Introduction
Leukemia is a neoplasm of the bone marrow and blood that is the primary malignant pathology in childhood. Acute leukemias are rapidly progressive diseases that affect immature hematopoietic cells, preventing them from functioning normally. The term acute myeloid leukemia (AML) encompasses a heterogeneous group of leukemias originating from myeloid, erythroid, and megakaryocytic precursors, and monocytic cell lineages. These leukemias are produced by clonal transformation of hematopoietic precursors by chromosomal rearrangements and multiple genetic mutations1. The classification and diagnosis of AML are based on morphological, cytochemical, cytogenetic, fluorescence in situ hybridization, immunophenotyping with flow cytometry, and molecular testing1. Therefore, the FAB (French-American-British Cooperative Group) classified AML into subtypes (M0-M7).
The clinical presentation of AML includes signs and symptoms caused by leukemic infiltration of the bone marrow and extramedullary sites such as the skin. Specific and nonspecific lesions can manifest cutaneous involvement during leukemia. Leukemides or nonspecific skin lesions are those lesions that do not contain tumor cells and may originate from abnormal hematopoiesis causing pancytopenia in the bone marrow. Their symptoms are bleeding, skin pallor, and susceptibility to infections; they are usually secondary to adverse drug reactions and paraneoplastic syndromes2. A low percentage of patients develop leukemia cutis (LC) or cutaneous leukemia, which is defined as cutaneous infiltration of neoplastic leukocytes (of myeloid or lymphoid lineage) resulting in skin lesions3,4. Cases that develop during the neonatal period are classified as congenital LC5. In some patients, cutaneous involvement is the only manifestation of leukemia, known as aleukemic leukemia cutis. Furthermore, this variety may precede leukemia in blood or bone marrow by months or years4,5.
Although acute lymphoblastic leukemia (ALL) is the most frequent leukemia in the pediatric population, LC appears more frequently in AML, mainly in the subtypes with a monocytic component6. So far, only a few studies of LC in the different varieties of leukemia have focused on the pediatric population, and the existing ones are case reports or studies with small sample size.
Methods
A retrospective cross-sectional study was conducted at the Hospital Infantil de México Federico Gómez from January 2009 to December 2019 to determine the clinical and demographic characteristics of AML patients with LC and other mucocutaneous manifestations.
All patients diagnosed with AML confirmed by bone marrow aspirate who attended the hospital during the referred study period and were younger than 18 years of age were included. Patients whose clinical records were not available or whose information was incomplete were excluded.
The medical information of AML diagnosed patients was obtained by reviewing the clinical records in the general archive of the hospital. Each patient's demographic and clinical data were collected, and the information obtained was captured in the statistical program SPSS version 17. Demographic information was collected from the initial clinical record. Clinical information (mucocutaneous manifestations) was obtained from the descriptions recorded in the clinical history, evolution, follow-up, and specialized assessment notes. Information was taken from the confirmation of the AML diagnosis until the evolution note of the patient's last visit to the hospital.
This study did not present any risk, since no intervention was performed; only medical record information was analyzed, preserving patient confidentiality.
Results
We identified 90 records of patients with a diagnosis of AML. From these records, 22 were excluded because they did not correspond to the diagnosis and were not available for review, and 14 were eliminated because they did not contain complete information.
We reviewed 54 files of patients with a diagnosis of AML who attended the hospital from 2009 to 2019, of which 29 (53.7%) were males and 25 (46.3%) females. The age of the patients ranged from 3 months to 18 years, with an average of 6 years 8 months. The cases studied came from ten states of the country: 23 cases (42.6%) from the State of Mexico, 21 (38.9%) from Mexico City, two cases (3.8%) from Guerrero, two cases (3.8%) from Veracruz and Tamaulipas, and one case per state from San Luis Potosí, Querétaro, Oaxaca, Jalisco, and Chiapas (1.8% for each case).
Of the total number of patients, 51 (94.5%) received chemotherapy. Three (5.5%) patients did not receive chemotherapy due to voluntary discharge or having medical insurance that allowed referral to another institution.
