Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.16 n.1 Ciudad de México Jan./Mar. 2012
Original research
Nasoalveolar bone graft integration range in patients with cleft lip and palate sequels
Alejandro Montaño López,* Héctor Rincón Rodríguez,§ Carlos Landa SolísII
* Maxillofacial and Oral Surgery Service HMG Hospital, Coyoacan, Mexico, General Pathology professor, Centro de Estudios Tecnológicos Industrial y de Servicios (Industrial Technology and Service Center). Mexico.
§ Head of Pediatric Maxillofacial Surgery, Stomatology Department, Mexico's Children Federico Gomez.
II ''B'' Research Assistant, Yissue Engineering, Tissue Therapy and Regenerative Unit, Instituto Nacional de Rehabilitación (Unit, Rehabilitation National Institute), Mexico.
ABSTRACT
Introduction: Cleft lip and palate are growth and development conditions accounting for 15% of congenital malformations, and are associated to external and internal factors. One of the most linked sequels to this condition is the nasoalveolar cleft (NAC). Treatment for this condition is generally based on a periosteal surgery or a bone graft. These can be classified according to the age or time when they are administered, as well as to the type or nature of the material used. Objective: To determine bone integration extent in nasoalveolar secondary bone grafts, obtained from the iliac crest in patients with unilateral cleft palate and lip sequels (CPLS) surgically treated following Dr Phillipe Boyne's technique, published in 1972. These patients were treated at the Maxillofacial Surgery Service of the Mexico's Children Hospital, Federico Gomez. Methods: 104 clinical and radiographic files of unilateral CPLS patients were examined. Patients age range was 7 to 14 years. Patients were classified according to the following criteria : gender, age, side of the cleft and development of complications. Grafts were radiographically evaluated, height with respect to the nasal floor was determined, and grafts were classified according to publications by Brusati and Garattin in 2,000. Results: A dependence was established between the extent of bone integration and the development of complications. No other dependence was observed in any of the variables. Conclusions: In the sample of studied population, Dr Philippe Boyne s technique for reconstruction of NAC and CPLS with extirpation and application of the iliac crest was very effective since adequate amounts of bone integration were achieved.
Key words: Nasoalveolar bone graft, nasoalveolar cleft, bone integration.
INTRODUCTION
Growth and development disorders associated to the craniofacial region are of a very diverse nature. Within their scope we include oral and facial clefts or fissures. The most frequent oral and facial fissures are nasolabial and nasopalatine, these are also known as cleft lip (CL) and cleft palate (CP). In due time, general classification of these fissures will be mentioned.
From the embryological point of view, labiopalatine clefts are defined as alterations of the development and union of the facial embryological processes. Specifically, CL develops due to a lack of thickening of the mesoderm and of the lateral and medial nasal processes. These are initially joined by a thin epithelial wall in their most lower or caudal region. At this point, around the fourth week of gestation, the mesoderm must migrate towards the cephalic region and the midline, invading thus this epithelial attachment (union) and allowing the thickening of the same, which now is also composed of mesenchymal tissue. A continuity is thus created between both processes; enabling thus the formation of the upper lip architecture, and the consequent formation of the nasal floor.
Deficiency of this phenomenon generates an evident lack in the mesodermal tissue migration. And this culminates in the resorption of the primitive epithelial union bridge and producing a more inferior border of the medial and lateral nasal processes up to the base of the nasal cavity.
The nasopalatine fissure is formed by the horizontal processes pertaining to the maxillary process. At around the seventh week of gestation, the borders of mesenchymal tissue covered with epithelial tissue must develop a migration towards the midline and must later bond with the contralateral portion originating thus the floor of the nasal fossae as well as the palatine vault or ceiling. This develops due to the apoptosis phenomenon which must be expressed by the epithelial cells from the covering of the aforementioned medial borders in both processes. This allows the exposition of mesenchymal tissue, later migration, as well as contact and union of these processes, and, finally, their re-epithelialization. Apparently, in the case of CP, this apoptotic process of the palatine processes of the epithelial border does not take place; the presence of the tongue in the fissure sometimes contributes to this situation, since, in a normal situation, the tongue should descend to allow for this union.1,2
Nasal and palatine fissures, from the etiological point of view are considered two pathologically different entities from the pathological or embryological standpoint. Nevertheless they are considered to be intimately related in their genetics and function, for these reasons they are considered a congenital disorder with a genetic component.1
We can specifically classify etiological agents of cleft lip and palate into:
Intrinsic or genetic factors.
Extrinsic or environmental factors.
