Introduction
In the fetus, the right ventricle (RV) is the dominant chamber accounting for about 60% of total cardiac output and about 90% of the RV outflow volume is shunted from pulmonary artery to descending aorta through ductus arteriosus. Soon after birth, with aeration and expansion of lungs pulmonary vascular resistance (PVR) rapidly falls allowing increased pulmonary blood flow and reversal of shunt across ductus arteriosus. With increased pulmonary venous return leading to increased left atrial pressure foramen ovale closes soon and gradually ductus arteriosus closes in most term infants within first 24-48 h. This established the neonatal circulation. However, PVR remains high during the 1st few weeks of life and reached to nadir, equivalent to adults, at around 6 weeks of age. During this time, there is a gradual change in dominance of the ventricles. RV, which is the predominant ventricle during fetal period, remains bigger than LV during transitional circulation and gradually LV dominance takes over1,2.
There is evidence that RV plays a significant role during transition circulation. Conventionally, functional assessment just involved qualitative assessment based on a visual inspection, "eyeballing," but in recent years the growing interest among neonatologists and cardiologists to establish standard echocardiographic parameters to assess RV function quantitatively lead The American Society of Echocardiography (ASE) in 2010 to publish guidelines for the assessment of the right heart in children. Despite this, in Mexico there are no studies addressing this subject3,4.
The main goal of this study was to perform a simple ten parameter echocardiographic protocol to analyze RV function and obtain anatomical measurements in newborn babies during the first 72 h after birth, establishing normal reference values for Mexican neonates.
Methods
Study design
For this prospective study, 70 healthy term newborns were recruited between June and December 2018 from the neonatal Unit at Hospital Español de México, Mexico City. The health records of all newborns who received routine postnatal care were screened.
On the basis of ASE guidelines, we developed a comprehensive RV functional protocol for term babies (gestational age, 37-42 weeks) and after a well-informed written consent all eligible newborns had echocardiographic assessment as per protocol between 24 and 72 h after birth.
Inclusion criteria
The following criteria were term healthy neonates, normal APGAR score, and no history of any respiratory symptom. All exams were examined in a resting state without prior sedation and were allowed comfort bottle feeding during the assessment.
Exclusion criteria
The following criteria were all the known factors which potentially can impact transitional circulation and RV function such as: maternal diseases (diabetes mellitus, chorioamnionitis, and placental dysfunction), newborns with confirmed perinatal asphyxia or need for active resuscitation at birth, PDA > 1.5 mm or symptomatic, suspected sepsis or any known medical illness, presence of any congenital or genetic malformation, suspected or confirmed pulmonary hypertension or need for inotropic, and chronotropic drugs.
The study was approved by the ethics committee at Hospital Español de México.
Echocardiographic methods
A simple ten parameter echocardiographic protocol was applied in newborn babies during the first 72 h after birth. The measurements were derived using multiple views and modes of echocardiography as agreed in the protocol. An echocardiogram was performed using an Acuson X150 scanner with an 8-MHz transducer (Siemens Medical Solutions USA) with the use of electrocardiogram electrodes in all cases. All the studies were performed and analyzed by a single pediatric cardiologist and echocardiographist; the images were digitally store for further analysis.
RV dimensions
From an RV four-chamber (RV-4C) view, the tricuspid valve (TV) annular diameter was defined as a straight line joining the hinge points of the anterior and septal valve leaflets. The basal diameter was measured at the basal third of the RV cavity as the maximal distance from the RV lateral wall to the septum while maintaining a parallel orientation to the TV annulus (TVA). A straight line joining the midpoint of the TVA to the RV apex constituted the RV length. The mid cavity diameter was defined by a straight distance between the RV lateral wall and the septum running parallel to the TVA but passing through the mid-point of RV length. In addition, with the aim of quantifying right ventricular anteroinferior dimension, the right ventricular inflow tract view was obtained by angling the sound beam toward the patient's right hip. This was measured as the maximal diameter at the basal third of the RV cavity from its anterior to inferior walls while maintaining a parallel orientation with the TVA. All dimensions were measured in end-diastole.
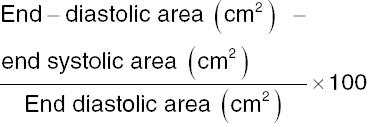
Fractional area change (FAC)
Right ventricular fractional area change (RVFAC) represents a surrogate measurement of RV ejection fraction and is expressed as a percentage change in the RV chamber area from end-diastole to end-systole, the RVFAC is calculated as follow:
Tricuspid annular plane systolic excursion (TAPSE)
TAPSE was measured by two-dimensional echocardiograph-guided M-mode recordings from the apical 4C view with the cursor place at free wall of the tricuspid annulus as parallel as possible.
