Services on Demand
Journal
Article
Indicators
Related links
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.16 n.3 Ciudad de México Jul./Sep. 2012
Case report
Stab wound in maxillofacial region. A case report
Ana María Nieto Munguía,* Gloria Leticia Lara Fong,§ Luis Rodrigo Flores Flores§
* Attached to Maxillofacial Surgery Service, Regional Hospital Adolfo López Mateos, ISSSTE.
§ Maxillofacial Surgeon, private practice.
ABSTRACT
Stab wounds in maxillofacial region are infrequent and rarely reported. These lesions can be life-threatening, especially in cases where major blood vessels are involved and resulting hemorrhage obstruct airways. Treatment must be of a multi-disciplinary nature: it begins at the trauma unit to provide airway maintenance, hemodynamic stabilization, and if necessary, neurological ophthalmological and vascular evaluation.1,2 This study presents the case of a lesion caused by a stabbing weapon. The lesion penetrated into the left orbit causing fracture of the orbit floor, proceeding to the soft palate, and did not damage important structures. The knife was removed through the entrance wound. Fracture was reduced with resorbable plates. No complications were observed either during or after surgery.
Key words: Knife injurie, resorbable plates, orbital fracture.
INTRODUCTION
Lesions which penetrate or surround the orbit represent potentially life-threatening trauma. In a study conducted during World War II,3 a 12% mortality rate was found in 42 patients suffering maxillary-orbital wounds with intra-cranial extension.
Lesions of the orbits and face can be obvious. Nevertheless, diagnosis can become difficult due to the intense inflammation experienced by facial structures surrounding the orbits and patient's lack of cooperation when faced with trauma.
CLINICAL CASE
16 year old male patient attended the Pediatric Emergency Service of the Regional Hospital ''Lic. Adolfo Lopez Mateos'' ISSSTE, Mexico City, due to a stab wound located in the left infra-orbital region caused by third party aggression. The patient was conscious, not presenting data of neurological deterioration or active hemorrhage. Airways were not compromised. He presented severe edema and ecchymosis in the orbital region which hindered occlusion of left eye. Intra-ocular exploration revealed upward displacement of ocular globe, due to one end of the weapon, and which limited eye movements. Patient reported blurry vision. The infra-orbital wound had been sutured outside of the Institution with 3-0 nylon material (Figures 1 and 2).


When performing intra-oral exploration ecchymosis of the right soft palate was observed. At that site, upon palpation, the tip of the knife could be felt. There was no open communication into the oral cavity. When history was taken, the patient revealed history of drug addiction, as well as drug intake just before the aggression.
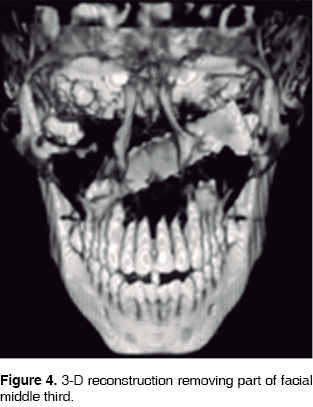
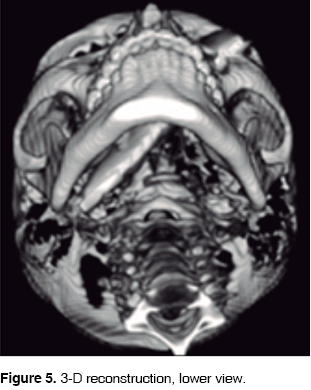
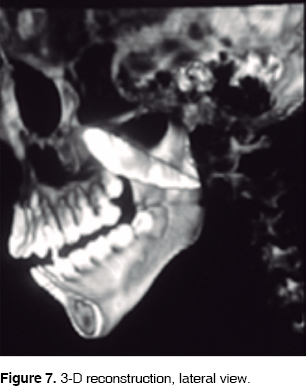
Imaging studies were conducted (Figures 3 to 7) (4, 5, 6) at different projections, to determine the extent of the wound and its probable relation to important neighboring structures. Computed tomography showed the knife's trajectory, which affected the orbit floor and left maxillary sinus, and crossed over laterally until reaching the right side of the palate.


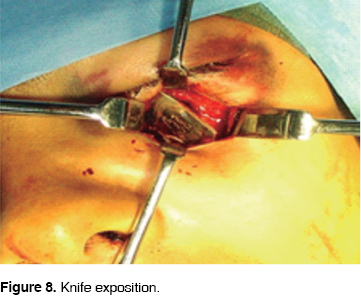
The patient entered the operating theatre and was subject to general anesthesia. The knife was withdrawn pulling it through the wound, without causing any damage to neighboring structures. (Figures 8 to 10)(9).


