Introduction
Stroke is one of the leading causes of death and disability worldwide. In 2019, the global burden of stroke had 6.5 million deaths and 143 million disability-adjusted life-years (DALY)1,2. Intracerebral hemorrhage (ICH) represents approximately 20% of strokes and is its most severe and least treatable form.
The incidence of ICH is 3.41 million2,3 but can vary significantly based on geographic location, population demographics, among other epidemiologic characteristics. ICH accounts for 5 to 20% of cerebrovascular disease in high-income countries (HICs); however, in low-and middle-income countries (LMICs), the disease burden is higher for ICH. Although the reasons for the higher burden of disease derived from ICH compared to ischemic stroke are not entirely established in LMICs, several factors have been identified, such as high prevalence of poorly controlled hypertension and high sodium intake in local diets4. Hospital-based studies from Ecuador, Mexico, Chile and Argentina report a proportion of ICH between 23 and 40%5,6. There is also a high incidence of ICH in Asia5 and in black compared to white populations from HICs7.
Additionally, ICH produces the highest mortality (50%)8 and accounts for 42% of all the disability-adjusted years lost due to stroke6 Despite all the above data, there are few ICH data published from LMICs of the Latin American region, and the scarce data available has been mainly derived from single-center hospital registries, which present the inherent selection bias of this type of study9.
The LASE (Latin American Stroke Registry) initiative was instituted using robust data compilation and structured methodology to explore multiple stroke outcomes in a population-based sample from tertiary hospitals in Latin America. The present study analyzes the functional outcome, recurrence and death among LASE participants with ICH.
Material and methods
The LASE is a multicenter stroke registry from tertiary referral hospitals with ongoing stroke registries from Central and Andean Latin America, designed to improve knowledge of stroke In the region. Participating sites recruited patients from January 2012 to January 2017. The corresponding Institutional Ethics Committee approved all stroke datasets by international and local research regulations and waived the need for signed informed consent. Still, the patient or a family member verbally agreed to the record of anonymized data in the registry. LASE data comes from 18 centers located in seven Latin American countries. Ten centers from Mexico [Mexico City (5), Durango, Morelia, Madero and Guadalajara (2)], two from Colombia (Bogotá and Cali), two from Perú (both in Lima), and one center from Argentina (Buenos Aires), Costa Rica (San José), Paraguay (Asunción), and Ecuador (Quito). The complete methods of the LASE registry have been published elsewhere10.
Study’s definitions and criteria
Spontaneous ICH was defined as a blood collection within the brain parenchyma secondary to vascular rupture- that was neither traumatic nor aneurysmal in origin. The inclusion criterion for the present analysis was patients with ICH confirmed by imaging studies. We included cases without a demonstrated aneurysmal or traumatic cause11. The cause of ICH was attributed to hypertension in patients with a history of hypertension with regular o irregular treatment and ICH located in sites traditionally associated with hypertension11. Cerebral amyloid angiopathy is a cerebral deposition of amyloid-β, this etiology was attributed to cases with features such as lobar hemorrhage, lobar microhemorrhages and superficial siderosis12. Only patients aged 18 years and older were included. Cases diagnosed with subarachnoid hemorrhage and those with incomplete information were excluded. Information was collected from the original datasets of each center and compiled into a single database by two authors (FS and MAB). The data includes demographic characteristics such as age, sex, and place of residence. Registered vascular risk factors were hypertension, atrial fibrillation, ischemic cardiopathy, diabetes mellitus, and smoking (current or former). Clinical characteristics, such as the NIHSS and Glasgow Como Scale at admission, were also documented. All patients underwent at least one brain imaging study (CT or MRI) to confirm ICH diagnosis. Clinical outcome was systematically recorded at discharge, as measured by the modified Rankin scale (mRs). Follow-up was not included since most centers only register in-hospital data. A poor clinical outcome was defined as a mRs ranging from 3 to 6, while a good clinical outcome was characterized by a score of 0 to 2. Mortality in this period was analyzed regardless of whether death was considered or not related to ICH.
Statistical analysis
Continuous data is summarized by the mean and standard deviation (SD) or the median and interquartile range according to the results of normality tests (Kolmogorov-Smirnoff test). Categorical data is presented as counts and percentages.