A skin lesion or dermatosis during the disease was present in 75.9% (41) of the patients, compared with 24.1% who showed no skin involvement. Thirteen patients presented two or more dermatoses during the disease, from which two cases were in the group with LC. The most frequent skin lesions were nonspecific; infectious conditions predominated, followed by dermatoses related to chemotherapy (Table 1). LC was present in 14.8% (8) of the patients, and two cases corresponded to congenital LC. The clinical and demographic characteristics of the patients with LC are shown in Table 2 (Figures 1-5). Table 3 shows the comparison between patients with and without skin infiltration.
Table 1 Dermatoses present in patients with leukemia cutis at the Hospital Infantil de México Federico Gómez
| Dermatological manifestation | Cases | Number of cases | Percentage (%) | Clinical manifestations |
|---|---|---|---|---|
| Leukemia cutis | 8 | 6 | 75 | Leukemia cutis |
| 2 | 25 | Congenital leukemia cutis | ||
| Paraneoplastic dermatoses | 10 | 7 | 7 | Disseminated intravascular coagulation |
| 1 | 10 | Chronic ulcer | ||
| 1 | 10 | Paraneoplastic itch | ||
| 1 | 10 | Erythema nodosum | ||
| Chemotherapy-associated dermatoses | 19 | 16 | 84.5 | Alopecia or stomatitis/mucositis |
| 1 | 0.5 | Erythema multiforme | ||
| 1 | 0.5 | Anaphylaxis | ||
| 1 | 0.5 | Diffuse hyperpigmentation | ||
| Infectious dermatoses | 29 | 12 | 41 | Cellulitis |
| 7 | 24 | Cutaneous abscesses | ||
| 5 | 17 | Chickenpox/shingles | ||
| 1 | 0.3 | Folliculitis | ||
| 1 | 0.3 | Staphylococcal scalded skin | ||
| 1 | 0.3 | Ecthyma gangrenosum | ||
| 1 | 0.3 | Herpes simplex | ||
| 1 | 0.3 | Verruca vulgaris |
Table 2 Clinical and demographic characteristics of patients with leukemia cutis at the Hospital Infantil de México Federico Gómez
| Case | Sex | Age | Birthplace | AML subtype | LC type | Clinical manifestation | Time of onset relative to the diagnosis of systemic leukemia | HP | Evolution |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 8 y | Mexico City | 2 | LC | Gingival hyperplasia Chloromas |
After | No | Monitoring |
| 2 | M | 7 y | Mexico City | 4 | LC | Infiltrated plaques | During the diagnostic assessment | No | Monitoring |
| 3 | M | 2 y | Mexico City | 7 | LC | Chloromas | During the diagnostic assessment | Yes | Monitoring |
| 4 | M | 8 m | State of Mexico | 2 | Congenital LC | Papules Infiltrated plaques | With the established diagnosis | Yes | Treatment |
| 5 | F | 5 m | Veracruz | 0 | Congenital LC | Nodules Tumors |
With the established diagnosis | Yes | Unknown |
| 6 | M | 8 y | State of Mexico | 2 | LC | Gingival hyperplasia | During the diagnostic assessment | No | Treatment |
| 7 | M | 2 y | Tamaulipas | 4 | LC | Gingival hyperplasia | With the established diagnosis | Yes | Treatment |
| 8 | M | 10 y | Guerrero | 0 | LC | Infiltrated plaques | During the diagnostic assessment | Yes | Death |
AML, acute myeloid leukemia; LC, leukemia cutis; m, months; HP, histopathology; y, years.

Figure 4 Perivascular, periannexal, and interstitial infiltrate consisting of atypical cells (hematoxylin and eosin staining).
