Introduction
The pandemic from SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) began in Wuhan, the Republic of China. The first case was reported in December 2019, manifested with pneumonia, and was initially associated with activities in the Wuhan Huanan Seafood Wholesale Market1. It was recognized as a pandemic by the World Health Organization (WHO) on March 11, 2020, and 118,000 deaths from this virus were reported in 114 countries2.
In Mexico, the first case of COVID-19 (coronavirus disease 2019) was confirmed on February 27, 2020. As of March 26, non-essential activities were suspended, excluding those related to security, health, energy, and cleaning services. This measure was accompanied by requesting companies and agencies in the country to stop work involving mobilizing their employees from their homes to the corresponding work center3,4. The Hospital Infantil de México Federico Gómez (HIMFG), a tertiary pediatric hospital, closed its outpatient care, except for hematology-oncology, nephrology, and the immunodeficiency clinic (CLINDI, for its Spanish acronym). As of March 28, 2020, on-call care began in different areas.
In the context of the health contingency due to SARS-CoV-2 in 2020, maintaining blood component reserves has represented a significant challenge for all countries of the world5-7. Mexico has been no exception, as the flow of donors to blood banks has decreased, according to information from the National Center for Blood Transfusion (CNTS, for its Spanish acronym)8.
In Mexico, the flow of donors in blood banks decreased during the COVID-19 pandemic. According to monthly reports sent by the country’s blood banks to CNTS, a 63% decrease in donors was registered in April 2020 compared to the same month in 2019. In May 2020, 85% fewer donors were reported compared to May 2019. The Ministry of Health, through the CNTS, has guaranteed the supply of safe blood components to the entire National Blood Network, following the Strategy for safe blood supply during the COVID-19 pandemic (Estrategia para el abastecimiento de sangre segura durante la pandemia de COVID-19). This means that, even with the decrease in blood donors and the supply of blood components, Mexico has guaranteed the fulfillment of the demand for blood transfusion, which has allowed, so far, access to transfusion in all hospitals in the country8. Despite this, HIMFG sought strategies to recover donors and maintain self-sufficiency in the supply of blood components.
Some of the strategies used globally to ensure blood component supply included deferring elective procedures, limiting routine transfusions, daily auditing of transfusion requests, maintaining a blood component reserve of at least two weeks, communicating with altruistic donors to encourage donation, use of external mobile blood donation centers, and changes in donation requirements, as well as changes in mass transfusion protocols9-13.
Although the above strategies have been implemented, the effect of each on donor flow has not been determined. Therefore, this study aimed to describe the strategy used at HIMFG for donor recruitment and assess its impact on recruiting altruistic and family donors.
Methods
We conducted an analytical, longitudinal, prospective, and quasi-experimental study to analyze the effect of various blood component donor recruitment strategies during 2020. Data on the number of donors, blood components, and rejections were collected routinely and prospectively by the blood bank.
Strategies were added as the need to increase the number of donors arose. Some aimed to attract altruistic donors, while others sought to attract family donors. An altruistic donor is a person who provides blood or blood components for the therapeutic use of anyone who requires it, with no intention of benefiting a particular person, motivated solely by humanitarian feelings and solidarity, without expecting any compensation in return, and without a specific request from healthcare personnel, family or friends of the patients14,15. A family or replacement donor refers to a person who provides blood or blood components to a patient in response to a specific request from healthcare personnel, family members, or friends of patients14,15.
Data from the 2019 HIMFG blood bank were compared with those from 2020, specifically in the months in which donor recruitment strategies were used, dividing the strategies into those focused on altruistic and family donation. Data from all accepted donors were considered.
Strategies implemented
Strategies were applied to recruit donors and ensure the self-sufficiency of blood components at the HIMFG (Table 1).
