Introduction
Hereditary hemorrhagic telangiectasia (HHT) or Osler Weber Rendu Syndrome (OWRS) is a multiorgan disorder, of autosomal dominant inheritance, resulting in fibrovascular dysplasia with multiple arteriovenous malformations in different organs1.
Pulmonary arteriovenous malformations are the most common pulmonary findings found in patients with HHT2,3. They can be asymptomatic or may present various symptoms such as cyanosis, dyspnea, heart failure, hemoptysis, and paradoxical embolism4.
Case
A 9-year-old female presented with cyanosis, dizziness, and headache for a month. No family history for heart disease. No murmurs, peripheral cyanosis, oxygen saturation 70% and normal electrocardiogram. The echocardiogram did not report structural abnormalities but with a positive bubbles test appearing after three cardiac cycles. She was referred with a report without images of pulmonary computed tomography that reported two arteriovenous malformations in the left lower lobe.
Interventional catheterization was performed, a catheter was advanced through a venous access to the lower left lobar artery, angiography was performed to identify the pulmonary arteriovenous fistulas, four were identified (Fig. 1), it was started by the central one, an Amplatzer® Vascular Plug device II of 10 mm was advanced and delivered. This procedure was repeated, cannulating the other three malformations, which were a few millimeters from the first one; a 12, 6, and 8 mm vascular plugs were used, respectively. A final angiogram showed occlusion of all four vessels (Fig. 1). Peripheral oxygen saturation in ambient air increased from 70% to 95%. The procedure was completed without complications.
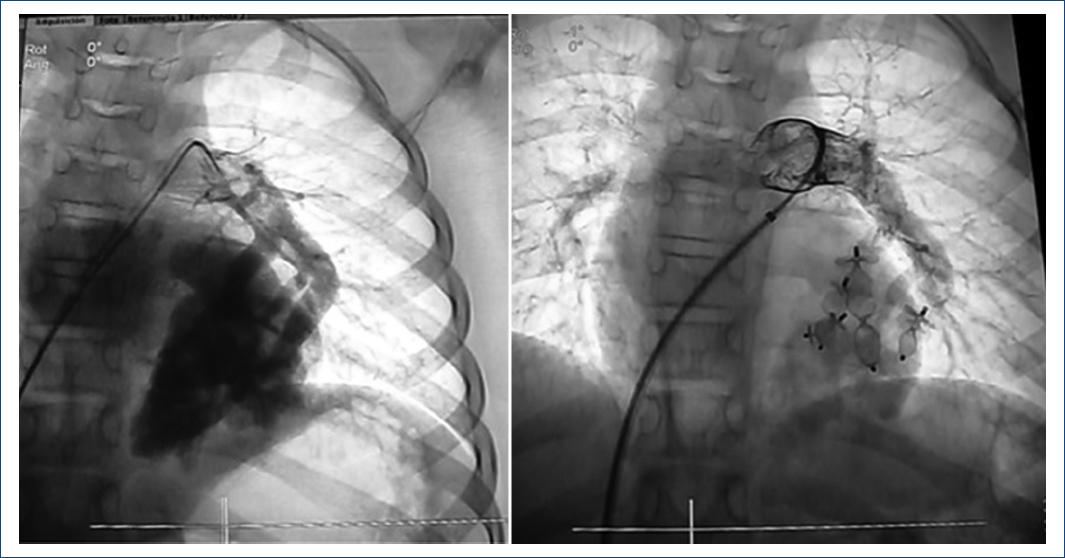
Figure 1 (Right) Selective angiography of the left lower lobar showing three pulmonary arteriovenous fistulas in this projection. (Left) Control after implantation of 4 Amplatzer vascular plugs II occlusion device.
Six-monthly follow-up was given and after 6 years the patient was asymptomatic, but her oxygen saturation decreased to 82%, so we performed a new diagnostic and interventional catheterization. Multiple angiographies were performed where a single anomalous vessel was identified (Fig. 2), we decided to use an 8 mm Amplatzer® Vascular Plug device II, Subsequent angiography confirmed total occlusion of the fistula and no other was observed. (Fig. 2), the patient had no complications and the oxygen saturation increased to 92%.
Discussion
OWRS occurs in approximately 10 to 20 individuals per 100,0003. With vascular involvement at different levels, being the pulmonary the most frequent, and the pulmonary arteriovenous fistulas the most reported lesions in these patients.
Until the 1980s, the treatment options in these cases were partial or total lobectomies, after which various percutaneous occlusion devices, mainly coils, began to be used with different degrees of success. The main difference between these approaches was the evolution and days of hospitalization.
In recent years, Amplatzer® devices have been the preferred device for occlusion of this type and, in general, for vascular malformations5,6. In the review of national and international publications, we did not find another case in which this number of malformations has been occluded percutaneously in the same patient and especially in the same lung, in some of the reported cases they were single lesions, and in those with multiple pulmonary arteriovenous fistulas, the location and/or size was not feasible for closure7-9.











 text new page (beta)
text new page (beta)