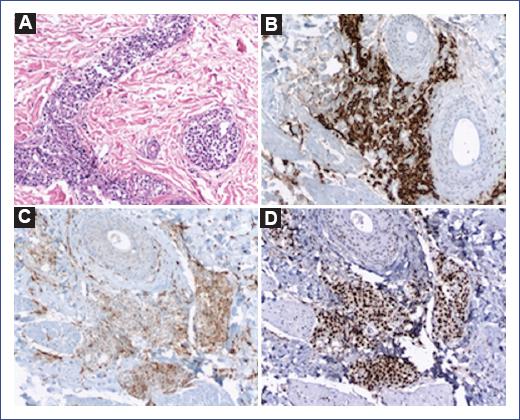
Figure 5 A: close-up of perivascular and interstitial infiltrate of atypical cells (hematoxylin and eosin staining). B: myeloperoxidase positive. C: CD68 (KP-1) positive. D: K1-67 (cell proliferation index) high.
Table 3 Characteristics of subjects with acute myeloid leukemia according to the presence of leukemia cutis
| Characteristics | Patients with LC n (%) | Patients with no LC n (%) |
|---|---|---|
| Number of patients | 8 | 46 |
| Sex | ||
| Male | 6 (75%) | 23 (50%) |
| Female | 2 (25%) | 23 (50%) |
| Age, median (range) | 4-6 m (1-4 m to 8 y) | 6 y (3-11 m to 12 y) |
| Type of AML according to FAB | ||
| M0: Minimally differentiated AML | 2 (25%) | 1 (2.2%) |
| M1: AML without maturation | 0 | 10 (21.8%) |
| M2: AML with maturation | 3 (37.5%) | 11 (24.0%) |
| M3: Acute promyelocytic leukemia | 0 | 10 (21.8%) |
| M4: Acute myelomonocytic leukemia | 2 (25%) | 8 (17.3%) |
| M5: Acute monocytic leukemia | 0 | 0 |
| M6: Acute erythroleukemia | 0 | 2 (4.3%) |
| M7: Acute megakaryoblastic leukemia | 1 (12.5%) | 4 (8.6%) |
| Evolution | ||
| Treatment | 3 (37.5%) | 16 (34.8%) |
| Monitoring | 3 (37.5%) | 15 (32.6%) |
| Death | 1 (12.5%) | 14 (30.4%) |
| Unknown | 1 (12.5%) | 1 (2.2%) |
AML, acute myeloid leukemia; FAB, French-American-British Cooperative Group; LC, leukemia cutis; m, months; y, years.
Discussion
To the extent of our knowledge, the present study is the first study in Mexico to collect cases of LC and other mucocutaneous manifestations over 10 years in all groups of pediatric patients with AML at a pediatric referral center. In this study, the most common mucocutaneous manifestations were drug reactions and infections.
There are few studies on LC in the Latino children population, and most are only case reports. Therefore, we could not compare the results with other populations with ethnic similarities with our population. When comparing our data with that from other parts of the world, only two studies of LC in patients with childhood AML were found in PubMed (Table 4)7,8. In one of these studies, the frequency of LC in children from France was found to be 5.5%7. In the adult population, an LC prevalence of 3.7-11% has been reported in patients with AML9,10. In our study, the frequency of LC was higher (14.8%) and more closely resembled data reported in adults.
Table 4 Studies on leukemia cutis in the pediatric population
| Feature | Present study (Godínez et al.) | Andriescu et al.8 | Gouache et al.7 |
|---|---|---|---|
| Country | Mexico | USA | France |
| Diagnoses of the study population | AML | AML (74.2%), ALL, CMML, JMML, MLL | AML |
| Number of LC cases | Total: 8 | Total: 31 | Total: 24 |
| Congenital LC: 2 | Congenital LC: 6 | Congenital LC: 1 | |
| Sex | F: 25% | F: 51.6% | F: 29% |
| M: 75% | M: 48.4% | M: 71% | |
| Frequency of LC | Clinical 14.8% | | Clinical 5.5% |
| Histological: 9.2% | Histological: 3.4% | ||
| Age comparison (average) | With LC: 4.7 years With no LC: 7.2 years |
With LC: 321 days | With LC: 1.2 years With no LC: 8.7 years |
| Clinical manifestations | Infiltrated plaques: 37.5%. | Nodules: 63.3% | Nodules: 67%. |
| Gingival hyperplasia: 37.5%. | Papules: 50% | Papules: 8%. | |
| Chloromas: 25%. | Papules + nodules: 8%. | ||
| Papules: 12.5%. | Infiltrated plaques: 17%. | ||
| Nodules: 12.5% | |||
| Tumors: 12.5%. | |||
| Deaths | Patients with LC: 1 (12.5%) | Patients with LC: 12 (38.7%) | Patients with LC: 53% |
| Patients with no LC: 14 (30.4%) | Patients with no LC: 23% |
ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; CMML, chronic myelomonocytic leukemia; F, female; JMML, juvenile myelomonocytic leukemia;
LC, leukemia cutis; M, male; MLL, mixed lineage leukemia or lymphoid-myeloid leukemia.