In the genetic factor group we include cases of a single disorder, as those associated to syndromic complexes. Less than 40% of all LPC have genetic etiology. If a child is born with LPC, and neither of the parents is so affected, there is a 4.4% possibility of the next child being afflicted with CLP. In cases when one of the parents is affected by CLP, there is a 3.2% chance that the first born child develops CLP. If this is the case, there is a 17% probability of CLP development in the second child.2
With respect to syndromic disorders associated to CLP, we can mention the following:
a) 21 Trisomy or Downs syndrome. In this section the following anomalies are included: mental retardation, auricular dysplasia, macroglossia, mandibular prognatism, heart disease in 12 % of cases, and CLP in 6% of cases.
b) 17-18 trisomy or Edwards syndrome. Here we can include mental retardation, congenital heart malformations, low insertion of auricular pavilion, hyperlaxity of limbs, micrognatia, renal function alterations, bone malformations, as well as CLP in 15-17% of cases.
c) 13-14 trisomy or Patau syndrome. In this disorder, the following factors are observed: mental retardation, congenital heart defects, deafness, eye development alterations, micrognatia, auricular dysplasia, urogenital disorders and CLP in 70 to 80% of cases.
d) Van der Woude syndrome. This is a dominant autosomal disorder. Non linked to gender, associated to the deletion of the 32 chromosome. It is characterized by cleft lip and/or palate, fossae in the lower lip (vermillion border) linked to defects in the minor salivary glands, partial maxillary anondontia, ankyloglossia , as well as temporomandibular joint disorders. Other manifestations have been reported such as: heart and leg malformations. This syndrome occurs in approximately one out of every 100,000 live births. 2% of CLP patients are linked world wide to this syndrome.
e) Tracher Collins syndrome. This constitutes a dominant autosomal disorder, not linked to gender and affecting the structures of the first and second branchial arches. It is characterized by hypoplasia which in the lower jaw can be moderate or severe, cygomaticapofisis of the temporal bone, maxillary jaw, malar bone and middle to external ear (microtia). Linear coloboma of the lower lid middle third can be observed (50% of reported cases) as well as antimongoloid obliquity. 30% of cases are associated to CLP and 15% to macrostomia.2,3
f) Cardiofacial Veil syndrome (Shprintzen syndrome). This constitutes a dominant autosomal disorder associated to the deletion of the 22 chromosome. It is characterized by CLP, heart anomalies, slow learning, as well as several endocrine, orthopedic, ophthalmologic an immunological non constant alterations.4
g) Robins sequence. A set of face and mouth alterations characterized by micrognathia, glossoptosis, and distinctive ''u'' shaped cleft palate. The severity of micrognathia can give rise to obstructions of the upper airway.5
In the case of environmental factors, which are considered as directly linked to hereditary disorders, we beg to mention the following:
a) Infectious agents. In this section we can mention the most frequent: congenital rubella (togavirus) which, besides CLP can originate ophthalmic malformations (cataracts, chorioretinitis, glaucoma and microphtalmia; ear malformations, mainly associated to deafness through lesions of the Corti organ; heart malformations which manifest through the persistence of the ductus arteriosus, septal defects as well as auricular-ventricular malformations and pulmonary stenosis. Also included in this section are other infections due to cytomegalovirus, congenital toxoplasmosis ( Toxoplasma Gondii ) and congenital syphilis ( Treponema Pallidum ).6
b) Pharmacological agents. Pharmacological groups associated to this condition are: Corticosteroids (cortisone), benzodiazepines, anticonvulsants, thalidomide, and antimetabolites such as aminopterin and methrotexate which antagonize folic acid metabolism. In this group we are also including hormonal deficiencies, where growth hormone deficiencies is a factor associated to CLP development. Retinoids, as well as tobacco and alcohol consumption have also been associated as etiological agents.6
c) Physical agents. In this group we mainly find Roentgen or x radiation which besides being linked to CLP cases, is associated to microcephaly, spina bifida and alterations in limb development. The development of pathological (fever) or induced (sauna) hyperthermia, has been in addition related to SNC alterations and neural tube defects.4
d) Other congenital agents. In this group we can mention severe oligohydramnios, which can generate anterior-posterior compression on the lower jaw in the placental membrane walls. This will prevent the descent of the tongue and preclude the union of the horizontal portions of the maxillary processes. This is one of the causes for Robin s Sequence.1,4
When speaking from the epidemiological standpoint, lip and palate clefts are two different entities which can occur either isolated or together, as has been already mentioned.7 It is considered a relatively frequent condition, and constitutes 15% of hereditary malformations, being second only to club foot and congenital heart defects.8,9 In Subjects afflicted with CLP, 45% of cleft lip cases are associated with cleft palate, 30% of cases present only cleft lip and the remaining 25% present cleft palate only. Unilateral cleft lip presents a 2:1 ratio. More cases are observed in the left side, this 2:1 ratio also applies to the male: female ratio. Cleft lip proportion is 1.5:1 in males with respect to females.10
Cleft lip and palate, presented as isolated pathological entities, present an incidence of 30 % and 20 % respectively, the remaining 50% is accounted for in cases where both conditions appear together. We must mention that, in cases of isolated cleft palate, 40 to 50% of reported cases are associated to some systemic condition or congenital malformation. In cases with isolated cleft lip only 7 to 13% of cases bear this relationship and in cases of combined cleft lip and palate, 2 to 11% of cases are thus related.9,10 Mean world ethnic incidence of live births is expressed as follows:
a) In Mexico: 1:700
b) In Latin America: 1:650
c) Caucasia race: 1:1,000
d) Asian races: 1:500
e) African races: 1:2,000
The classification of cleft lip and palate is subject to great controversy due to the multiple criteria that can be used to reach that goal. The most accepted and established lip and palate cleft classification in the course of the last 70 years are:
a) Davies and Ritchie. Clefts are grouped in three categories:
I. Anterior (nasolabial) clefts.
II. Posterior (palatine) clefts.
III. Nasolabial and palatine clefts.
b) Veau. Four groups are formed (either numerical or alphabetical). Group 1 or A includes fissures of the soft palate, group 2 includes fissures of both soft and hard palate, group 3 or C includes defects of palate and alveolar ridge, which generally unilaterally involve the lip, and group 4 or D which includes bilateral fissures.
c) Kernahan and Stark. The incisive foramen acts as division point between the two embryological entities which involve CLP; they are named primary and secondary. Labiopalatine clefts are divided into four groups: A) primary labial clefts, B) soft palate clefts, C) hard palate clefts, D) palatine and lip clefts.
d) The National Confederation of Plastic And Reconstructive Surgery mentions three groups: a) alveolar and labial defects, b) primary and secondary palate clefts, and c) any combination of clefts involving both primary and secondary palate.4,10
Other well accepted classification and nomenclature is based upon the anatomical description of clefts.
Cleft lip with or without cleft palate:
a) Unilateral left clip
b) Unilateral cleft lip and palate
c) Bilateral cleft lip
d) Bilateral cleft lip and palate
Cleft Palate:
a) Cleft palate
b) Submucosal palate
c) Velopharyngeal insufficiency
d) Robin's sequence
We must also incorporate into the classifications the following adjectives: 1) ''incomplete'' when anatomical extension in the labiopalatine cleft is so expressed, 2) ''primary'' when the lip and palate cleft involves the most forward region of the premaxilla and 3) ''secondary'' when it affects the posterior region of the apical foramen regardless of whether it affects the soft palate, the hard palate, or both.
Treatment of palate and lip clefts involves many disciplines. We can divide treatment into two broad categories: surgical and non surgical. The scope of the present paper will only describe the first mentioned category.
Surgical treatment for cleft lip and palate can be classified into two stages: primary and secondary.
Primary surgical treatment encompasses the closure of cleft lip and palate (primary closure) as well as a nasal surgical review and the correction of nasopharyngeal insufficiencies. These events are normally carried out during the patients first five years of life. Nevertheless, some authors mention that primary procedures must be limited to the closure of cleft lip and palate. Specifically, with respect to primary closure of cleft lip, there is the trend to perform an early closure, at the postnatal stage. This due to the fact that the phoetal collagen levels are still high, and this guarantees a better connective tissue regenerations, avoiding thus the development of conspicuous scarring. Likewise, the presence of considerable amounts of maternal immunoglobulin and natural plasma corticosteroids reduce possible postsurgical complications. Another advantage of cleft lip early primary closure is that it allows for better patient feeding, and parents and family experience psychological acceptance.4 Nevertheless, not all reports on primary closure have been positive. Some authors have initiated controversy pointing out to the possibility of complications occurring during anaesthesia due to the relatively larger amount of drugs required, greater difficulty when intubating as well as the smaller anatomical dimensions of the cleft lip. This admits then to consider a criterion of a longer waiting time for this primary closure. Among other elements, Wilhelmsen and Musgrave 196615 ''rule of ten'' can be observed (a minimum of 10 mg hemoglobin, at least 10 pounds of weight, up to ten thousand leukocytes and 10 weeks of life). In an almost parallel manner, Veau suggested that the optimum time for the procedure was when the patient reached 18 months of age, supporting his claim by stating that this is the period in which the patient initiates the process of language. Nevertheless, other studies showed that an early closure can be performed from 6 months onwards, based on the development of an improved muscular activity of the soft palate muscles, a better velopharyngeal competence which results from a smaller scar flange applied to the soft tissues of the cleft palate. The early closure of the hard palate considerably compromises maxillary anteroposterior growth; for these reasons it has been suggested to postpone closure until the patient reaches 18 months of age. The main objectives to strive for in a primary closure process are: a) optimize feeding, b) improve airway, especially in syndromic associations or cases which might imply mandibular retrognathia, c) treatment of middle ear conditions where palatine fissure conditions a serous otitis due to the sphincter muscle insufficiency of the mouth of the auditory tube d) decrease of velopharyngeal insufficiency, which promotes hypernasal voice. Age is considered the main criterion when programming the closure, since speech develops fixation in the cerebral cortex at around six years of age.
