Introduction
Smooth muscle hamartomas (SMH) are rare benign neoformations characterized by increased density of smooth muscle bundles in the dermis and are divided into congenital and acquired. Congenital smooth muscle hamartomas (CSMH) are the most common and present as plaques with hyperpigmentation and hypertrichosis. Conversely, acquired smooth muscle hamartoma (ASMH) is a rare condition with a heterogeneous clinical presentation1. The following is the first case of acquired smooth muscle hamartoma with a sebaceous component.
Clinical case
We describe the case of an 18-year-old male patient with no relevant history of the current condition, who came for consultation due to a pigmented area with excess hair on the left cheek. According to the patient, this condition was uncomfortable because it forced him to shave that area more frequently compared to the contralateral side of the face. The dermatosis had been progressing for a year with no further symptoms. A physician prescribed topical steroids and emollients, but no improvement was observed.
Physical examination revealed a localized dermatosis on the left hemiface affecting the preauricular region, which distributed caudally following the Blaschko lines of the face, passing through the mandibular ramus and gonial angle until reaching the left cheek. The dermatosis consisted of irregular, poorly defined, 2 x 8 cm, a hyperpigmented, grayish-brown plaque with abundant short, coarse hair on its surface and 1-2 mm follicular papules (Figure 1). No piloerection, erythema, or induration of the plaque was observed when the lesion was rubbed (negative pseudo-Darier sign). The evolution had been asymptomatic up to that time.
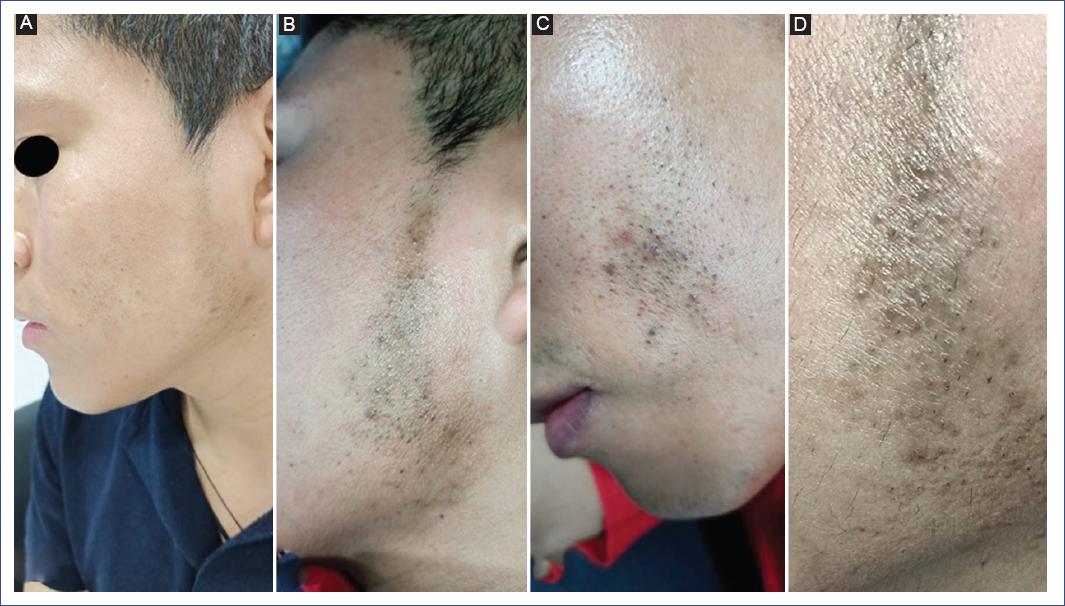
Figure 1 A: plaque following a Blaschkoid distribution on the left hemiface. B-C: the shape of the plaque is irregular, with poorly defined borders in the preauricular region and on the left cheek. D: close-up shows grayish-brown hyperpigmentation, an abundance of coarse, short hairs, and millimetric papular lesions.
