Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.15 n.2 Ciudad de México Apr./Jun. 2011
Case report
Unusual mandibular lesion of central odontogenic fibroma combined with mandibular giant cell central granuloma
Gabriel Cortés Castillo,* Rodrigo Liceaga Reyes,§ Adalberto Mosqueda TaylorII
* Oral and Maxillofacial Surgery Department, ISSEMYM Ecatepec.
§ Oral and Maxillofacial Surgery Department, Hospital Juárez de México.
II Professor, Health Care Department, UAM Xochimilco.
ABSTRACT
It is very hard to find two different lesions in the jaws, but to find a central odontogenic fibroma coexisting with another lesion is even harder. This article presents a case of a 14 years old patient with a central odontogenic fibroma. and a central giant cell granuloma. A literature review is provided.
Key words: Central odontogenic fibroma, central giant cell granuloma, hybrid lesion.
INTRODUCTION
Odontogenic Fibromas are strange tumors.1 The World Health Organization (WHO) defines them as an ectomesenchymal benign proliferation characterized by fibroblastic tissue with a variable amount of odontogenic epithelium inactive apparently.2 WHO classified in two, depending on their location: intraosseous or central (COF) and extraosseous or peripheral (POF), but it does not subdivide COF.3 Gardner in 1980 tried to establish criteria to diagnose POF, separates them into two variables of central lesions, type 1 Simple COF and type 2 WHO COF. The latter with greater cellular content, than the simple one with epithelial cells, that conforms a substantial part of the lesion, and show many collagen fibers and calcifications.4 Different histological varieties of this lesion have been reported although they have not been included in the classification of maxillary neoplasms, as the granular cells type, the OF with a central giant cell lesion and OF with pleomorphic fibroblasts.3
A mandibular central odontogenic fibroma combined with a giant cell central granuloma in a 14 years old patient is presented. The clinical, radiographical, surgical and histopathological features are discussed comparing it with the few cases reported previously.
CASE REPORT
A 14 year old boy was admitted to the dental clinic at the Hospital Juárez de México in July 2004, with a right mandibular tumor like lesion, of apparently 7 months of evolution. The patient reported tenderness and there was no other relevant history for this lesion. The swelling was located from the right second premolar to the third molar zone with vestibular expansion with displacement and mobility of the first and second molar ipsilateral (Figure 1). The panoramic radiograph showed a unilocular radiolucid lesion that extended from the first and second right molars with a very close relation to the third molar, well defined borders and measuring approximately 30 x 20 mm, producing displacement of the teeth involved (Figure 2). The simple CT scan showed a lesion that produced vestibular and lingual cortical slimming and expansion with preservation of the mandibular border (Figure 3).



An incisional biopsy was taken and the histopathological result was as follows: Central Giant Cell Granuloma (GCCG) combined with Central Odontogenic Fibroma. Surgery was programmed for September of the same year.
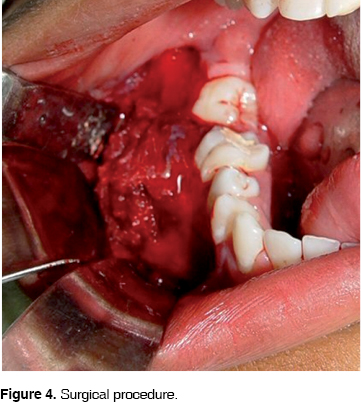
Under general anesthesia and nasotracheal intubation, an outlining incision was designed with distal retromolar extension and anterior vestibular, mucoperiosteal flap elevation, complete curettage of the lesion, extractions of the involved teeth and surgical drilling of the borders, protecting the displaced alveolar nerve (Figure 4). First an absorbable haemostatic sponge was placed in the gap then the mucoperiosteal flap was sutured.
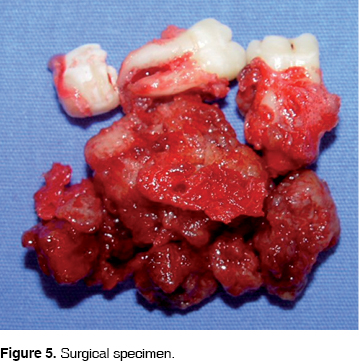
Microscopically the lesion had well defined borders, a rough surface, firm consistency and pale yellow color, producing lingual and vestibular expansion of 40 x 30 x 25 mm (Figure 5).