Table 1 Blood component donor recruitment strategies
| Strategy | Description | Implementation period | Type of donor to whom it is directed |
|---|---|---|---|
| Awareness raising and promotion of blood donation | Awareness-raising talks and promotion of blood component donation were given to patients’ families in the hematology-oncology service | March to October 2020 | Family members |
| Updated criteria on the number of donors required for each procedure | Patients undergoing procedures or attending certain services are asked for blood donors as a preventive measure in case they need blood components. There is a ratio of the number of donors requested according to the procedure; this ratio changed after the onset of the pandemic, with more donors requested so that the blood bank would remain self-sufficient | October to December 2020 | Family members |
| Locating recurrent altruistic donors | Altruistic donors were located with the help of the internal operating system "Blood Bank Diagnostic System" to request their support for blood donations | March to June 2020 | Altruists |
| Campaign for HIMFG employees | HIMFG employees were invited by mail to donate blood components. Posters were also placed in the facilities with the same invitation | April to May 2020 | Altruists |
| Partnership with the association Blooders | A partnership was signed with the Blooders association to be part of its digital platform for programming and recruiting altruistic blood donors | May to December 2020 | Altruists |
HIMFG: Hospital Infantil de México Federico Gómez.
Awareness raising and promotion of blood donation
Informative and awareness-raising talks were given at the hematology-oncology and short-stay chemotherapy outpatient clinic, where bone marrow aspiration and lumbar puncture procedures have been performed on an outpatient basis since March 2020. As many of these patients only come for one procedure and are sometimes transfused before the procedure is completed, the number of transfusions performed and the number of donors requested when the patient is hospitalized increase. In each of the presentations and educational sessions, information was provided on the requirements and need for blood donation in times of pandemic, inviting and encouraging more active participation. Data for the talks was obtained from the Technical Guide of the Blood Bank and Transfusion Medicine Service (Guía técnica del servicio de banco de sangre y medicina transfusional)16, which is an official HIMFG document (reference code HIM-LC-MT-PR.15-DE.01). This document contains a script of what to say to family members, which includes topics such as the following:
– Handling of personal data at the Blood Bank
– Process, screening, and evaluations before donation
– Types of blood component donation
– Average duration of the different donation processes
– Foods and beverages that can be consumed during the donation process
– Promotion of altruistic donation
– Hemovigilance
– Myths and benefits of blood donation
– Self-exclusion form
– Care and recommendations after donation.
Updated criteria for requesting blood donors per patient according to procedure
On October 20, 2020, the number of blood donors requested from patients based on the condition or procedure to undergo was updated (Table 2).
Table 2 Donors requested according to their condition or procedure
| Condition or procedure | Donors required |
|---|---|
| Hospitalization | Two |
| Minor surgery or endoscopic procedures | Two |
| Plastic surgery (cranial advancement) | Five |
| Orthopedic major surgery | Five |
| Bone marrow transplant | Five for blood and five for apheresis |
| Liver transplant | Ten |
| Kidney transplant | Five |
| Extracorporeal circulation pump surgery | Eight |
| Nasopharyngeal angiofibroma | Fifteen |
| Neurosurgery | Five |
| Liver biopsy | Two for apheresis |
Any patient who had met the minimum donation requirements and, having been transfused, required a larger quantity of blood components had to complete the missing blood units.
Locating repeat altruistic donors
Tracking and locating eligible repeat altruistic donors by telephone was performed with the help of the blood bank’s internal system. Appointments were scheduled for eligible donors of different blood groups between March and December 2020.
Campaign for HIMFG employees
An altruistic blood donation campaign was conducted for HIMFG personnel in April and May 2020. The campaign was publicized with the support of social networks, the union section 84, and the Institute’s commuter. Images of the campaign can be found in Annex 1.
Collaboration with the Blooders association
In May 2020, HIMFG formed a link with the association Blooders to be part of their digital platform for registration and scheduling blood donation appointments. On this platform, donors can choose our institution for donation, and they can schedule an appointment. Blood bank social work was in charge of confirming the appointment, reviewing the donation status, and following up with donors for subsequent donations.