The patient underwent two skin biopsies: the first from the left cheek and the second from the left preauricular region. In the first biopsy, orthokeratosis was found covering the epidermis with discrete acanthosis and hyperpigmentation of the basal layer. In addition, a fragment with isolated smooth muscle fiber bundles was identified in the mid-dermis, with no involvement of any other structure at the epidermis or dermis level (Figure 2). The second biopsy showed orthokeratosis with discrete and regular acanthosis and hyperpigmentation of the basal layer with numerous follicular sebaceous structures. Sebaceous glands of different sizes were observed from the superficial dermis to the deep dermis. Miniaturized follicular outgrowths were observed in the follicular component, and numerous intermingled smooth muscle bundles in the external, mid, and deep dermis with collagen disruption and sebaceous glands surroundings. Masson’s trichrome staining was positive, showing enhancement of muscle bundles in red over dermal collagen tissue in blue (Figure 3). Based on the clinicopathologic correlation, acquired smooth muscle hamartoma with a sebaceous component was diagnosed. Treatment with 2% hydroquinone was administered for 3 months, which partially improved hyperpigmentation.
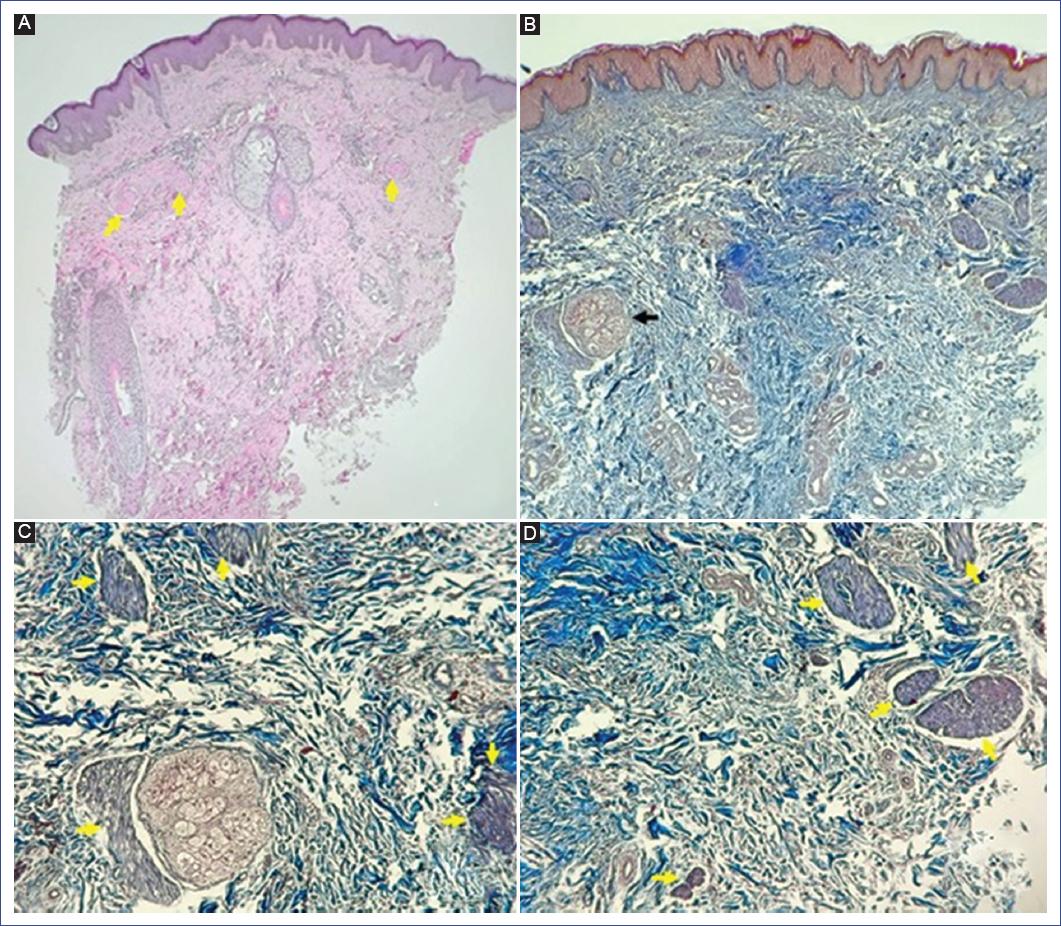
Figure 2 Histopathology of left cheek lesion. A: numerous smooth muscle bundles (arrows) can be observed in the mid and deep dermis. Presence of a small adnexa in the mid dermis and perivascular inflammatory infiltrate (hematoxylin-eosin stain, 4x). B: multiple isolated smooth muscle bundles are observed, one surrounding the sebaceous gland (arrow) with no sebaceous follicle continuity (Masson’s trichrome stain, 10x). C: close-up of the smooth muscle bundles in the collagen surrounding the sebaceous gland (arrows) (Masson’s trichrome stain, 40x). D: close-up of the smooth muscle bundles (Masson’s trichrome stain, 40x).