Histologically the tumor was conformed by fibrocellular vascularized tissue forming cross linked bundles with a scarcity of collagen production.
Histological features: the tumor was conformed by fibro-cellular tissue vascularized forming cross linked bundles of fusiform cells with scarce production of collagen, between them islands and strands of non active odontogenic epithelium were found. In some zones specially in the outer area, there was a highly vascularized fibro-cellular tissue where could be found many osteoclastic giant multinucleated cells type, distributed around vessels and some intralesional hemorrhages (Figures 6 and 7).


On a follow up 2 years after the treatment the patient was found without any clinical or radiographic evidence of recurrence (Figure 8).

DISCUSSION
Among the reported cases of this rare intraosseous lesion with histological features of COF and GCCG Allen et al. reported a three cases series.5 Odell et al referred ten lesions with the same features and suggested that those were hybrid lesions.6 Mosqueda et al reported another case with the same histological pattern.7 It should be noticed that there are not many cases published of this unusual lesion.
The Central Odontogenic Fibroma (COF) is a rare benign neoplasm that only appears in the upper and lower jaws, the reason for this is that the lesion derives of mesenchimal tissue of dental origin: periodontal ligament, dental papilla or dental follicle. The WHO defines it as a fibroblastic neoplasia with a variable amount of seemingly inactive odontogenic epithelium. Some lesions have a certain amount of hard tissue that resembles dysplastic cement or bone.8
COF can appear at any age, but it is more frequent between the second and fourth decade of life, twice more common in women than in men. It can affect either the maxilla or the mandible, posterior or anterior zone of the mouth.8
Svirsky (1986), analyzed 15 cases of COF, he reported that 80% of the cases were in the mandible, 60% of them affected women, ranging from 11-80 years, with a 29 years old.9
Handlers et al, showed among 39 cases, 22 cases maxillar and 17 mandibular, with a range of 3:1 female-male incidence, in patients from 11 to 80 years old.9
Ramer et al revision in 2002, showed a 1:1 mandibular and maxillar incidence, predominating female in 69%. 25 of the 34 mandibular cases were posterior while in the maxilla 25 of 34 were found in the anterior zone; the range of age of the patients was varied from 4 to 80 years and a media of 35 years.9
Radiographically it has been described as a radiolucent area well defined that resembles a unilocular ameloblastoma or an odontogenic cyst and as a radiolucent lesion with well defined borders with a tendency to be smaller than other radiolucent unilocular lesions, while greater lesions frequently are multilocular. In most cases the lesion has well defined borders but also can be seen as a lesion of mixed appearance with difuse borders.8 Sometimes these lesions can be associated with root resorption of the involved teeth.9 There are not radiographic pathognomonic features of COF.
Microscopically the differentiation spectrum is diverse. The simple type COF is mode of star-shaped fibroblasts, fine collagen fibers and an important amount of fundamental substance, scarce amount of odontogenic epithelium; dystrophic calcifications may be found. The WHO type COF along the same features of the simple type can also have odontogenic epithelium and calcifications similar to cement and to dentine. Other histological variants include granular cell type and hybrid tumor of COF and giant cells. The COFs have been related to intracranial aneurysms and tuberous sclerosis.10
It is thought to derive from mesenchymal elements of the dental germ, as the dental follicle, the dental papillae and periodontal ligament and it is possible that in his final and mature spectrum it could be seen as odontogenic myxoma, myxofibroma or odontogenic fibroma.11
The usual treatment of COF is enucleation. Recurrence it is not common. Dunlap and Barrer reported 2 cases of COF treated with curettage with 9 and 10 years follow up without recurrence. However, some cases of recurrence have been reported.9
The Central Giant Cell Granuloma (GCCG) was described by Jaffe in 1953.12 It is a common lesion that represents 7% of all benign tumors of the maxilla.14 The histological features of GCCG have been widely discussed13 and have been defined by WHO as an intraosseous lesion compound of fibrous cellular tissue with multiple hemorrhagic foci and multinucleated giant cells and sometimes inmature bone trabecular tissue.2
The clinical feature of this lesion ranges from an asymptomatic slow growth lesion to an aggressive destructive and painful one with root resorption or dental displacement. The aggressive subtypes of this lesion have a tendency to recurrence after treatment.13 It can be seen more frequently in women than in men around, 30 years of age and it is more common in mandible than in maxilla.15 Commonly this lesion has been found in areas with teeth14 in the anterior zone.