It should be noted that all donors were asked to strictly wear valve-less N-95 or tri-layer masks, as recommended by the Ministry of Health and CNTS. In addition, alcohol gel was constantly provided. Donors were seated in the waiting room, maintaining a safe distance during the blood donation process.
Donors had at their disposal the Integral Privacy Notice of the Blood Bank and Transfusion Medicine Service (Aviso de Privacidad Integral del Servicio de Banco de Sangre y Medicina Transfusional)17.
Statistical analysis
SPSS version 21 was used for statistical analysis. For the baseline characteristics of the eligible donors, frequencies and percentages were used for qualitative variables, and median and interquartile ranges for quantitative variables.
The number and percentage of altruistic and family donors in the months of 2020 in which the strategies were applied were compared with the same months of 2019 using the χ2 test.
Spearman’s test calculated the correlation between the number of altruistic donor recruitment strategies and the percentage of altruistic donors.
Results
Donations
In 2019-2020, 17,003 donors were registered; mean monthly donations were 706.42 (standard deviation (SD) 34.42). Since the beginning of the pandemic, no COVID-19 infection was recorded in donors during the study. The total number of donors in 2020 (6,747) decreased from 2019 (9,787). Of these donors, 7,274 (74.2%) in 2019 and 5,071 (75.16%) in 2020 were accepted.
The requirement for blood components decreased, as 10,037 units were transfused in 2019 and 8,619 in 2020, thus maintaining self-sufficiency in donations. It is worth mentioning that the components obtained from donors can be fractionated into different blood components.
Regarding the characteristics of eligible donors, they mainly remained the same in 2019 and 2020 (Table 3). Throughout the study, most donors were males between 26 and 42 years of age who had completed high school. Consistent with the prevalence of blood types worldwide, the most frequent blood type was O+.
Table 3 Baseline characteristics of eligible donors
| Total (n = 12,385) | 2019 (n = 7,315) | 2020 (n = 5,070) | p-value* | |
|---|---|---|---|---|
| Female, n (%) | 4,728 (38.18) | 2,765 (37.80) | 1,963 (38.72) | 0.300 |
| Age, median (IQR) | 33 (26-42) | 34 (26-42) | 33 (26-41) | 0.002** |
| Schooling, n (%) | ||||
| – Illiterate | 65 (0.52) | 40 (0.55) | 25 (0.49) | 0.684 |
| – Reads and writes | 132 (1.07) | 76 (1.04) | 56 (1.10) | 0.727 |
| – Primary school | 1,173 (9.47) | 731 (9.99) | 442 (8.72) | 0.015 |
| – Junior High school | 4,016 (32.43) | 2,434 (33.27) | 1,582 (31.20) | 0.015 |
| – High school | 3,633 (29.33) | 2,107 (28.80) | 1,526 (30.10) | 0.119 |
| – Technical career | 350 (2.83) | 211 (2.88) | 139 (2.74) | 0.637 |
| – Bachelor’s degree | 2,838 (22.91) | 1,626 (22.23) | 1,212 (23.91) | 0.029 |
| – No data | 178 (1.44) | 90 (1.23) | 88 (1.74) | 0.0201 |
| Blood type, n (%) | ||||
| – O+ | 8,765 (70.77) | 5,218 (71.33) | 3,547 (69.96) | 0.099 |
| – A+ | 2,368 (19.12) | 1,375 (18.80) | 993 (19.59) | 0.272 |
| – B+ | 831 (6.71) | 490 (6.70) | 341 (6.73) | 0.950 |
| – AB+ | 107 (0.86) | 60 (0.82) | 47 (0.93) | 0.528 |
| – O- | 211 (1.70) | 110 (1.50) | 101 (1.99) | 0.039 |
| – A- | 71 (0.57) | 46 (0.63) | 25 (0.49) | 0.235 |
| – B- | 15 (0.12) | 9 (0.12) | 6 (0.12) | 0.944 |
| – AB- | 1 (0.01) | 1 (0.01) | 0 (0) | 0.854 (Yates) |
| Collection, n (%) | ||||
| – Whole blood | 9,839 (79.44) | 5,889 (80.51) | 3,950 (77.91) | 0.0004 |
| – Apheresis | 2,546 (20.56) | 1,426 (19.49) | 1,120 (22.09) |
*χ2-test;
**Mann-Whitney U test.
IQR: interquartile range.