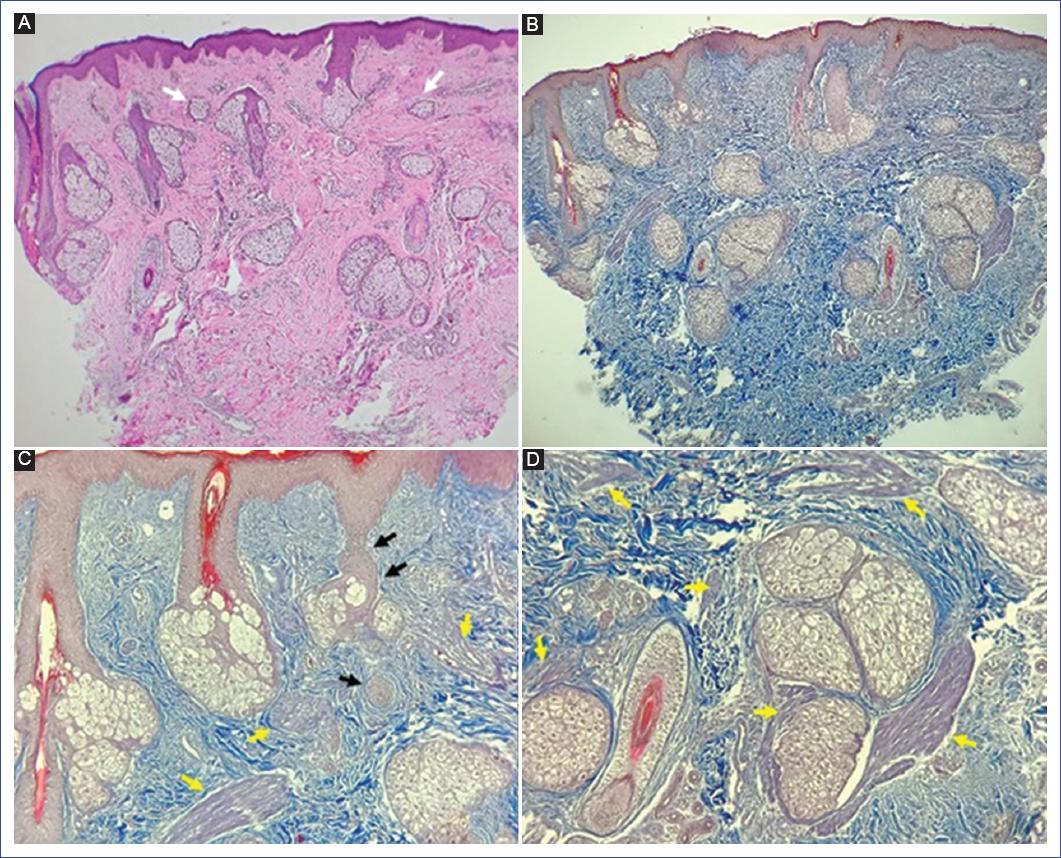
Figure 3 Histopathology of the left preauricular lesion. A: panoramic view showing numerous sebaceous glands, some miniaturized (arrows), and smooth muscle bundles (hematoxylin-eosin stain, 4x). B: abundant smooth muscle bundles embedded in the collagen bundles and surrounding the mature sebaceous glands (Masson’s trichrome stain, 10x). C: abundant smooth muscle bundles in the collagen (yellow arrows); miniaturized sebaceous follicles (black arrows) (Masson’s trichrome stain, 20x). D: smooth muscle bundles (arrows) surrounding a mature sebaceous gland (Masson’s trichrome stain, 40x).
Discussion
The word hamartoma comes from the Greek word hamartomein (to fail, error). Hamartomas are benign neoplastic lesions that combine several cellular elements of various origins. Cutaneous hamartomas are tumor-like malformations in which there is overgrowth and a defective mixture of normal skin components1,2.
A smooth muscle hamartoma (SMH) is a benign proliferation of smooth muscle cells within the dermis. Smooth muscle cells of the skin can be found in the erector pili muscle, scrotal musculature (dartos), vulvar musculature, nipple or areola (muscularis mamillae), and dermal blood vessel wall3,4. Histologically, smooth muscle cells are spindle-shaped with a central cigar-shaped nucleus and eosinophilic cytoplasm without striations1.