The second surgical stage, also known as secondary, begins at around the patient's 7 years of age. It involves treatment of nasoalveolar fissures and fistulas (NAF), orthodontic and orthopedic correction of maxillary-mandibular skeletal disharmonies or deficiencies. In these, common denominators are jaw anterior posterior and transversal hypoplasia, as well as the vertical growth of the mandible. The aforementioned is known as cleft lip and palate sequels (CLPS).12
Within this state of secondary surgical treatment, we specifically refer to NAF treatment procedures, where the bone defect elicits an important sequence of functional and aesthetic sequels, which involve soft and hard tissues and is frequently associated to the presence of nasoalveolar fistulas.
One of the fundamental principles of NAF treatment is the closure of fistulas whenever present, and their reconstruction with a bone graft.
Through the years, several materials have been used to reconstruct human bone defects. In 1901, Dr Von Eiselberg, considered one of the pioneers of NAF treatment, applied a pedicle bone graft to correct an alveolar defect.14 At a later date, in 1907, Dr Axhausen performed one of the greater contribution to the area of bone transplant and osteogenesis: He formulated the biological principle that the periosteum stimulated osteogenesis cellular index from certain autologous grafts. This ocurrence is considerably low in the event of heterografts and practically nil in xenografts. His research provided the bases upon which bone graft biology, as we nowadays know it, was developed.3,14 In 1914, Dr Drachter performed the first attempt of a nasoalveolar bone graft for the reconstruction of NAF.
NAF reconstructions through autologous primary bone graft application were very popular during the 50's, in 1955 specifically with Dr Nodin, who is considered pioneer of NAF reconstruction with autologous graft. He performed this procedure in an attempt to prevent maxillary collapse, achieve transversal stability, and at the same time allow optimal craniofacial growth, thus facilitating eruption of primary teeth at the graft site. In spite of these expectations, Dr Jolley, in 1968, determined that, in the long run, patients showed considerably compromised facial growth and high incidence of malocclusion phenomena.11
After this trend, came the technique of primary surgical periosteal surgery. In it, only closure of soft tissues was created, with the aim of promoting bone growth at the fissure site through the biological principle of stimulation or periosteal induction. This aim was partially met when obtaining narrow bone bridges which reconstruct the fissure with the advantage of not disturbing facial growth. Nevertheless, the amount of newly formed bone was not sufficient to cover necessary objectives or expectations, and neither was it sufficient to meet requirements or objectives for a nasoalveolar reconstruction graft.8
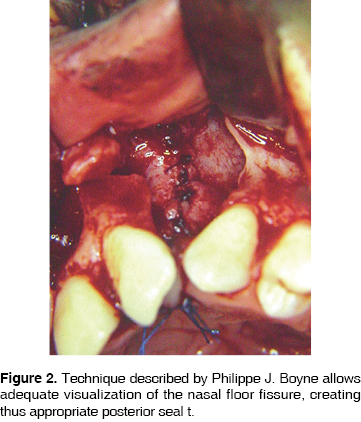
In the decade of the seventies, secondary reconstruction of nasoalveolar fissures gains new importance with the 1972 publication of surgeons Phillipe J. Boyne and N.R. Sands: ''Secondary Bone Grafts in Palatine and Alveolar Clefts''. In this essay, NAF secondary reconstruction concepts are reinforced and a new technique is presented (Figure 1). This technique allows, among other advantages, an appropriate closure of the nasal floor through the dissection of the mouth's nasal mucosa (Figure 2). It also affords application of a more considerable volume of bone tissue (Figure 3), which grants better expectations of the NAG. This subject will be dealt with at a later moment. Due to all the aforementioned reasons, this technique is then considered part of the protocol for treatment of NAF with NAGin the present study.


As mentioned before, establishing biological bases for a bone graft allowed the determination of ideal criteria and properties for bone reconstruction materials. These are: 1) biocompatibility, 2) viability, 3) osteogenic potential, 4) bone matrix neoformation and 5) mechanical stability.
Through biological development and clinical evolution, these criteria have indicated that autologous bone is a primary choice for bone reconstruction.
We also deem important to mention the nasoalveolar graft classification. NAG classification based on application chronology can be as follows:
Early secondary bone grafts: Early secondary bone grafts are performed during the primary dentition phase, which varies from 2 to 5 years of age. Presence of bone tissue to allow eruption of primary dentition as well as provide appropriate periodontal health is one of the fundamental considerations for this early graft. Notwithstanding, in patients subject to this type of grafts, some alterations and deficiencies in hemifacial growth and development have been observed.
Secondary bone grafts: Secondary bone grafts are applied during the mixed dentition stage, which varies between 6 and 12 years of age. Most authors consider this the optimal moment to place a graft, since the bone provides support for the eruption of the permanent cuspid at the site of the fissure, it also provides sufficient bone tissue to give appropiate height to the alveolar process. In these cases there is expectation of minimal interference with facial growth.12
Late secondary bone grafts: Bone graft requirements in a skeletally mature patient are much lesser than those of a young one. Te need for bone tissue to allow dental eruption is made unnecessary. No alteration whatsoever in facial growth is observed in this type of grafts.12
It was previously mentioned that NAF reconstruction is part of LPF sequels treatment. An important factor among these sequels will depend directly on the development of an hypoplasia, a hypofunction, or a combination of both, in hard and soft tissues of the anatomical regions involved in the fissures. Therefore, the main objective of the surgical correction of these deformities or sequels must focus on the re-establishment of a proper physiology which will later allow optimal facial growth.8
For all the aforementioned reasons, nasoalveolar bone grafts must ideally comply with the following characteristics:
1) Allow the closure of the nasoalveolar anterior fistula.
