dissimulate asymmetry. The patient decided upon the second option. First premolars were extracted, exception made of the upper right first premolar. Upper right canine was surgically extracted. Left lower third molar was subjected to a process of mesialization and distalization along with the second molar on the same side of the arch, to fill the space left by the extracted first molar. Pro-torque slot .018'' x .025'' orthodontic appliance was put into place. Treatment was then initiated in the following fashion.
Anchorage. Active trans-palatine bar (ATB) with extension towards premolars for expansion and lingual arch. After three months of treatment, lingual arch and ATB extensions were removed. ATB was removed after 17 months of treatment.
Alignment leveling and rotation correction phase. The following arches were used: .014'' CuNiTi and .016'' NiTi. This phase lasted for five months during which distal movement of canines was achieved with the use of closed elastomeric chain.
Space closure and midline correction phase. Use of contraction arches .016'' x .022 Blue Elgiloy, with use of inter-maxillary elastics; class II in the left, class III in the right, as well as crossed anterior. With the use of an elastomeric chain, the left lower second molar was moved towards mesial direction.
Both dental arches were once more leveled with wire arches .018NiTi and .018SS. A button device was placed on the third retained molar, placing an inter-maxillary elastic to go from this position to the left upper second molar in order to parallelize it and also extrude it. Use of elastics was continued for midline correction. Once the clinical crown of the third molar presented acceptable surface, a tube was placed on the vestibular side, as well as a button on the lingual size to level it and de-rotate it, with the help of an elastomeric chain.
Detailing and completion phase. .016'' x .022NiTi, .016'' x .022SS, .017'' x .025''NiTi, .017'' x .025 SS. Before removing devices, a new orthopantomography was taken to confirm root parallelism. The patient was then remitted to the periodontics department, to be subjected to gingivectomies to elongate clinical crowns and circumferential supra-crest fiberotomy at the level of the left lower third molar, so as to avoid relapse possibility after removal of the orthodontic device. Orthodontic devices were removed after 35 months of treatment.
Retention. Circumferential plates were placed. 24 hours a day use was recommended for 6 months, to eventually only be used during the night. Monthly reviews were conducted during the 3 months that followed treatment completion. The patient was advised to attend bi-yearly visits to control retention.
RESULTS
At treatment completion, the patient presented skeletal class II with a slight decrease of the initial maxillary-mandibular discrepancy. Due to existing mandibular deviation, class I left canine and class III right canine relationships were present, even though the upper right first premolar substituted the canine in that side of the arch. Right molar class III was preserved; on the left side molar class I was achieved. The lower first molar was substituted through a process of mesialization of second and third molars in that arch. The midline was partially improved, but was not fully corrected. Proper horizontal and vertical overbites were achieved. Table I shows initial and final cephalometric data where significant changes can be observed. The patient's main complaint was solved with surgical extraction of the retained canine, and its substitution by the right upper first premolar. From the clinical standpoint, the esthetic result was deemed favorable since labial incompetence was eliminated, profile convexity was reduced, gingival smile was eliminated and facial asymmetry was considerably dissimulated (Figures 4 and 5). Radiographically, incisor dental-alveolar inclination changes could be seen as well as proper root parallelism in all teeth at treatment completion (Figure 6).
DISCUSSION
It is important to perform a detailed assessment of clinical cases where skeletal defects which might cause dental and facial asymmetries can be detected, since a decision must be made to either orthodontically correct the problem or propose orthognathic surgery to the patient. According to Mihalik and Profitt (2003)14 the most important factor when deciding between orthodontic camouflage or surgery is to establish whether the aesthetic improvement achieved with surgery is ,for the patient, worth the increase in cost and risks. Surgery risks are obviously much greater than risks incurred upon with camouflage orthodontics. The most common surgery risk is decrease or loss of lip sensitivity. In camouflage orthodontics to redress skeletal class II, the risks appear to be upper incisor root resorption, since they become retracted and tilt against the cortical palatal plate.13 The present clinical case did not present severe dental and facial asymmetry. Therefore it was possible to suggest to the patient she should consider the use of camouflage orthodontics to decrease her functional and aesthetic problem, since not all cases can be dentally compensated or corrected. In the present case, the psychological make-up of the patient was of paramount importance: her skeletal defect did not represent for her a problem impinging on her quality of life, therefore, choosing treatment plan was simpler.
In the present case, when performing asymmetric extraction of left first upper premolar and first lower premolars, a maxillary-mandibular retraction was achieved. This reflected as a 3o and 2o decrease in SNA and SNB angles respectively. According to ANB, a 1o maxillary-mandibular discrepancy decrease was achieved. Significant changes in dental pro-inclination were also observed, as well as in labial protrusion with respect to Ricketts Esthetic line (E plane). According to Mihalik and Profitt (2003), patients treated with camouflage orthodontics did not reflect significant skeletal changes, they experienced changes no greater than 2 mm at the points a, B, or pogonion.14 Luecke and Johnson (1992) found average retraction of -2.2 mm in the upper lip, and -1.4 mm in the lower lip with respect to plane E in cases of upper premolar extractions.15
Another important aspect of this clinical case was the decision which had to be made with respect to the retained upper right canine. According to Dachi and Howell (1961) and Tylander and Myrberg (1973) incidence of canines retained in the upper jaw in general population ranges between 1 to 3%.16,17 A study conducted in 1984 showed that untreated partially erupted or impacted canines can give rise to several complications such as displacement and vitality loss of adjacent incisors, decrease in dental arch length, follicular cysts formation, canine ankylosis, recurrent pain and infections, external and internal resorption of canines and adjacent teeth, or any combinations of all the aforementioned factors.18
It was then decided to perform surgical extraction of the retained upper right canine, since it was considered that if trying to move it to the first premolar position there was risk of harming the root of the lateral incisor.
