Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.16 n.1 Ciudad de México Jan./Mar. 2012
Case reports
Mandibular desmoid tumor. Case report
Doroteo Vargas López,* Ronald Rojas Villegas,§ Víctor García Alcaraz,* Sara Guadalupe García AmadorII
* Physician attached to the Maxillofacial Surgery Service of the ''Adolfo López Mateos'' Hospital ISSSTE. Mexico City, Mexico.
§ Maxillofacial Surgeon, private practice.
II Former resident attached to the Maxillofacial Surgery Service of the Regional Hospital ''Adolfo López Mateos'' ISSSTE. Mexico City, Mexico.
ABSTRACT
Desmoid tumor is a fibroblastic proliferation of aponeurotic muscle tissue, fascia or periosteum of unknown etiology. It generally appears as a single tumor and can be related to Gardner's Syndrome. It is considered a rare lesion, representing less than 0.03% of all tumors, with a annual incidence of 2-4 cases per 100,000 habitants. It usually appears as a mass (body) with symptomatology associated to location. It has the potential of achieving local invasion without progressing to metastasis. These tumors experience high rates of local recurrence after surgery, even when wide margins have been respected. A case of a 12 year old male patient is presented. He attended the Maxillofacial Surgery Service of the Hospital Regional Adolfo Lopez Mateos due to a volume increase of the left ascending mandibular ramus.
Key words: Desmoid tumor, extraabdominal, mandible.
INTRODUCTION
There is an ill-defined group of fibroblastic cells hyperplasia called fibromatosis. These can vary from a postinflammatory keloid scar up to non neoplastic fibrosis. Also included are lesions which can be considered as mid-way between fibromas and fibrosarcomas and are known as aggressive fibromatosis (desmoid tumors). 1
Desmoid tumor is a fibroblastic proliferation of musculoaponeurotic tissue, fascia or periosteum. It consists of a painless, non encapsulated, ill- defined single tumor mass. It shows a firm consistency upon palpation, presents a grayish hue, is of slow and progressive growth, benign, locally invasive, and with a tendency to recurrence. It equally presents the ability to encapsulate adjacent neurovascular structures.2 It can present an unpredictable evolution, and when the lesion is located in the head or neck its proximity to vital and complex structures can complicate its evolution or treatment.
It generally appears as a single tumor and can be related to Gardner's Syndrome.2,3
Its etiology is not well known. Some studies suggest the possibility of some genetic defect. Other correlations indicate the possible role of trauma6 and estrogen stimulation as causes of these lesions.1,4-6
INCIDENCE AND PREVALENCE
It is a rare lesion representing less than 0.03% of all tumors, with yearly incidence of 2-4 cases per 100,000 people. They represent 0.03% of benign tumors and 0.06% of all bone tumors.
Desmoid tumors associated with hereditary adenomatous polyposis are 1,000 times more frequent than those found in general population. There is a female: male predominance of 2:1. Prevalence of desmoid tumor in this condition is 7-12%. In these patients, abdominal location of the tumor is most frequent. 42% of these tumors are located within the abdomen and the remaining 40% are found in the abdominal wall.7
CLINICAL OBSERVATIONS
These tumors appear as a mass whose symptomatology will depend on its location. Usually they present a slow growth pattern, and can reach considerable size. In 10% of cases, a rapid growth pattern can be found, spontaneous regression cases have also been described.8
DIAGNOSIS
Diagnosis is established based on findings obtained from clinical observation, as well as radiographic and histopathological studies.9
CLINICAL CASE
12 year old male patient attended the Maxillofacial Surgery Service of the Regional Hospital ''Lic. Adolfo López Mateos'' due to a one month evolution mass increase in the left mandibular ascending ramus. The lesion presented the following characteristics: limits the oral opening, is painful, indurated, of approximately 3 mm in diameter, non displaceable, non erythematosous, non hyperhemic or hyperthermic (Figure 1).

In orthopantomography evaluation, a radiolucid zone is observed in the left ramus and mandibular body, observing a third molar in proximity of the lesion region (Figure 2). A 3D reconstruction achieved through computerized tomography was requested. In it, a hypodense zone in the left mandibular ascending ramus zone was observed, as well as bone lysis and a tumor mass of approximately 6 to 8 cm diameter extending into the infratemporal fossa (Figures 3, 4 and 5).