In 2019, the rejection rate was 25%, while in 2020, it was 29.6%. Approximately 75% of the rejections in both years were due to medical causes (Table 4). The other rejection causes were illicit substance use, acupuncture, and breastfeeding. While the first two causes of rejection remained the same in 2019 and 2020, in 2020, the third cause of rejection was the common cold, while in 2019, it was leukocytosis.
Table 4 Causes of medical rejection
| Variables | Total (n = 4,618) n (%) | 2019 (n = 2,482) n (%) | 2020 (n = 2,136) n (%) | p-value* |
|---|---|---|---|---|
| Risky sexual practices | 878 (19.0) | 504 (20.3) | 374 (17.5) | 0.016 |
| Low hemoglobin | 643 (13.9) | 381 (15.4) | 262 (12.3) | 0.003 |
| Leukocytosis | 235 (5.1) | 128 (5.2) | 107 (5.0) | 0.820 |
| High hemoglobin | 218 (4.7) | 145 (5.8) | 73 (3.4) | 0.0001 |
| Common cold | 210 (4.5) | 57 (2.3) | 153 (7.2) | < 0.0001 |
| Lipemia | 184 (4.0) | 85 (3.4) | 99 (4.6) | 0.036 |
| Caries 4 G | 172 (3.7) | 90 (3.6) | 82 (3.8) | 0.703 |
| Low weight | 168 (3.6) | 101 (4.1) | 67 (3.1) | 0.091 |
| Thrombocytopenia | 150 (3.2) | 69 (2.8) | 81 (3.8) | 0.053 |
| Hypertension | 122 (2.6) | 61 (2.5) | 61 (2.9) | 0.400 |
| Leukopenia | 116 (2.5) | 38 (1.5) | 78 (3.7) | < 0.0001 |
| Tattoos | 103 (2.2) | 60 (2.4) | 43 (2.0) | 0.353 |
| Vaccinations | 82 (1.8) | 34 (1.4) | 48 (2.2) | 0.024 |
| Perforations | 76 (1.6) | 43 (1.7) | 33 (1.5) | 0.618 |
| Medications | 71 (1.5) | 29 (1.2) | 42 (2.0) | 0.028 |
| Difficulty accessing vein | 51 (1.1) | 41 (1.7) | 10 (0.5) | 0.0001 |
*χ2-test.
Altruistic donations
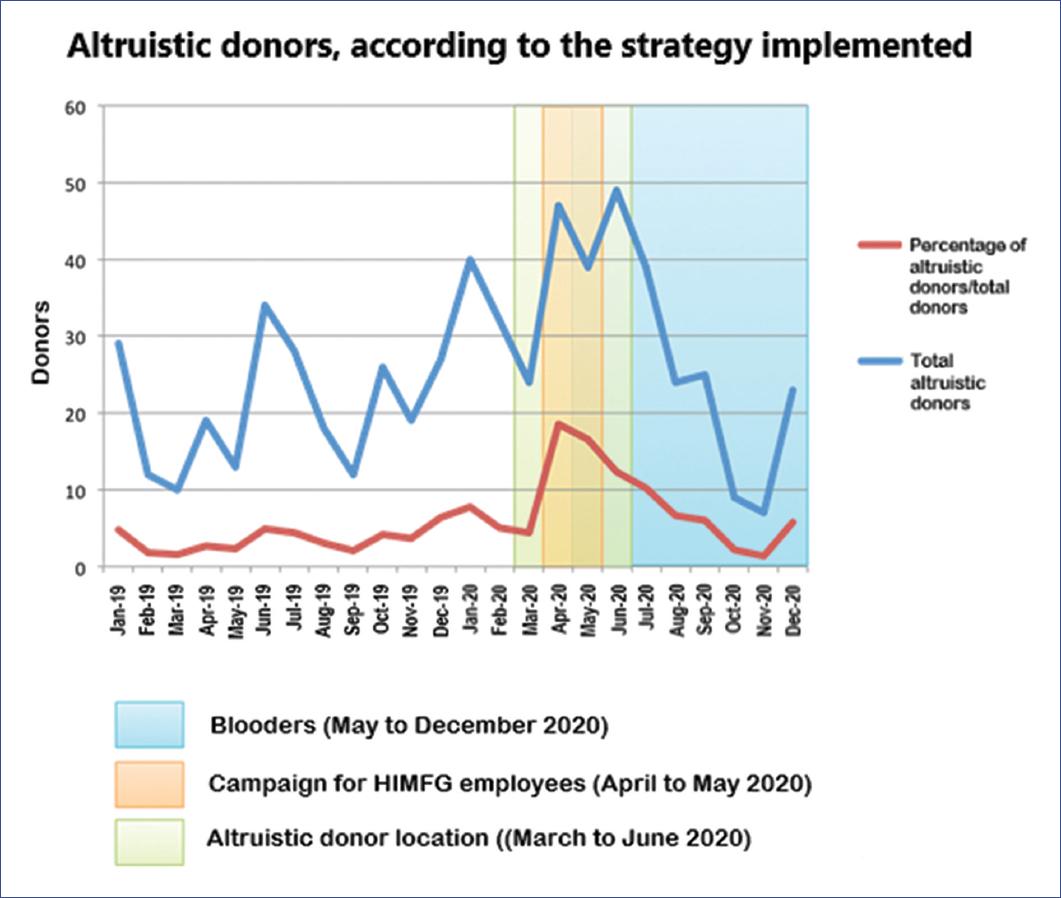