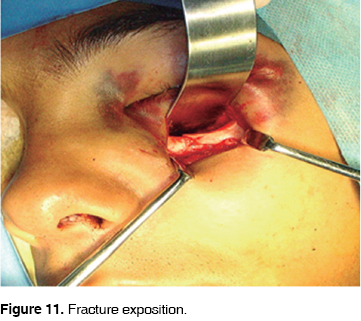
After this, reduction and fixation of the orbital floor fracture was achieved by placing resorbable plate and screws. The wound was sutured anew, and the surgical event was finalized with the administration of the following drugs: clyndamycin 600 mg IV every 6 hours, ketocorolac 10 mg every 8 hours for two days, metoclopramide, 10 mg IV, single dose, dexamethasone 8 mg IV, single dose. The patient was discharged and asked to continue with clyndamycin 600 mg every 6 hours for 7 days, as well as ketocorolac 10 mg every 8 hours for two days. The patient experienced satisfactory evolution immediately after surgery: visual acuity was restored, eye movements were not compromised, excellent functional esthetic and results were obtained. These results were obvious in post-surgery control visits (Figures 11 to 14)(12, 13).



DISCUSSION
Treatment of penetrating lesions located in the maxillofacial region can vary according to the lesion's etiology, the nature of the retained foreign body, the site of the lesion, as well as extension of damage to soft and hard tissues of the region and neighboring structures.4 Eyes are especially vulnerable to intrusive lesions and foreign bodies, which can lodge within the orbit and even extend beyond it, into the skull. Removal of foreign bodies is not always easy, especially in cases when they deeply embed themselves into soft tissues.
Routine removal of a foreign body is normally performed through the entrance wound as well as the trajectory created by the foreign object. It might prove necessary to expand the incision caused by the wounding agent so as to facilitate proper exploration of the trajectory, and the recovery of the foreign body with a curved hemostat. Removal of an intruding object, such as a knife, serrated fragments of a bullet, or shards of glass, must be approached with extreme caution, since these very sharp objects could damage vital structures during the removal process.
CONCLUSIONS
Penetrating lesions on the middle facial third, where intracranial extension is suspected, must be assessed and treated following multi-disciplinary criteria. Therefore, the following is recommended:
1. Airway should be examined, and in some cases, endotracheal intubation might be needed to ensure patient's proper ventilation.5,6
2. Vascular damage is frequently diagnosed and treated at early stages.5,7
3. X-rays and tomography are paramount to determine the wound's trajectory and assess any possible damages to central nervous system.
4. These lesions can severely affect anatomical structures such as maxillary sinus, ocular globe, blood vessels, brain and cervical spine.5,8,9
5. Detailed history of trauma incident must be obtained, including description of the weapon.
Ophthalmological, neurosurgical, and ENT services must always be consulted, so they can assist in orbital framework fracture management, or in cases when foreign bodies are embedded into the orbit, or into circum-nasal and intra-cranial sinuses in cases associated with penetrating maxillofacial trauma.
Injuring artifacts such as shot, or bullet fragments superficially located must be removed through the entrance way. Nevertheless, artifacts located in deeper planes and impinging upon vital structures must be subject of a more detailed and prolonged examination as well as systematic follow-ups.
Facial lesions in the mid-facial third with intra-cranial extensions, must be borne in mind when assessing moderate or severe intruding trauma. The possibility that this trauma might show extension towards the brain must also be considered.
When treating maxillofacial or circum-orbital penetrating trauma, signs and symptoms associated to intra-cranial extension can be attributed to other causes in cases when there is no fracture of the orbital floor or cranial fossa floor is suspected.3
REFERENCES
1. Shinohara EH, Heringer L, de Carvalho PJ Jr. Impacted knife injuries in the maxillofacial region Report of 2 cases. J Oral Maxillofac Surg 2001; 59: 1221-1223. [ Links ]
2. Morrissette MP, Chewning LC. Rapid airway compromise followingtraumatic laceration of the facial artery. J Oral Maxillofac Surg 1990; 48: 989. [ Links ]
3. Díaz FJM, Caballero JJ, Quintero MY, Peña SL. Lesiones penetrantes maxilofaciales. Presentación de 4 casos. Rev Cubana Estomatol 2006; 43 (3). [ Links ]
4. Gan BJ, Kallal RH, Helgerson AC. The imagen interfier in oral and maxillofacial injuries surg. J Oral Maxillofac Surg 2000; 28 (3): 726-31. [ Links ]
5. Bourguignon FAM, Puppin AAC, Pimentel DP, Jaques PM. Unusual penetrating orbit injury. Int J Oral Maxillofac Surg 2006; 35: 92-93. [ Links ]
6. Motamedi MH. Primary management of maxillofacial hard and soft tissue gunshot and shrapnel injuries. J Oral Maxillofacial Surg 2003; 61: 1390-1398. [ Links ]
7. Shinohara EH, Heringer L, Carvalho JP Jr. Impacted knife injuries in the maxillofacial region: report of 2 cases. J Oral Maxillof Surg 2001; 59: 1221-1223. [ Links ]
8. Azevedo R, Carneiro B Jr, González A. Traumatismo facial por agresso com arma branca- relato de um caso clìnico. Rev Odonto Ciencia 2003; 18: 13-16. [ Links ]
9. Exadaktulos AK, Stettbacher A, Bautz PC. The value of protocol-driven CT scanning in stab wounds to the head. Am J Emerg Med 2002; 20: 295-297. [ Links ]
 Mailing address
Mailing address
Dra. Gloria Leticia Lara Fong
E-mail: dra_gloriallf@hotmail.com
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 text in
text in 