Smooth muscle hamartomas can be divided into two types: congenital and acquired. To date, the reported cases of congenital hamartomas showed their origin in the erector pili muscles, and those acquired, in the erector pili mucles, as well as in dartos, vulvar, or dermis blood vessel muscles3-5.
Congenital smooth muscle hamartoma (CSMH) is the most frequent form; the first case was described in 1969 by Sourreril et al.6. Clinically, it presents as a hyperpigmented plaque with hypertrichosis and some papular elements located predominantly on the trunk or extremities. The positive pseudo-Darier sign is considered typical of the congenital form. This sign consists of the triggering transient edema, induration, or piloerection upon rubbing the lesion1,7. This sign represents a neural component of the hamartoma, not an actual histamine release, as seen in the true Darier sign in cutaneous mastocytosis8.
Acquired smooth muscle hamartoma (ASMH) is a rare variety first described by Wong and Solomon in 19855. This form appears later in life compared to the congenital variety. According to a literature search, only 25 cases of ASMH have been described (Table 1).
Table 1 Summary of cases of acquired smooth muscle hamartoma reported in the international literature
| Author/Country | Sex (age) | Time of evolution | Topography | Morphology | Pigmentation | Hypertrichosis | Pseudo-Darier | Symptoms | Location/Origin |
|---|---|---|---|---|---|---|---|---|---|
| Wong and Solomon, 1985 (Country not reported)5 | Male (28 years) | 14 years | Forearm | Solitary plaque of 2-3 cm | Yes | No | NR | Asymptomatic | Dermis and hypodermis, erector pili muscle |
| Darling et al., 1993 (USA)12 | Male (53 years) | 10 years | Neck | Erythematous, indurated plaque | No | No | Negative | Asymptomatic | Dermis, erector pili muscle |
| De la Espriella et al., 1993 (France)14 | Female (18 years) | 3 years | Right breast | 15 cm plaque composed of papules | NR | NR | NR | Asymptomatic | Dermis, erector pili muscle |
| Hsiao and Chen, 1995 (Taiwan)25 | Male (33 years) | 8 years | Scrotum | Multiple skin-colored papular and nodular lesions | No | No | Negative | Asymptomatic | Dermis, dartos muscle |
| Semerci et al., 1997 (Turkey)26 | Male (65 years) | 8 months | Penoscrotal region | Thickening and edema | No | No | NR | NR | Dermis, dartos muscle |
| Quinn and Young, 1997 (USA)27 | Male (60 years) | Several months | Scrotum | 2.8 x 1.8 cm nodular neoformation | No | No | NR | Intermittent purulent drainage | Dermis, dartos muscle |
| Kwon et al., 2000 (Korea)23 | Female (30 years) | 5 years | Vulva (labia majora) | 10 x 4 cm yellowish indurated plaque with multiple 2-5 mm papules | No | No | NR | Pruritus | Dermis, dartos labialis muscle |
| De Alba et al., 2001 (Mexico)11 | Male (18 years) | 3 years | Face (left cheek) | 10 x 5.5 cm plaque with 1-2 mm perifollicular hemispheric lesions | Yes | Yes | Negative | Asymptomatic | Dermis, erector pili muscle |
| Ryu et al., 2002 (Korea)13 | Female (57 years) | 43 years | Neck (right side) | Indurated plaque with skin-colored papular surface | No | No | Negative | NR | Dermis, erector pili muscle |
| Morales-Callaghan et al., 2005 (Spain)9 | Male (18 years) | 2 years | Chest (left side) | Triangular plaque with skin-colored papules and hypertrichosis | No | Yes | Positive | Asymptomatic | Dermis, erector pili muscle |
| Oiso et al., 2005 (Japan)4 | Male (24 years) | 6 months | Scrotum | Diffuse thickening and edema with skin-colored papules | No | No | Negative | Asymptomatic | Dermis, dartos muscle |
| Bari and Rahman, 2006 (Pakistan)15 | Male (19 years) | 7 years | Back and left shoulder | Red-brown indurated plaque, irregular surface, with mottled pigmentation | No | No | Positive | Pruritus | Dermis, erector pili muscle |