Altruistic donors increased in 2020 compared to 2019. A total of 604 altruistic donors were registered during the study: 246 in 2019 and 358 in 2020. The mean number of altruistic donors per month increased from 20.58 (SD 8.00) in 2019 to 29.83 (SD 13.59) in 2020 (p = 0.05). Of the total number of donors, 3.65% were altruistic. Similarly, this figure increased in 2020 compared to 2019: 2.5% altruistic donors in 2019 and 5.3% altruistic donors in 2020 (p < 0.001).
Impact of strategies on altruistic donors
The strategies associated with an increase in the percentage of altruistic donors were Locating altruistic donors alone, as well as the combination of two or more strategies aimed at obtaining altruistic donors. The collaboration with the Blooders association had no significant impact per se (Table 5).
Table 5 Percentage of altruistic donors during the interventions directed to this population
| Number of interventions | Interventions | 2019 n (%) | 2020 n (%) | p-value |
|---|---|---|---|---|
| 1 | Location of altruistic donors1 | 657 10 (1.52) | 550 25 (4.36) | 0.0030 |
| 2 | Location of altruistic donors+Donation campaign directed to HIMFG staff2 | 707 19 (2.69) | 254 47 (18.50) | < 0.0001 |
| 3 | Localization of altruistic donors + Donation campaign directed to HIMFG staff + BLOODERS3 | 554 13 (2.35) | 235 39 (16.60) | < 0.0001 |
| 2 | Localization of altruistic donors + BLOODERS4 | 1340 62 (4.63) | 781 88 (11.27) | < 0.0001 |
| 1 | BLOODERS5 | 2739 102 (3.72) | 2099 88 (4.19) | 0.4058 |
The months during which the intervention was carried out in 2020 were compared against the same months in 2019.
1March 2019 vs. March 2020;
2April 2019 vs. April 2020;
3May 2019 vs. May 2020;
4June-July vs. June-July 2020;
5August-December 2019 vs. August-December 2020.
HIMFG: Hospital Infantil de México Federico Gómez.