Association analysis of continuous data (age, in-hospital length stay) was done with the Mann–Whitney U or Student t-test according to normality. The chi-squared test or Fisher’s exact test adjustment was employed for dichotomous data (including vascular risk factors, demographics, type of ICH, functional outcome, recurrence, and death).
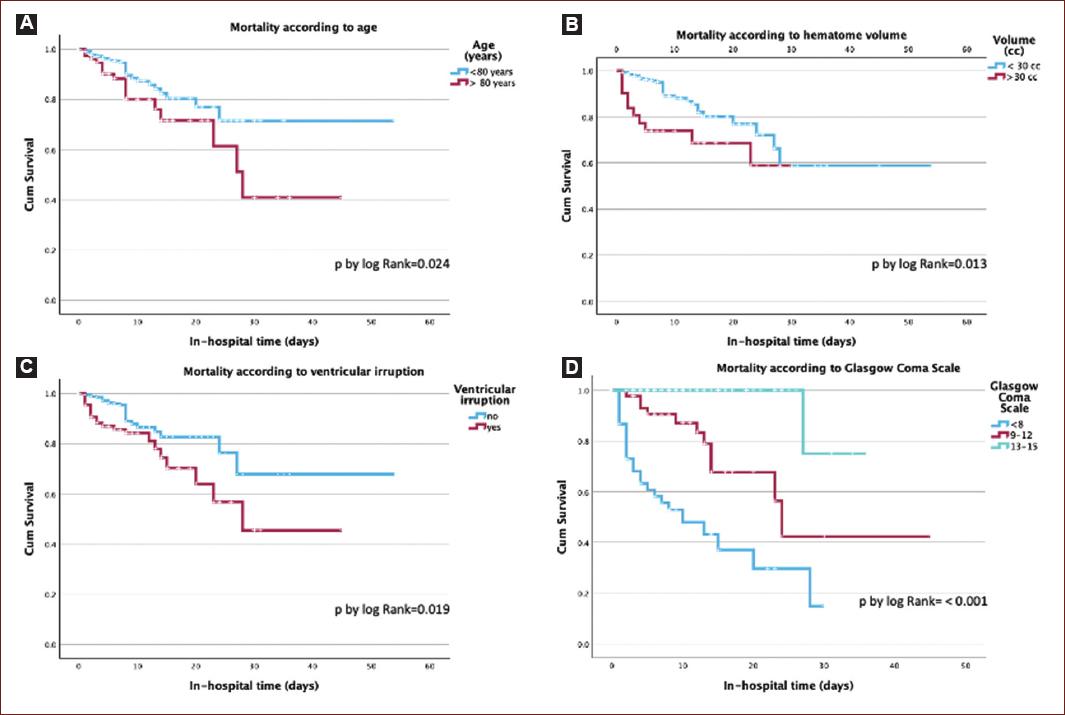
Kaplan–Meier survival curves and the Log-Rank test were utilized to evaluate the absolute risk of death in ICH events during the acute in-hospital period. Significance was defined at p < 0.05. Hazard ratios (HRs) and 95% CIs were calculated.
All statistical analyses were calculated using the SPSS 29.0.1.0 software package (SPSS Statistics for Windows, IBM Corp., Armonk, NY).
Results
Demographics
We recruited data from 5336 patients, 508 of these patents were excluded because of the absence of complete information (medical records and neuroimaging). Only 4828 patients with a confirmed imaging diagnosis and complete inpatient clinical information were included in the analysis. Among these patients, 495 corresponded to intracranial hemorrhage, representing 10.3% of all collected stroke subtypes in LASE.
Of the 18 participating centers, three centers did not contribute patients to the database because their neurosurgery departments were responsible for the evaluation, treatment, and follow-up of ICH patients, and the corresponding clinical neurology departments had no access to the data. The median age of all patients was 64 years (interquartile range, 18-94). Among the patients, there were 285 (57.6%) males (median age, 62 years, interquartile range, 18-94) and 210 (42.4%) females (median age, 65 years, interquartile range, 18-93).