2) Provide sufficient bone tissue to the fissure site, not only to allow the proper eruption of the permanent cuspid but also provide maxillary stability (premaxilla) and provide appropriate root support to teeth involved in the fissure.
3) Provide a proper bone architecture (continuity) to the premaxilla region, providing at the same time optimal lip support.
4) Establish a functional airway in the nasal cavity involved with the lip and palate fissure.
5) Provide appropriate bone volume to allow the best possible dental rehabilitation.1,12
Among controversial points related to nasoalveolar bone grafts the following can be mentioned: a) surgical time required for NAF reconstruction, b) type of bone and donor site to be used for the graft, c) orthodontic and orthopedic aspects involving the fissure site such as maxillary expansion for the correction of anterior-posterior discrepancies.11
In this study we are going to stress on donor bone types and sites.
We have already mentioned there is an ample array of materials taken from the human body for the reconstruction of bone defects. Two main groups can be observed:
• Bone grafts or transplants which are divided according to their origin into autologous grafts (those harvested from the same individual where the graft is going to be applied), homologous grafts (those obtained from different subjects belonging to the same species) and heterologous grafts (obtained from subjects of a species different from that of the receptor). These biological materials are subject to varied processes like freezing, deminerilization or lyophilization, which allow, among other properties, to modify the graft's antigenic capacity. The second group encompasses aloplastic materials, these are all of synthetic or semi-synthetic materials which allow to achieve bone reconstruction. Among these we can mention hydroxyapatite of even synthetic bone.
Research and experience of several authors have demonstrated that autologous bone grafts cover the best part of expectations for bone reconstruction grafts. This quality is mainly due to the ability of the bone to integrate to the recipient bed through the biological processes of osteogenesis, osteoconduction and osteoinduction.12
Within the category of autologous bone grafts we can find three variants: a) bloc non vascularized cortical cancellous bone in where the transplants consists of greater amount of bone mineral matrix than bone cellular components; b) vascularized cortical cancellous bone depending for its application on anastomosis of vascular tissues. This has to bear the disadvantage of the size and anatomical shape of the donor site, such the fibula or rib, c) cortical particulate bone or bone marrow which provides adequate cellular density to the graft, mineral components, as well as the bone morphogenetic protein needed for the graft's osteoinduction.
We hereby provide a list of autologous donor sites for maxillofacial region bone reconstruction deemed adequate due to their histological and ossification characteristics as well as to their approach site and convenient amount of bone to harvest:
1) Iliac crest upper border and lateral, anterior and posterior sides.
2) Cranial parietal eminence
3) Mid-lateral side of the tibia
4) Rib (cortical cancellous or costochondral)
5) Chin region
The iliac crest has been systematically used for maxillofacial region bone reconstruction. It presents advantages, since it is possible to obtain from it the three types of bone we have mentioned (cortical, cancellous and cortical-cancellous) and it provides sufficient amount of material. The posterior region of this bone is indicated to obtain larger volumes. The two main disadvantages of using this donor site are based on the fact that this a growth center, which could result affected with the process of donation and the morbidity associated to approach a harvest of the graft. In the first case, the harvesting of the graft in a growing and developing patient, the surgical technique is modified so as to preserve the growth cartilage located at the upper and anterior portion of the iliac crest. In the second case, main morbidity is associated to the lesion of the iliac or gluteus maximus muscles, which, in the patient, elicits pain when walking. Nevertheless, a meticulous tissue dissection and a conservative suture technique will allow adequate reposition of these structures and decrease risk of complications.2
For the aforementioned reasons autologous nasoalveolar bone grafts harvested from the iliac crest are the best alternative for the reconstruction of bone defects of NAF in CLPS patients. Finally concerning the degree or determination of amount of bone present in the grafted NAF, or the degree of bone integration, the evaluation of NAG is based on Bergland O. and Sembs 1986 classification3 as well as on the modification and re-proposal developed by Brusati and Garattini, published in 2000.5 In this latter, classification is determined by the radiographic appreciation of the NAF occlusal projection and its perspective of bone volume based upon the observable radiopacity in the NAF space, as well as its relationship with nostrils and alveolar ridge. All the aforementioned facts allowed the authors to establish the following classification:
Type 1: Bone graft with complete fissure ossification and reconstruction from the floor of the nostrils up to the entirety of the alveolar ridge (100%).
Type 2: Ossification is observed from the nasal floor, reaching a height of three quarters of the alveolar ridge (75%).
Type 3: Graft ossification encompasses from the nasal floor up to a height lesser than two thirds of the height of the alveolar ridge (50%).