The percentage of altruistic donors was higher when the three strategies were applied simultaneously (Figure 1).
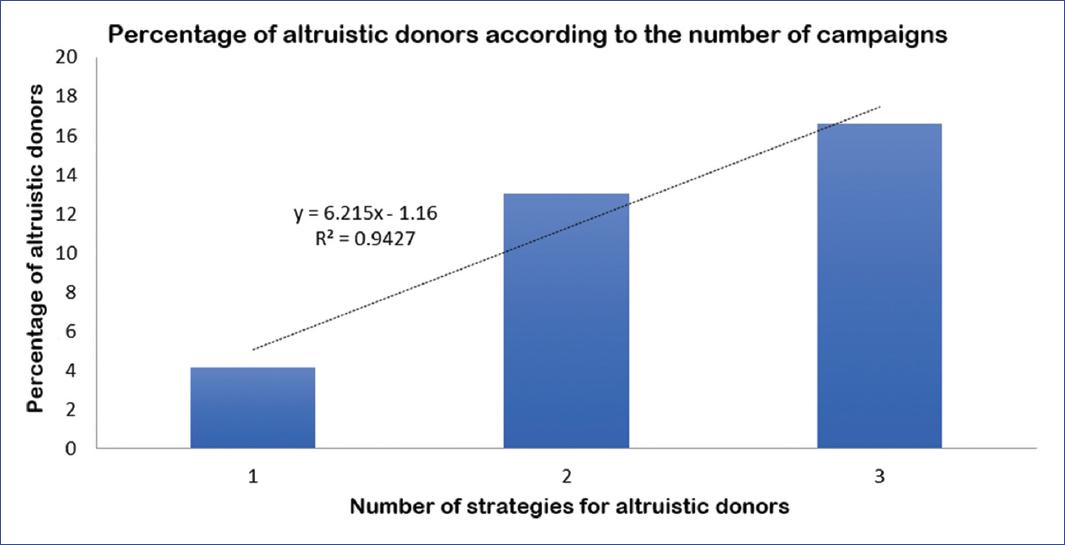
A positive correlation was found between the number of strategies and the percentage of altruistic donors (rho = 0.846, p = 0.002). In addition, a tendency for donors to increase with the number of strategies applied simultaneously was detected (Figure 2).
Also, the results showed a decrease in blood donor refusal in 2020 compared to the previous year. In 2019, the percentage of rejection was 24.9% (mean 203.67, SD 31.84), while in 2020 it was 22.01% (mean 123.75, SD 84.97) (p = 0.005). Table 3 shows the number of donors rejected with and without each strategy applied.
Impact of strategies on family donors
No statistically significant differences were observed when comparing the months in which the strategies aimed at obtaining family donors were applied in 2019 compared with the same months in 2020. The only significant difference was found with the strategy Awareness and promotion in hematology and oncology. However, more family donors were identified in 2019 than 2020 when comparing the same months in which the strategy was applied (Table 6).
Table 6 Percentage of family donors during interventions directed to this population
| Number of interventions | Interventions | 2019 No intervention n (%) | 2020 Intervention n (%) | p-value |
|---|---|---|---|---|
| 1 | Awareness raising and promotion in hematology and oncology1 | 4431 4297 (96.98) |
2600 2353 (90.50) |
< 0.0001 |
| 2 | Awareness raising and promotion in hematology and oncology + Update of criteria for the number of donors2 | 630 604 (95.87) |
406 397 (97.78) |
0.0966 |
| 1 | Update of criteria for the number of donors3 | 936 890 (95.09) |
913 883 (96.71) |
0.0778 |
The months during which the intervention was carried out in 2020 were compared against the same months in 2019.
1March-September 2019 vs. March-September 2020;
2October 2019 vs. October 2020;
3November-December 2019 vs. November-December 2020.