The radiological features have not been clearly defined and there are many contradictory descriptions in the literature.14 The lesion can be found as a uni or multilocular radiolucency with well or badly defined borders and with different degrees of cortical expansion. It is important to notice that this lesion has not a radiologic pathognomonic appearance therefore it can be confused with other maxillary lesions.16
The usual treatment for GCCG is surgical removal. However the surgical treatment varies from a simple curettage to a complete resection of the tumor. The curettage most be follow up by cryosurgery 17 or peripheral ostectomy.18 The GCCG has been recently treated by non surgical methods utilizing systemic calcitonin19,20 or an intralesional injection of corticosteroids.21
The presentation of this unusual lesion associated with COF, shows prevalence in women (12 cases in women to 1 case in men) with a range of age between 5 and 66 years old (average 35.5) more common in mandible (11 mandibular cases compared to 2 maxillary cases); in the mandibular cases the posterior zone was the affected one.7
There are not many publications where the clinical features of this combined lesion can be found. Most of the cases reported were asymptomatic with a slow growth and cortical expansion with dental mobility and in some cases displacement of the teeth. In this case it was observed the relation of the lesion with an impacted third molar that seemed a dentigerous cyst. There were no trauma antecedents or systemic diseases and the bibliography only one case reported showed relation with orthodontic treatment, root canal treatment and antecedent of dental extraction in the zone of the lesion, not knowing if the lesion was pre-existent.
Only one case mentioned a fast growth with expansion and cortical perforation.5-7 Because the scarce number of cases reported and the resemblance with the clinical features of other kinds of lesions, it is difficult to establish the pattern for this combined lesion.
From a radiographical point of view the scarce number of cases reported makes it difficult to compare with previous descriptions of COF and GCCG. Of six cases reported with radiographical description there were 3 unilocular and 3 multilocular lesions.6,7 The case here described showed an unilocular lesion associated with an impacted third molar, and it had a different radiographical pattern.6,7 Kaffe and Buchner reported that 55% of the lesions described as COF had a radiolucent unilocular lesion with well defined borders, and 29.4% were multilocular. The GCCG can have either a multilocular or unilocular presentation and the borders can be well or poorly defined, it can present different degrees of cortical expansion and can be confused with other maxillary lesions.14 It has not been possible to establish a specific radiographic pattern of the combined lesion (COF and GCCG).
The case here reported histologically is formed by fibro-cellular tissue well vascularized forming cross linked bundles of fusiform cells and scarce production of collagen fibers, abundant strings and islands of inactive odontogenic epithelium. In some areas of the fibro-cellular tissue many giant multinucleated osteoclast type cells may be identified specially around the blood vessels and intralesional hemorrhage zones. These findings are similar to those described in the previously reported cases.
Allen et al5 refer to an unusual association of COF and GCCG reaction, thus confirming the presence of a histopathological component and considers the possibility that his cases represent a "collision" of tumors in the same area. This appears to be a very rare probability in which a rare lesion like FOC WHO type develops along with another uncommon lesion like the GCCG.5
An alternative explanation could be that type WHO COF, could by some means evoke a formation of GCCG in these patients. It is important to mention that the aneurismal bone cyst that histopathologically resembles GCCG has been reported in association with a certain number of intraosseous lesions. Recently there have been reports of giant cells reactions in association with ameloblastoma. Some researchers believe that the giant cells identified surrounding the ameloblastoma were more a result of a reactive process than a feature of the lesion itself.5
The paper of Mosqueda et al. mentioned that 3 cases among those published until 1999 (25%) have had recurrence 3 years after the treatment with similar histological findings than the first lesions.7 Allen et al. mentioned that in one of the recurrence cases there were histological components of COF WHO type and giant cells.5
These findings, according to Odell et al, suggest a combination of two entities as a main feature of the lesion therefore they consider it an hybrid tumor.6
So far it has not been possible to determine if the development of COF in a central position produced a surrounding giant cells reaction or if both tissues developed at random in the same place.5
The antecedents of recurrence in the published cases of this type of lesion suggest that it should be treated surgically as GCCG because of its possibility of recurrence, they also suggest to monitor constantly after the surgical excision.
CONCLUSION
Because of the scarce number of reported cases in the literature, it is not possible to establish clinical and radiographical features to diagnose this neoplasia among the group of odontogenic tumors but like most of the lesions only histological findings can confirm this particular entity.