Type 4: Ossification is limited to a scant bone bridge amounting to a third of the required bone volume (25% or less).3,5
See figure 2.
Within the important aspects of surgical treatment of NPF we must include handling of possible post surgical complications or sequels. Within the scope of nasoalveolar grafts, the most common complications are soft tissue dehiscence and the resulting bone tissue exposition in the oral cavity; the development of a sinus infectious process which can compromise bone integration process. In the first case, it is more frequent in large NAF (over 10 mm) where oral mucosa flaps can be insufficient for NAF closure and recovering. On the other hand, factors like eating habits and hygiene among others, are elements which can influence in the development of soft tissues as well as in the process of localized infectious process. Development of these complications negatively modifies the objectives sought when closing a nasoalveolar fistula and NAF bone reconstruction. At the beginning of this paper, it was mentioned that the objectives sought with this reconstruction, nevertheless it must be realized that these aims are rarely met at 100%. Within NAF closure and reconstruction protocols the following characteristics are considered the minimum required to consider the nasoalveolar graft as a success: 1) Appropriate closure of nasoalveolar fistula, 2) Sufficient bone tissue integration to allow maxillary stabilization in the premaxilla and 3) eruption of permanent cuspid and/or its later prosthetic rehabilitation. For clarity of expression purposes, ''sufficient degree'' is considered for those NAG which can hold degree I, II or III in the Brusatti and Garatini classification (Figure 4). Those deemed ''not sufficient'' are those determined as grade IV (Figure 5).


PROBLEM APPROACH
Surgeons of the maxillofacial surgery service (MSS) of Mexico's Children's Hospital (Hospital Infantil de México) MCH have been performing an average of 160 surgeries in the last ten years. These surgical events are related to the closure and reconstruction of nasoalveolar fissures (NAF) taken from iliac crest autologous secondary bone grafts, as part of the rehabilitation protocol and treatment of patients with CLPS. These interventions represent over 40% of all surgical procedures performed by staff of this Center. The requirements for scientific and statistical documentation as well as results to back up this therapeutic conduct show the need for a study that will sustain and present important elements that might corroborate, or, in a given case, modify treatment protocol for NAF reconstruction and closure procedures. This study aspires to contribute statistically significant information on the degree of bone integration developed in patients subject of NAF closure and reconstruction processes as well as factors that might modify them.
The aforementioned can be expressed in the following fashion:
a) How many patients have developed bone integration with secondary nasoalveolar grafts of the iliac crest in surgical interventions performed at the Mexico's Children's Hospital's maxillofacial service during 1991 to 2001? And what if any is the degree of bone integration in operated subjects.
b) Which factors such as age (within the secondary graft rank), site ( side) of the fissure and gender of patient could be associated to the NAG bone integration degree?
OBJECTIVES
A) General Objective:
To ascertain the degree of bone integration in patients with CLPS subject of secondary nasoalveolar grafts of the iliac crest at the maxillofacial surgery service of the children s hospital in Mexico City during the period 1991 to 2001.
B) Specific objectives:
1) To obtain frequency of iliac crest secondary nasoalveolar bone grafts performed ond on patients of the Maxillofacial Service of the Mexico s Children s Hospital in the period between 1991 and 2001, and the number of these which developed any degree of bone integration
2) To ascertain whether there is any relationship among factors like age and gender of patient, location of the fissure (side) and the degree of bone integration.
HYPOTHESIS
1) 80% of all NAF reconstruction performed with iliac crest secondary graft at the maxillofacial service of the Mexico, s Children's Hospital developed some degree of bone integration.
2) 70% of patients who experienced some degree of bone integration are within the rank of functional grafts corresponding to degree I, II and III.
RESEARCH DESIGN
a) Type of Research: The present study has been deemed documental since it is based on written and radiographic records of clinical files of CLPS, operated for NAF reconstruction at the Maxillofacial clinic of the Mexicos Children hospital. The study is also retrospective since already performed surgical procedures are subject of research. It is as well longitudinal because the study encompasses patients subject of surgical intervention during the period from 1991 to 2001.
b) Consideration of variables: Variables to be applied to this study are qualitative and quantitative.
1) The independent variable is the degree of bone integration developed in patients subject of a graft.
2) Dependent variables are the following:
i. Side of the cleft (right or left)
ii. Age of patients subject of the surgical procedure
iii. Sex of patients subject of the surgical procedure
iv. Development of complications
1. Postoperative re-fistulization of the NAF.
2. Development of infectious rino-sinusite process.
c) Material: Clinical files and office studies (occlusal radiographs) of unilateral CLPS patients operated at the MFC of the MCH.
d) Method: An initial selection of all files was carried out. These files encompassed all patients operated for reconstruction and closure of NAF from 1991 to 2001. 176 files were obtained. A second selection was later performed in which to admit only patients with diagnose of unilateral CLPS, with reconstruction based solely on autologous bone harvested from the iliac crest, and whose age corresponded to a secondary graft. Finally all cases which lacked sufficient radiographic files to allow evaluation with or without the characteristics just mentioned were precluded, leaving thus a an encompassing sample of 104 files. Clinical file evaluation was initiated, in which the age of patient at the time of the graft was determined. Those found in the lower section of the age rank (7 to 10 years) and those in the higher section (11 to 14 years) were sub-grouped. Other factors considered were gender of patient, side of the NAF and postoperative evolution during the six months following the nasoalveolar reconstruction. Results were included in a resume table. Radiographic characteristics of the graft will allow the to be initially classified as:
1) Integrated
2) Non integrated.