Discussion
The COVID-19 pandemic significantly decreased the flow of blood donors worldwide5-7; the same occurred in the HIMFG blood bank. Although the strategies implemented throughout 2020 to attract donors failed to increase their number, they did manage to increase the percentage of altruistic donors. However, it is impossible to know whether they came willingly or because of any strategies to attract them. Fear of contagion was, however, known to be a factor present at the beginning of the pandemic that caused donors to limit their attendance at the blood banks12. Regardless, this study demonstrates that strategies to attract altruistic donors had a positive outcome: the more simultaneous strategies were applied, the higher the percentage of altruistic donors.
Another factor that may have influenced the flow of altruistic donors to the bank was pandemic activity. According to data from the National Council of Science and Technology (CONACYT, for its Spanish acronym), in 2020, the highest infection peaks were recorded during July and December18. In July 2020, two strategies to attract altruistic donors were active at HIMFG. When comparing the percentage of donors between July 2019 and July 2020, we found an increase in July 2020 (4.1% to 10.2%; p < 0.0001). Despite being under a wave of contagion, donors came to help, which may have resulted from the strategies implemented. This was not the case during December, as the percentage of altruistic donors in December 2019 and December 2020 did not differ. It should be noted that, during this month, only the Blooders association linkage strategy was active, which did not show any effect on the increase in altruistic donors.
Strategies focused on family donor recruitment were not entirely successful, as the percentage of family donors was maintained; however, this may be related to several factors. As part of the Strategy for the safe blood supply during the COVID-19 pandemic implemented by the CNTS8, donor selection and deferral criteria were updated from the onset of the pandemic to avoid COVID-19 transmission. The deferral of elective procedures could have influenced the decrease in the demand for blood components since the beginning of the pandemic, which would explain the reduction of family donors.
Although the various strategies used to maintain self-sufficiency in blood banks have been reported worldwide9-13, we have not found studies that report either the impact or the increase in altruistic donors when implementing simultaneous strategies. The strategies implemented worked in a tertiary pediatric hospital during the COVID-19 pandemic. However, it is essential to mention that these interventions can be extrapolated for future studies. Awareness talks can be given, with the same topics, in other hospitals or institutes. Depending on the procedures or surgeries, the donation criteria requested may vary according to the type of patients; however, they can also be applied. Locating frequent altruistic donors depends on the records of each blood bank; if a registry exists, reminders can be created to maintain contact with them. If not, it can be made for this purpose. In any work environment, employees can be invited to become donors with information sheets (Annex 1). Finally, organizations such as Blooders serve as a link between altruistic donors and blood banks.
Among the limitations of this study is that being a real-time study, it was impossible to isolate the impact of each strategy since several were applied simultaneously. However, more strategies exponentially affected the number of altruistic donors.
Another limitation was that the scope of the strategies was not quantified. Measuring the direct and indirect impact of each strategy (communication from one person to another, the visual impact of posters, among others) is highly complicated in a hospital, during and outside the context of a pandemic; it is also difficult to measure the persistence of their effect.
Each of the strategies aims to attract donors, but the intention is that they become recurrent donors. A limitation of the study is that there is no way of knowing whether successfully recruited donors donated once or more times during the study, nor whether they continued to do so afterward. Therefore, studies aimed at measuring outreach and continuity are needed.
Finally, the cost of each strategy was not calculated. Although the exact cost of calls, mailings, brochures, posters, and other materials used was not calculated, we consider that the strategies implemented are not costly since most of them depend on the goodwill of those involved.
In conclusion, we can state that altruistic donors are vital in a health emergency to achieving blood bank self-sufficiency. Their participation is of utmost importance since, thanks to them, it is possible to provide adequate care to patients requiring hematological components for their medical treatment.
This study demonstrates that applying simple strategies to recover altruistic donors effectively maintains blood bank self-sufficiency in a pediatric hospital, even in a pandemic. Furthermore, the results suggest the importance of encouraging the implementation of similar strategies in different blood banks in this context.











 text new page (beta)
text new page (beta)