An angiography was performed to preclude vascular compromise (Figure 6)

Under localized anaesthesia, incisional biopsy was performed and the sample was sent to the pathology department.
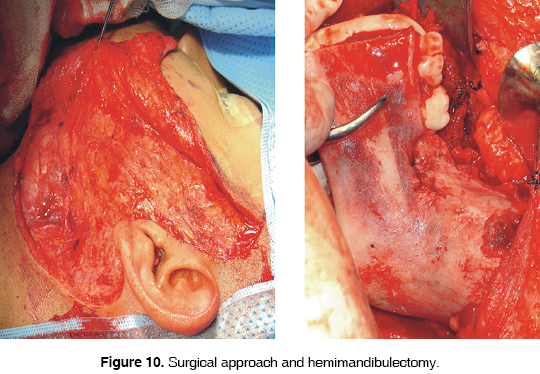
Anatomical and pathological study revealed a desmoid tumor located on the outside of the abdomen (Figure 7). Surgery was performed in the following fashion: temporal, preauricular retromandibular approach with submandibular extension to uncover left ramus and mandibular body; Tumor mass was removed from soft tissues, a hemimandibulectomy was performed with the placement of a mandibular reconstruction plate (Figures 8, 9, 10, 11, 12 y 13).






Based on the anatomical and pathological study the diagnosis of desmoid tumor was confirmed. The patient presently shows favorable evolution, facial paralysis in remission, no recurrence data, and is under strict surveillance (Figure 14).