Vascular risk factors
The most common vascular risk factor was hypertension, identified in 339 patients (68.5%), followed by smoking (12.9 %) and diabetes (17.8 %). The predominant etiology was hypertensive in 75 % of cases, 5.9% had arteriovenous malformatios, 4% had no aneurysmal subarachnoid hemorrhage, 3.8% had cerebral amyloid angiopathy, 2.8% were related to drugs (anticoagulants/antiplatelet) and 7.7% were undetermined due to incomplete studies. Table 1 presents the general characteristics and risk factors based on functional prognosis upon hospital discharge.
Table 1 General characteristics, vascular risk factors, etiology and treatment according to functional prognosis at hospital discharge
| Variable | Good clinical outcome mRs 0 - 2 (n = 281 [%]) | Poor clinical outcome mRs 3 - 6 (n = 214 [%]) | Total (n = 495) | p value |
|---|---|---|---|---|
| Age, ya | 73 (24-89) | 67 (37-90) | 68 (24-90) | < 0.001* |
| Male | 176 (62.6%) | 109 (50.9%) | 285 (57.6%) | 0.009 |
| Hospital stay, d | 8 (1-34) | 10.5 (SD 8.3) | 9 (1-30) | 0.280* |
| Risk factors | ||||
| Hypertension | 174 (61.9%) | 165 (77.1%) | 339 (68.5%) | < 0.001 |
| Diabetes mellitus | 35 (12.5%) | 53 (24.8 %) | 88 (17.8%) | < 0.001 |
| Current smoking | 41 (18.3%) | 23 (11.2%) | 64 (14.9%) | 0.121 |
| Coronary disease | 8 (2.8%) | 11 (5.1%) | 19 (3.8%) | 0.188 |
| Hypercholesterolemia | 34 (12.1%) | 31 (14.5%) | 65 (13.1%) | 0.330 |
| Atrial fibrillation | 9 (3.2%) | 13 (6.1%) | 22 (4.4%) | 0.125 |
| Clinical and image | ||||
| NIHSS at admission | 10 (0-23) | 15 (6-32) | 12.5 pt (0-32) | < 0.001* |
| Ventricular irruption | 34 (12.1%) | 53 (24.8%) | 87 (17.6%) | < 0.001 |
| Hematoma volume > 30 cc | 5 (1.8%) | 26 (12.2%) | 31 (6.3%) | < 0.001+ |
| Etiology | ||||
| Hypertensive | 189 (67.3%) | 185 (86.4%) | 374 (75 %) | < 0.001 |
| Amyloid angiopathy | 7 (2.5 %) | 12 (5.6%) | 19 (3.8%) | 0.074 |
| Arteriovenous malformatios | 13 (4.6%) | 16 (7.5%) | 29 (5.9%) | 0.181 |
| Drugs | 4 (1.4%) | 10 (4.7%) | 14 (2.8%) | 0.052+ |
| No aneurysmal SAH | 11 (3.9%) | 10 (4.7%) | 21 (4.2 %) | 0.678 |
| Not determined incomplete studies | 16 (5.7 %) | 22 (10.3%) | 38 (7.7%) | 0.058 |
| Treatment | ||||
| Conservative | 273 (97.2%) | 200 (93.5%) | 473 (95.6%) | 0.048 |
| Medical Intensive | 8 (2.8%) | 14 (6.5%) | 22 (4.4%) | 0.048 |
| Surgical | 13 (4.6%) | 17 (7.9%) | 30 (6.1%) | 0.125 |
aMedian (Interquartile Range).
*P value U-Mann-Whitney Wilcoxon. +Fisher’s Exact Test.
In-hospital outcome
Intracerebral hemorrhage presented an in-hospital bad functional outcome, with mRs of 3-6 observed in 214 patients (43.2%): 62.6% in women versus 50.9% in men (p = 0.009). The stroke recurrence during hospitalization was 5.9% (29 patients).