| Zarineh et al., 2008 (USA)16 | Male (49 years) | NR | Back (upper left portion) | Nodular pinkish neoformation 1.2 cm with grayish pigmentation in the center | Yes | No | NR | NR | Dermis, erector pili muscle. Two components: melanocyte cords intermingled with smooth muscle bundles |
| Lee et al., 2009 (Korea)3 | Female (21 years) | 18 months | Right sole | Nodular neoformation 0.5x0.5 cm | No | No | Negative | Paresthesia | Dermis, vascular smooth muscle |
| Yancovitz et al., 2009 (USA)19 | Female (52 years) | 46 years | Left arm | Indurated plaque of 15 cm and erythematous papules on its surface. | Yes | Yes | Negative | Pruritus | Dermis, erector pili muscle |
| Monteagudo et al., 2010 (Spain)17 | Male (32 years) | 26 years | Back and right shoulder | Macular neoformation with dark brown punctiform spots and a 2 cm plaque at one end of the lesion | Yes | Yes | Positive | Asymptomatic | Dermis, erector pili muscle. Two components:
lentiginous melanocytic hyperplasia and smooth muscle bundles |
| Toeima et al., 2010 (England)24 | Female (55 years) | NR | Vulva | Lichenification | No | No | NR | Vaginal xerosis | Dermis, dartos labialis muscle |
| Matsuda et al., 2011 (Japan)20 | Male (22 years) | 16 years | Upper right arm | Dark brown, indurated plaque 8x10 cm with follicular papules on its surface | Yes | No | NR | Pruritus, Meyerson’s phenomenon (eczematization) | Dermis, erector pili muscle |
| Adulkar et al., 2014 (India)18 | Male (32 years) | 6 months | Back (left side) | Plaque with multiple hyperpigmented follicular papules | NR | Yes | NR | Asymptomatic | Dermis, erector pili muscle |
| Chen et al., 2015 (Taiwan)28 | Male (58 years) | 10 years | Scrotum | A large mass of 30 cm composed of multiple skin-colored, firm papular, and nodular neoformations | No | No | NR | Gait disturbances, erectile dysfunction | NR |
| Bogetti et al., 2016 (Italy)29 | Male (70 years) | 1 year | Scrotum | A large mass of 20 x 32 cm, with multiple papular neoformations on its surface erythema and ulceration | NR | NR | NR | Inability to stand upright | Dermis, dartos muscle |
| Desai et al., 2017 (India)21 | Female (28 years) | 8 months | Right mid-heel | Erythematous plaque | No | No | Negative | Asymptomatic | Dermis and hypodermis, erector pili muscle |
| Jain et al., 2018 (India)10 | Male (25 years) | 6 years | Scalp skin | Multiple indurated, hyperpigmented, poorly defined plaques. The most extensive, measuring 4.5 x 6 cm. Wrinkled skin appearance | Yes | No | Negative | Asymptomatic | Dermis, erector pili muscle |
| Ladha and Remington, 2019 (Canada)22 | Female (29 years) | 6 years | Left leg | A 7 cm plaque, circular sclera, firm, with a conglomerate of skin-colored papules, warty appearance, with perilesional hyperpigmentation | Yes | No | Negative | Pain and hyperhidrosis | Dermis, erector pili muscle |
| Chen et al., 2019 (Taiwan)30 | Male (41 years) | 1 year | Penis (dorsal side) | Erythematous indurated plaque | No | No | Positive | Pruritus | Dermis, dartos muscle |
NR: not reported.
ASMH also presents clinically as plaques with hyperpigmentation and a variable degree of hypertrichosis, as well as small papules on the surface. However, very heterogeneous morphologies have been described, ranging from nodular lesions to large neoformations, forming masses up to 30 cm in size9,10. The topographies reported are the scalp10, face11, neck12,13, trunk9,14-18, upper extremities5,19,20, lower extremities3,21,22, vulva23,24, and penoscrotal area4,25-30. The present case is the second case of facial localization reported worldwide. De Alba et al. (2001) reported the first case of ASMH located on the face of an 18-year-old male patient, with a hyperpigmented plaque with thick, short, and abundant hair, with perifollicular hemispherical lesions affecting the right cheek. Histologically, the deep dermis showed numerous smooth muscle bundles and hair follicles in different evolutionary stages11.