DISCUSSION
Enzinger and Weiss10 differentiate between superficial and deep desmoid tumors. Included within the superficial tumor category are the following: palmar (palm), plantar (sole) and genital tumors.
Deep fibroid tumors include the following subtypes: abdominal, intraabdominal and extraabdominal (inside and outside of the abdomen). According to this classification, desmoid tumors of the head and neck belong to the deep fibroid group and extraabdominal type.
WHO describes it as a benign tumor, characterized by the presence of abundant collagen fibers formed by tumor cells. The tumor is cell-poor and nuclei are of ovoid or elongated shape. They present no cellularity.
In scientific literature there are very few reported cases of head and neck desmoid tumors. Incidence can be ascertained at 9.5 to 33%, out of which 85% are found in the neck. Other less frequent sites have also been reported like face, oral cavity, scalp, paranasal sinus and orbit.11-14 They can appear at any age rank, although their appearance is most frequent in patients between their 3rd and 4th decade of life.
There are no characteristic radiographic signs. In general terms, it is a translucent lesion which expands the cortical and thins it. The lesion is surrounded by a thin margin of reactive bone. When scintigraphically observed (gammagraphically), a radiotracer uptake increase can be observed in the inside of the lesion.
Radiation can be prescribed only in cases of inoperable tumors, or cases of residual disease after marginal surgery has been performed.15
As final observation, it can be noted that the following have been described as effective: Progesterone, AINE, warfarine. Vitamins C and K, tamoxifen, testolactone, and some antineoplastic agents like adriamycin dacarbazine, vincristine etc.2 The use of antiestrogen and anti-inflammatory agents has also been recommended as treatment for tumors not suitable for resection.16,17
REFERENCES
1. Cotrán RS, Kumar V, Collins TR. Patología estructural y funcional. 6ta edición. Ed. McGraw Hill Interamericana: España, 2000: 1308-9. [ Links ]
2. Siegel NS, Bradford CR. Fibromatosis of the head and neck: a challenging lesion. Otolaryngol Head Neck Surg 2000; 123: 269-75. [ Links ]
3. Allen E. Tratado de cirugía ortopédica . Tomo I. Ed. Panamericana: México, 1996. [ Links ]
4. Tan YY, Low CK, Chong PY. A case report on aggressive fibromatosis with bone involvement. Singapore Med J 1999; 40 (2): 111-2. [ Links ]
5. Abrams GD. Disturbances of growth, cellular proliferation and differentiation. In: Price SA, Wilson LM. Pathophisiology. Clinical concepts of disease processes . 4th edition. International: Mosby, 1992: 94-5. [ Links ]
6. Tejpar S, Nollet F, Li C, Wonder JS, Michils G, dal Cin P. Predominance of beta-catenin mutations and beta-catenin dysregulation in esporadic aggressive fibromatosis (desmoid tumour). Oncogene 1999; 18 (47):. [ Links ]
7. Bertario L, Russo A, Sala P, Eboli M. Genotype and phenotype factors as determinants of desmoid tumors in patients with familial adenomatous poliposis. Int J Cancer 2001; 95: (102) 6615-20. [ Links ]
8. Peterschulte G, Lickfeld T, Moslein G. The desmoid problem. Chirurg 2000; 71: 89. [ Links ]
9. Tostevin PMJ, Wyatt M, Hosni A. Six cases of fibromatosis of the head and neck in children. Int J Pediatr Otorhinolaryngol 2000; 53: 235-244. [ Links ]
10. Enzinger FM, Weiss SW. Soft tissue tumors . 3rd ed. St Louis: Mosby; 1995. [ Links ]
11. Masson JK, Soule EH. Desmoid tumors of the head and neck. Am J Surg 1966; 112: 615-22. [ Links ]
12. Conley J, Healy WV, Stout AP. Fibromatosis of the head and neck. Am J Surg 1996; 112: 609-14. [ Links ]
13. Gnepp DR, Henley J, Weiss S et al. Desmoid fibromatosis of the sinusal tract and nasopharynx. A clinicopathologic study of 25 cases. Cancer 1996; 78: 2572-9. [ Links ]
14. Rao BN, Horowitz ME, Parham DM et al. Challenges in the treatment of childhood fibromatosis. Arch Surg 1987; 122: 1296-8. [ Links ]
15. Lackner H, Urban C, Kerbl R, Schwinger W, Beham A. Noncytotoxic drug therapy in children with unresectable desmoid tumors. Cancer 1997; 80 (2): 334-4. [ Links ]
16. Ballo MT, Zagars GK, Pollack RA. Desmoid tumor: Prognostic factors an outcome after surgery radiation therapy, or combined surgery and radiation therapy. J Clin Oncol 1999; (17): 158-167. [ Links ]
17. Leithner A, Schnack B, Katterschatka T, Wiltschke C, Amann G, Windhager R et al. Treatment of extra-abdominal desmoid tumor with interferon-alpha with or without tretinoin. J Surg Oncol 2000; 73 (1): 21-5. [ Links ]
BIBLIOGRAFÍA COMPLEMENTARIA
18. Batsakis JG, Raslan W. Pathology consultation extraabdominal desmoid fibromatosis. Ann Otol Rhinol Laryngol 1994; 103: 331-4. [ Links ]
19. El-Sayed Y. Fibromatosis of the head and neck. J Laryngol Otol 1992; 106: 459-62. [ Links ]
20. Eitamo JJ, Hayry P, Nykri E et al. The desmoid tumor I. Incidence, sex, age, and anatomical distribution in the finish population. Am J Clin Pathol 1983; 77: 665-73. [ Links ]
21. Welling RE, Hermann ME, Kasper GC. Experience with desmoid tumor in a community teaching hospital. J of Surg Oncol 1992; 49 (2): 113-5. [ Links ]
22. Enzinger FM, Shiraki M. Musculoaponeurotic fibromatosis of the shoulder girdle (extra-abdominal desmoid). Analysis of ten cases followed up for ten of more years. Cancer 1967; 20: 1131-40. [ Links ]
23. Das Gupta TK, Brasfield RD, O Hara J. Extra-abdominal desmoids: a clinicopathologic study. Ann Surg 1969; 170: 109-21. [ Links ]
24. Johns MM, Taylor RA, Bogdasarian RS. Quiz case 2. Arch Otolaryngol Head Neck Surg 2000; 126: 905. [ Links ]
25. Hayry P, Reitamo JJ, Totterman S et al. The desmoid tumor. II. Analysis of factors possibly contributing to the etiology and growth behaviour. Am J Clin Pathol 1982; 77: 681-5. [ Links ]
 Correspondence address:
Correspondence address:
Dr. Doroteo Vargas López
Hospital Regional ''Lic Adolfo López Mateos''
Av. Universidad 1321, Mexico City.
E-mail: dovarlo@yahoo.com.mx
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 text in
text in 