The first classification is based upon radiographic evaluation, which establishes presence or absence of calcified integrated bone tissue (radio opacity) in the NAF zone, regardlessly of the amount, density or in relation to other anatomical sites. The second classification is considered when the radiographic image does not show any trace of calcified bone material (radiolucency) present in the NAF. In the array of NAF, once selected those with presence of bone integration, the amount or degree of bone present must be assessed. This can be determined with a second radiographic assessment, to determine the amount of bone present with the total NAF area, and can be assessed following criteria mentioned by Brusati and Garattini.13
The assessment was undertaken by three members of the MFS of the MCH. Their assessments were averaged.
Finally, results were analyzed applying Chi Square statistical tests, to assess the hypothesis with respect to variables. Fisher's Exact Test was used to determine, at every step, dependence among analyzed variables. Phi test was used to determine whether the cases are sufficient for the analysis. These three tests were applied with STATS v.2. software.
e) Inclusion criteria:
1) Patients who have received a graft at the corresponding age to secondary grafts, with autologous bone harvested from the iliac crest, with procedure performed at the Maxillofacial Service of the Mexico s Childrens Hospital during the period encompassed between 1991 and 2001.
2) Patients with unilateral CLPS.
3) Patients with full (complete) radiographic and clinical file.
f) Exclusion Criteria:
1) Patients with bilateral CLPS.
2) Patients not operated at the MFS of the MCH.
3) Patients nasoalveolar grafts are considered primare or late secondary.
4) Patients whose grafts are not considered autologous in type and harvested from the iliac crest.
5) Patients with insufficient radiographic file.
RESULTS
One hundred and four clinical and radiographic files corresponding to the 1991 to 2001 period were examined. 44.26% (46) corresponded to female patients and 55.76% (58) to male patients. Average age of patients was 11.52 years, with maximum 15 years of age, minimum 8.
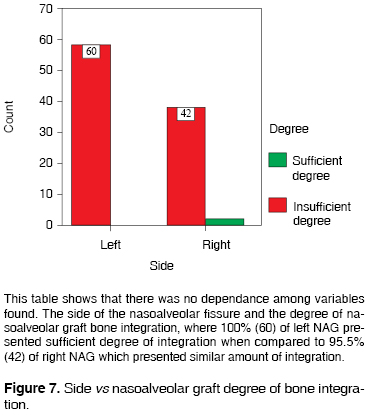
With respect to anatomical location of fissures, 59.61% (62) were on the left side and the remaining 40.48% (42) on the right side.
Total number of grafts presenting sufficient or functional bone integration grades I, II, and III) correspond to 98.07% (102) of cases and the remaining 1.98 % (2) to grafts which did not develop sufficient amount of bone integration (grade IV). These two cases where the graft was considered insufficient were a consequence of rino-sinusitic condition sitis).
Quantitative correlation of the independent variable with dependent variables is as follows:
1) Total number of grafts with grade I integration: (53.84%) (56)
a) Gender
a. Female : 57.14 (32)
b. Male: 42.85% (24)
b) Side:
a. Left: 57.14% (32)
b. Right: 42.85% (24)
c) Age average 9.3 years (max 15, min. 8)
d) Complications: None.
2) Total number of grafts with grade II integration:
a) Gender:
a. Female: 43.75 (14)
b. Male: 56.25% (18)
b) Side:
a. Left: 68.75% (22)
b. Right: 31.25 (10)
c) Age average: 10.8 years (max: 14, min: 8).
d) Complications: 7 (21.8%)
3) Total number of grafts with grade III integration: 13.46 % (14)
a) Gender:
a. Female: 42.85% (6)
b. Male: 57.14% (8)
b) Side:
a. Left: 14.2% (4)
b. Right: 71.42% (10)
c) Age average: 12 years (max: 14, min: 11)
d) Complications: 8 (57.14%)
4) Total number of grafts with grade IV integration: 1.9% (2)
a) Gender:
a. Female: 0%
b. Male: 100% (2)
b) Side:
a. Left: 100% (2)
b. Right: 0%
c) Age average: 9 years (10 and 8)
d) Complications: 2 (100%).



DISCUSSION
Within the scope of the studied sample, 83.3% (87) cases did no present local postoperative complications. All of them experienced sufficient degree of bone integration. The remaining 1.9% which did present complications did not attain sufficient degree of bone integration. When establishing a comparison with the 2000 study performed by Brusati and Garattini which mentions the degree of bone integration developed in a 70 subject sample, and where 100% of cases developed a sufficient degree of bone integration. In those cases presenting right NAF only 95.5% of cases experienced sufficient amount of bone integration.