It has not been possible to determine the origin of this lesion or to find out if one of the lesions derives from the other or if they developed simultaneous in the same zone but the recommended treatment should take into consideration the most aggressive component of the hybrid tumor.
REFERENCES
 Address correspondence:
Address correspondence:
Adalberto Mosqueda MD
E-mail: mosqueda@correo.xoc.uam.mx
Nota
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
1. Handlers JP, Abrams AM, Melrose RJ et al. Central odontogenic fibroma: Clinicopathologic features of 19 cases and review of the literature. J Oral Maxillofac Surg 1991; 49: 46. [ Links ]
2. Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumor . Berlin Germany, Springer-Verlag 1992. [ Links ]
3. Nicolás C, Damián A, Mercedes P, Luis J. Central odontogenic fibroma granular cell variant: A case report and review of the literature. J Oral Maxillofac Surg 2002; 60: 1192-1194. [ Links ]
4. Gardner DG. The central odontogenic fibroma: An attempt at clarification. Oral Surg Oral Med Oral Pathol 1980; 50: 425. [ Links ]
5. Allen CM, Hammond HL, Stimson PG. Central odontogenic fibroma, WHO type: A report of three cases with an unusual associated giant cell reaction. Oral Surg Oral Med Oral Pathol 1992; 73: 62. [ Links ]
6. Odell EW, Lombardi T, Barrett AW et al. Hybrid central giant cell granuloma and central odontogenic fibroma-lie lesions of the jaws. Histopathology 1997; 30: 165. [ Links ]
7. Mosqueda TA, Bermudez FV, Diaz FMA. Combined central odontogenic fibroma and giant cell granuloma-like lesion of the mandible: report of a case and review of the literature. J Oral Maxillofac Surg 1999; 57: 1258-l262. [ Links ]
8. Kaffe I, Buchner, Buchner A. Radiologic features of central odontogenic fibroma. Oral Surg Oral Med Oral Pathol 1994; 78: 811. [ Links ]
9. Spencer J, Daniels M. Central odontogenic fibroma of mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 98: 295-300. [ Links ]
10. Rauben HEJ, Noffke CE. Central odontogenic fibroma-like tumors, hypodontia, and enamel dysplasia: review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94:74-7. [ Links ]
11. Zachariades N. Odontogenic fibroma. Int J Oral Maxillofac Surg 1986; 15: 102. 12. [ Links ]
12. Jan de L, Hans P. van den Akker. Clinical and radiological features of central giant-cell lesions of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 464-70 [ Links ]
13. Chuong R, Kaban LB, Kozakewich H et al. Central giant cell lesions of the jaws: A clinicopathologic study. J Oral Maxillofac Surg 1986; 44: 708. [ Links ]
14. Bataineh AB, Al-Khateeb T, Rawashdeh MA. The surgical treatment of central giant cell granuloma of the mandible. J Oral Maxillofac Surg 2002; 60: 756-761. [ Links ]
15. Whitaker SB, Waldron CA. Central giant cell lesions of the jaws. Oral Surg Oral Med Oral Pathol 1993; 75: 199. [ Links ]
16. Cohen MA, Hertzanu Y. Radiologic features, including those seen with computed tomography, of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol 1988; 65: 255. [ Links ]
17. Webb DJ, Brockbank J. Combined curettage and cryosurgical treatment for the aggressive "giant cell lesion" of the mandible. Int J Oral Maxillofac Surg 1986; 5: 780. [ Links ]
18. Eisenbud L, Stern M, Rothberg M et al. Central giant cell granuloma of the jaws: Experiences in the management of thirty-seven cases. J Oral Maxillofac Surg 1988; 46: 376-84. [ Links ]
19. Harris M. Central giant cell granulomas of the jaws regress with calcitonin therapy. Br J Oral Maxillofac Surg 1993; 31: 89. [ Links ]
20. de Lange J, Rosenberg AJ, van den Akker HP et al. Treatment of central giant cell granuloma of the jaw with calcitonin. Int J Oral Maxillofac Surg 1999; 28: 372. [ Links ]
21. Kermer C, Millesi W, Watzke IM. Local injection of corticosteroids for central giant cell granuloma: A case report. Int J Oral Maxillofac Surg 1994; 23: 366. [ Links ]











 text in
text in 