Regarding sex, LC was similar between males and females in children from the U.S.8, but in French children, LC predominated in males7. We also found that LC was more frequent in males in our study. As for age, children with AML with LC were younger than children with AML but no LC; these data are similar to those reported by Gouache et al. in a French pediatric population7. Three pediatric studies included cases of neonates with AML and leukemic skin infiltration; the reported frequency at this age was 25-30%11,12. Both American and Mexican studies confirmed this frequency.
To date, all reports in children and adults agree that the most frequent forms of clinical expression of LC are papules, nodules, and infiltrated plaques7,8,13,14. Our patients also expressed these lesions. Additionally, some of them showed gingival hyperplasia, a mucosal condition very suggestive of leukemic infiltration that appears more in the myeloid cell lineage due to the monocyte's predilection to migrate to this tissue6,13,14. The other skin condition found was chloroma, which is a nodular, dome-shaped, firm, erythematous lesion that, when incised, acquires a greenish color due to its high myeloperoxidase content6,15; an increased incidence of these lesions has been observed in children6.
All skin lesions can appear at different stages of the hematologic disease. Most frequently, they occur after hematologic diagnosis (55%), followed by coincident occurrence (38%), and more rarely (7%) before systemic infiltration13. In the pediatric population, the onset of LC usually occurs concomitantly and after systemic disease8; this behavior was also observed in our study.
Finally, LC is considered by some authors as a poor prognostic factor because it may indicate tumor relapse or recurrence8. For example, in the study published by Su et al., 88% of adult patients with LC died, most of them within one year13. In French children, the cumulative mortality incidence in patients with AML and LC was higher (53%) than patients without LC (23%)7. These data are different from what we found in our study since there was only one death in LC cases (12.5%) and mortality was higher in patients without LC (30.4%). This observation could be explained due to the sample size or follow-up of patients at the study cutoff.
It is necessary to carry out more descriptive studies worldwide in the pediatric population with AML and LC to compare these populations' clinical and demographic characteristics and validate the results. We cannot generalize the information we obtained in this pediatric population with AML to a national level since most of the patients in our study were from Mexico City. Therefore, the information obtained is representative of only one geographic region. Some of the remaining questions for this topic are whether chloromas in LC are more frequent in children and if the appearance of LC modifies the prognosis in pediatric patients. To answer these questions, we need to have a more extensive series of patients with a longer follow-up time.
Our study found that LC in patients with AML appeared in 14.8% of cases (and 9.2% with histological correlation). Of the cases with LC, the predominant gender was male, the patients were younger than those without LC, and the most frequent AML subtype was M2 (37.5%); infiltrated plaques, chloromas, and gingival hyperplasia were the most frequent clinical expressions, and the time of onset of LC was simultaneous with the diagnosis of AML (50% in the diagnostic workup, 37.5% with the diagnosis established) or after diagnosis.
AML can present with infiltration of neoplastic leukocytes to the skin, and its clinical expression is variable. Some lesions are infiltrated papules, nodules, or plaques and can be the first sign of disease or be indicative of clinical progression; their recognition will favor a timely diagnosis and treatment.











 text new page (beta)
text new page (beta)