ASMH is usually asymptomatic, although some patients present with pruritus, pain, or paresthesia3,23. A case with hyperhidrosis in the lesion was recently reported22. The acquired variant usually shows a negative pseudo-Darier sign10. On histopathology, long bundles of smooth muscle cells are randomly arranged at different dermis levels, and muscle cells have a central cigar-shaped nucleus23. Smooth muscle bundles are positive in Masson’s trichrome stain. By immunohistochemistry, alpha-actin and desmin positivity confirm the muscular histologic origin14. The age of presentation of the reported cases varies, ranging from 18 to 70 years, with no gender predominance.
Regarding the differential diagnosis of smooth muscle hamartoma, dermatologists should consider leiomyomas, angioleiomyomas, Becker’s nevus, and connective tissue nevi.
Leiomyomas are single or multiple neoformations of papular appearance, smooth, red, brown, or skin-colored. They adhere to the skin but not to deeper tissues and are painful to palpation. They predominate on the extensor surfaces of the extremities, followed by the trunk, head, and neck. On histology, they contain tightly intertwined and poorly demarcated smooth muscle bundles.
Angioleiomyomas are single neoformations of papular or nodular appearance. These lesions are red or brown, well-demarcated, slow-growing, and painful on palpation. They mainly affect the lower extremities and, less frequently, the upper extremities. Angioleiomyomas contain thick-walled blood vessels with smooth muscle fibers arranged in concentric layers.
Becker’s nevi are mixed-shape, light brown, hyperpigmented spots with fine hair on the surface. The presentation of these lesions can be multiple and bilateral, sometimes with no hypertrichosis. They are located on the face, shoulders, and anterior chest. Clinically and histologically, Becker’s nevus is the most similar entity to smooth muscle hamartoma. It has an increased number of large, deeply seated hair follicles that are sometimes associated with hyperplastic dermal smooth muscle. Due to the overlapping histologic features, some authors consider Becker’s nevus and smooth muscle hamartoma to be polar conditions at either end of a spectrum3,9,15,31. ASMH has been associated with other neoformations such as melanocytic nevi16 or nevus spilus17.
Another diagnosis to consider is connective tissue nevi. These neoformations can be congenital or acquired, single or multiple. Clinically, their appearance is papular or nodular, yellowish or skin-colored with a mamelon-shaped surface. The collagenous forms of these nevi are characterized by thickened collagen bundles in the reticular dermis, whereas elastic tissue nevi show thickened elastic fibers in the reticular dermis32.
Given the benign nature of ASMH, treatment is unnecessary; however, it can be surgically removed for cosmetic reasons, or lasers can be used to remove excess hair1 and reduce epidermal pigmentation. Some patients improve with a combination of several types of laser [pulsed light, Nd: YAG (neodymium-doped yttrium aluminum garnet), alexandrite, diode, among others] used similarly to how they are used for Becker’s nevus. Wavelengths range from 504 nm to 10,600 nm33.
The case reported here is considered atypical because of the clinical manifestations and histology. The patient showed numerous smooth muscle bundles arranged randomly, with an orientation unrelated to hair follicles and interspersed with abundant sebaceous glands throughout the thickness of the dermis. The patient also showed a significant number of hair follicles in different stages of evolution.
According to the literature, acquired smooth muscle hamartoma is derived from and constituted by smooth muscle, whereas folliculosebaceous cystic hamartoma presents cystic structures characterized by aberrant proliferation of hair follicles, sebaceous glands, and blood vessels surrounded by fibrous septa and a large number of sebocytes scattered throughout the thickness of the dermis34.
Clinically, both hamartomas present similar findings, such as nodular and xanthochromic plaque-like lesions and other pigmentations. In this regard, two cases reported were found, one as a multiple-plaque smooth muscle hamartoma10 and the other reported as the first case of folliculosebaceous cystic hamartoma with smooth muscle component35. In both cases, many smooth muscle bundles with numerous sebaceous glands of various sizes were identified on histopathologic imaging. Therefore, the patient presented here could be an intermediate form of hamartoma within a spectrum in which, at one end, there is a pure smooth muscle hamartoma and, at the other, a folliculosebaceous cystic hamartoma.
We propose to name this variant smooth muscle hamartoma with a sebaceous component, which has not been previously described to the best of our knowledge.
The present case is unusual because it is a case of an acquired smooth muscle hamartoma with a unique topography, such as the face, and mixed histopathologic findings. This article emphasizes the clinical and histopathological variability associated with both acquired smooth muscle hamartoma and folliculosebaceous cystic hamartoma.











 text new page (beta)
text new page (beta)