With respect to this study, the development of NAG complications were classified into two groups: those that, complications notwithstanding, developed sufficient or satisfactory degree of bone integration, and those which did not achieve this goal. The difference is statistically significant.
Subject of the study, were also divided into two groups according to age. The first group encompassed patients ages 7-11, second group comprised patients ages 11-14. In the first group (37.3% of the sample) it was determined that 95% of cases presented sufficient degree of bone integration, the remaining 5% did not achieve this goal. In the second group, (62.7% of the sample) 100% presented sufficient integration degree. The gender of the sample population was determinant, since it revealed that 100% of female patients (48.1% of the sample) showed sufficient degree of bone integration. 96.3% of male patients developed sufficient degree of bone integration, and the remaining 3.7% did not.
See figure 10
The application of the technique described in 1972 by Dr Phillipe J Boyne for the reconstruction of NAF such as CLPS resulted efficient in patients with unilateral LPF, since it permits to obtain bone integration degrees deemed sufficient for the purposes of nasoalveolar grafts. On the other hand, the use of bone harvested from the iliac crest as reconstruction material resulted equally successful. It has been demonstrated that there is a significant degree of dependence among patients with sufficient degree of bone integration and the development of complications, especially those related to infection. The question of comparative studies among different techniques for NAF closure in comparison to the one here presented also remains on the table. Also of interest would be the attainment of comparative studies of different reconstruction materials.
REFERENCES
1. Johnson DC. Cleft lip and palate. In: Behrman RE, Kliegman RM, Arvin AM, and editors. Textbook of pediatrics. 15th edition. Madrid (ES) McGraw-Hill. 1997; I: 1312. [ Links ]
2. Bloomquist DS, Turvey TA. Bone grafting in dentofacial deformities. In: Bell WH. Modern practice in orthognatic and reconstructive surgery . 2nd ed. Philadelphia: W.B. Saunders; 1992: 834-35, 839-841. [ Links ]
3. Bergland O, Semb G, Abyholm FE. Elimination of the residual alveolar cleft by secondary bone grafting and subsequent orthodontic treatment. Cleft Palate Craniofacial J 1986; 23: 175. [ Links ]
4. Kernahan DA, Rosenstein SW. Cleft lip and palate . Baltimore, Maryland Williams & Wilkins; 1990: 13-18, 115-118. [ Links ]
5. Brusati R, Garattini G. The early secondary gingivoperiostoplasty. Oral and Maxillofacial Surgery Clinics of North America 2000; 3: 443-453. [ Links ]
6. Cohen MM. Etiology and pathogenesis of orofacial clefting. Oral and Maxillofacial Surgery Clinics of North America 2000; 3: 361-376. [ Links ]
7. Bauer BS, Vicari FA. Cleft palate. In: Georgiade GS. Gregory NG, Riefkhol R, Barwick WJ. Textbook of plastic, maxillofacial and reconstructive surgery . 2nd ed. New York: Wiliams & Wilkins 1992: 299-306. [ Links ]
8. Boyne JP. The evolution of guided tissue regeneration, in: alveolar ridge reconstruction/guided tissue regeneration and bone grafting. Oral and Maxillofacial Surgery Clinics of North America 2001; 13: 3. [ Links ]
9. Marx RE. Philosophy and particulars of autogenous bone grafting. Oral and Maxillofacial Surgery Clinics of North America 1993; 4: 599-612. [ Links ]
10. Optiz, Meier, Stoll. Subklew radiographic evaluation of the transplant bone height in patients with clefts of the lip, alveolus palate, after secondary bone grafting. Journal of Orofacial Orthopedics 1999; 60 (6): 383-91. [ Links ]
11. Bardach J, Kenneth ES. Técnicas quirúrgicas en labio y paladar hendidos . Medilibros 1989, Madrid, España. [ Links ]
12. Turvey TA, Fonseca RJ. Facial clefts and craniosinostosis, principles of management . Edit. W.B. Saunders 1996. [ Links ]
13. Amin K, Jefrey WS, Raymod JF. Secondary grafting in the alveolar cleft patient. Oral And Maxillofacial Surgery Clinics of North America 2002; 4: 477-489. [ Links ]
14. Regezi JA, Sciubba JJ. Oral pathology, clinical pathologic correlations . 3a ed. México, D.F: McGraw-Hill; 2000. [ Links ]
15. Vig WL, Turvey TA, Fonseca RJ. Orthodontic and surgical considerations in bone grafting in the cleft maxilla and palate. In: Surgical management of craniofacial deformities . New York: WB Saunders 1998; 2. [ Links ]
 Correspondence address:
Correspondence address:
Alejandro Montaño López
E-mail: amontano.lopez@universomedico.com.mx
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 text in
text in 