The mortality rate was 12.5% (62 patients). The risk of death was found non-significantly higher in men (6.9%) compared to women (5.7%) (p = 0.64). The optimal age cutoff for mortality was 80 years, with an area under curve (AUC) of 0.602. The Kaplan Meier survival curves, categorized by age, hematoma volume, ventricular irruption and Glasgow Coma Scale, are presented in Figure 1. However, there is a difference in mortality, with higher frequency, in patients aged over 80 years (HR 1.89, 95%CI 1.07-3.35, p = 0.028), with GCS below 8 (HR 0.19, 95%CI 0.11-0.33, p = < 0.001), ventricular irruption (HR 1.88, 95%CI 1.09-3.24, p = 0.0282), and hematoma volume exceeding 30 cc (HR 2.36, 95%CI 1.17-4.77, p = 0.016).
Discussion
This analysis showed that ICH represents 10% of our registry. This finding is of great importance since it indicates an underreporting of ICH in the region. In some LASE sites, ICH represented less than 5% of stroke cases, which is lower than other reported ICH series. This could be associated with the fact that in some centers, patients with ICH are managed by the neurosurgery service. The management of acute stroke, especially ICH, in Latin America differs from other regions, and several countries do not have a national plan for stroke13. However, many of the ICH cases occur in low and middle-income countries, such as those included in LASE, mainly explained by lower levels of consciousness and poor control of hypertension. In this registry, nearly 60% of the ICH were hypertensive. Management of this critical risk factor could reduce the functional and socioeconomic impact of ICH.
Exploring the factors contributing to ICH within Hispanic populations, the National Institute of Neurology and Neurosurgery-Stroke Registry in Mexico14 highlighted the prevalence of hypertension (85.1%) among ICH patients Our study also identified a high prevalence of hypertension (68.5%) in ICH patients within LASE. Other risk factors revealed in our study included diabetes mellitus in 17.8% of the cases, which is higher compared to other reports where it is 9%15,16.
Our findings also mirrored previous reports, indicating a worse functional outcome among ICH patients. 43% of our cases had poor functional prognosis, with a mortality rate of 12.5%, mainly attributed to advanced age (> 80 years), greater bleeding severity (ventricular irruption and hematoma volume exceeding 30 cc) and GCS below 8. Midline shift, lobar and supratentorial bleeds as well as high presenting SBP and nonconsumption of leafy green vegetables, have also been described as predictors of mortality16.
In the RENAMEVASC (a Mexican stroke registry), a 30-day mortality rate of 30% was reported, with a bad functional outcome present in 31% of the participants17. Romano et al. observed comparable stroke severity between Mexican and Miami Hispanic populations (11.6 + 7.6 in Mexico, 11.3 + 8.4 in Miami, p = 0.84)18, notably, Hispanics in the United States exhibit a heightened risk of ICH compared to non-Hispanic whites (OR 2.6, CI 1.4-6.1)18.
Our study represents a significant collaborative effort in Latin America, encompassing over 4000 patients from 18 diverse hospitals across seven countries. However, it has multiple limitations. First, the study has the inherent bias of retrospective observational studies. Second, there is a sub-representation of ICH cases, which does not accurately represent this stroke subtype’s reality in the entire country. Additionally, the unevenness of the data regarding the distinct aspects of ICH management across the participant countries should be emphasized. Finally, it was impossible to register follow-up data from the participants, which does not add to our understanding of the mid and long-term outcomes of ICH. Despite these limitations, the LASE initiative is and will continue to be a valuable tool to improve stroke knowledge, providing accurate and systematically recorded data from Latin American patients with stroke. Additionally, our findings highlight the urgent need for more reliable data on ICH in Latin America and serve as a call to action to identify and control arterial hypertension early.
Conclusion
Our study demonstrates a poor functional prognosis in 43.2% of ICH patients, with the risk factors for higher mortality being age over 80 years, higher GCS values, and ventricular irruption. Our collaborative study contributes substantial insight into the factors influencing ICH occurrence, prognosis, and outcomes in Latin America. While sharing similarities with global stroke registries, it provides valuable region-specific information that could guide targeted interventions and healthcare strategies. Additionally, the complexities of ethnic and genetic influences on ICH risk are highlighted, as well as the importance of continuous monitoring and improvement of healthcare practices to enhance outcomes in this population.











 text new page (beta)
text new page (beta)