According to De-la-Rosa & et al (2006). most lower third molars can be parallelized and acceptably substitute lower second molars in cases when the latter are absent or have been extracted.19
Ay & et al (2006) studied position changes of lower third molars after unilateral extraction of lower first molars in non-orthodontic patients. They concluded that this type of extraction increases space for third molar eruption and helps to situate them in a better position.20
Bayram & et al (2006) concluded that first molar prescribed extraction for orthodontic reasons, can significantly increase eruption space of third molars in cases when second molars are moved to mesial position.21
In the present case, the patient presented absence of left lower first molar, which had been previously extracted due to dental caries. The lower third molar on that same arch was present, but it was retained as well as mesially tilted. In order to avoid yet another extraction and absent first molar substitution with a prosthetic device, it was then decided to move the left lower second molar to a mesial direction as well as orthodontically parallelizing and mesializing the retained third molar, thus achieving adequate position within the arch as well as successfully substituting the lower second molar.
CONCLUSIONS
Camouflage orthodontics has inherent limitations, since we are trying to solve skeletal problems through the use merely of dental movements. In cases of dental-facial asymmetries, some of the dental objectives to be met, such as matching midlines as well as molar and canine class I will not be ideally achieved.
Function of each and every tooth is very specific. Sometimes, eruption problems or dental absences due to development, or to caries and dental extractions, make it impossible for a tooth to occupy a specific place in the dental arch. In these cases, substitution of this tooth must be considered, either with orthodontic movements which will move another tooth to the position of the absent one, or preserving the space for later rehabilitation with a prosthetic device.
REFERENCES
1. Borja A, García-Rozado A. Diagnóstico y tratamiento de las asimetrías mandibulares. Protocolos Clínicos de la Sociedad Española de Cirugía Oral y Maxilofacial 29: 407. [ Links ]
2. Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: A review. Angle Orthod 1994; 64: 89-97. [ Links ]
3. Legan H. Surgical correction of patients with asymmetries. Seminars in Orthodontics 1998; 4 (3): 189. [ Links ]
4. Servert TP, Proffit WR. The prevalence of facial asymmetry in the dentofacial deformities population at The University of North Carolina. Int J Adult Orthod Orthog Surg 1997; 12: 171-176. [ Links ]
5. Proffit WR, Raymond P. Contemporary treatment of dentofacial deformity. St. Louis; Mosby, 2003. [ Links ]
6. Obwegeser H. Mandibular growth anomalies Springer-Verlag. Berlin, 2000. [ Links ]
7. Campos A, Cardona C, Merlano S, Montoya P. Hiperplasia condilar: revisión de la literatura. Revista Odontológica Maxilofacial 2002; 6: 46-53. [ Links ]
8. Obwegeser HL, Makek MS. Hemimandibular hypertrophy, hemimandibular elongation. J Maxillofacial Surg 1986; 14: 183-208. [ Links ]
9. Proffit W. Contemporary orthodontics. ed 4, St. Louis; Mosby 2007. [ Links ]
10. Legan H. Surgical correction of patients with asymmetries. Semin Orthod 1998; 4: 189-219. [ Links ]
11. Kronmiller J. Development of asymmetries. Semin Orthod 1998; 4: 134-137. [ Links ]
12. Urban S, Waite P. Management of facial asymmetry. Am J Cosm Surg 2005; 22 (4): 214-221. [ Links ]
13. Proffit WR, Phillips C, Douvartzidis N. A comparison of outcomes of orthodontic and surgical-orthodontic treatment of Class II malocclusion in adults. Am J Orthod Dentofacial Orthop 1992; 101 (6): 556-565. [ Links ]
14. Mihalik CA, Proffit WR, Phillips C. Long-term follow-up of Class II adults treated with orthodontic camouflage: A comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop 2003; 123 (3): 266-278. [ Links ]
15. Luecke PE, Johnston LE. The effect of maxillary first premolar extraction and incisor retraction on mandibular position: testing the central dogma of ''functional orthodontics''. Am J Orthod Dentofacial Orthop 1992; 101: 4-12. [ Links ]
16. Dachi SF, Howell FV. A survey of 3,874 routine full mouth radiographs. Oral Surg Oral Med and Oral Pathol 1961; 14: 1165-1169. [ Links ]
17. Thilander B, Myrberg N. The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res 1973; 81: 12-21. [ Links ]
18. Shafer WG, Hine MK, Levy BM. A textbook of oral pathologyed 4. W.B. Sauders; Philadelphia, 1998. [ Links ]
19. De-la-Rosa-Gay C, Valmaseda-Castellón E, Gay-Escodac C. Spontaneous third-molar eruption after second-molar extraction in orthodontic patients. Am J Orthod Dentofacial Orthop 2006; 129: 337-344 [ Links ]
20. Ay S, Agar U, Biçakçi AA, Kösger HH. Changes in mandibular third molar angle and position after unilateral mandibular first molar extraction. Am J Orthod Dentofacial Orthop 2006; 129: 36-41. [ Links ]
21. Bayram M, Özer M, Arici S. effects of first molar extraction on third molar angulation and eruption space. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: e14-e20. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
Hugo Alberto Vásquez Estrada
E-mail: hugodonto9@hotmail.com











 text in
text in 