TV inflow
TV inflow was assessed by placing a pulsed-wave (PW) sample gate of 2 mm at the tip of the TV leaflets during diastole with the Doppler beam parallel to the inflow as visualized using color Doppler echocardiography. Early (E) and late (A) TV inflow velocities and their ratio (E/A) were measured.
We also measured the tricuspid regurgitation (TR) expressed in mmHg by placing a continuous-wave (CW) Doppler 2 mm below the tip of the TV leaflets during diastole.
Myocardial velocities
Pulsed tissue Doppler imaging (TDI) of the tricuspid annulus was obtained by placing a PW Doppler just below the lateral tricuspid annulus. With this we could measure: Peak systolic (S´), early diastolic (E´), and late diastolic (A´) velocities.
RV myocardial performance index (MPI)
RV MPI or Tei index were measure by the time intervals: isovolumic contraction time (ICT), isovolumic relaxation time (IRT), and right ventricular ejection time (RVET). TDI and MPI were calculated by the use of the following formula.
MPI = [ICT (ms)+IRV ms)]/RVET (ms)
Pulmonary artery acceleration time (PAAT)
This parameter was measured from PW Doppler of the main pulmonary artery from the parasternal long-axis view of the RV outflow tract, we measured the beginning of pulmonary systolic flow till the peak of systolic ejection, and this parameter was expressed in milliseconds.
Results
Characteristics of patients and results of anatomical and functional parameters are summarized in tables 1 and 2, figures 1-6. A total of 70 full-term neonates fulfilled the inclusion criteria; based on weight we established anatomical parameters for basal, anteroinferior basal, mid cavity diameter, and length.
Table 1 Characteristics of the population mean and standard deviation (n = 70)
| Characteristics | Mean or proportion ± SD |
|---|---|
| Girls (%) | 55 |
| Boys (%) | 45 |
| Gestation weeks | 38.5 ± 2.7 |
| Weight (kg) | 3.1 ± 0.4 |
| Height (cm) | 48.7 ± 1.5 |
Table 2 Summary of echocardiographic parameters for right ventricular assessment in 70 patients. Data are expressed as mean ± SD
| Parameters | Mean ± SD |
|---|---|
| TV diameter (mm) | 13 ± 1.8 |
| Basal diameter (mm) | 16.7 ± 2 |
| RV length (mm) | 27.8 ± 2.2 |
| Mid cavity diameter (mm) | 14.3 ± 1.7 |
| RV-AIBD (mm) | 21.5 ± 2.5 |
| Tricuspid regurgitation (mmHg) | 13.3 ± 5.9 |
| FAVD 3C (%) | 37.8 ± 15.8 |
| FAVD 4C (%) | 40.6 ± 7.5 |
| Tricuspid E/A ratio | 0.7 ± 0.5 |
| MPI index | 0.5 ± 0.1 |
| Pulmonary artery acceleration time (ms) | 58.8 ± 14.9 |
TV: tricuspid valve, RV: right ventricle, RV-AIBD: right ventricular anteroinferior basal diameter, FAVD: fracción de acortamiento del VD, MPI: myocardial performance index.
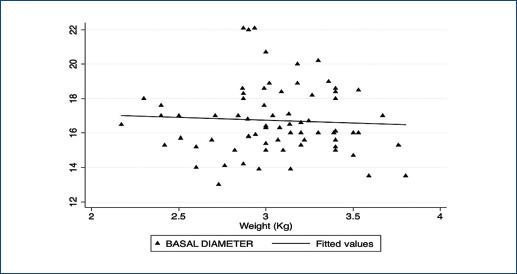
Figure 2 Weight versus observed value of basal RV diameter in mm (right ventricle). The mean is indicated by a solid black line.
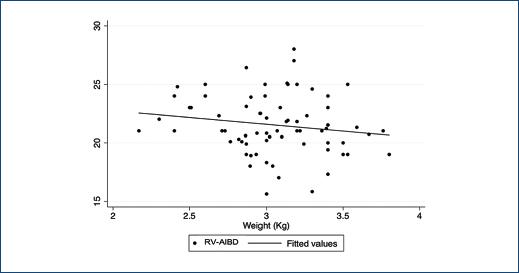
Figure 3 Weight versus observed value of right ventricular anteroinferior basal diameter in mm. The mean is indicated by a solid black line.
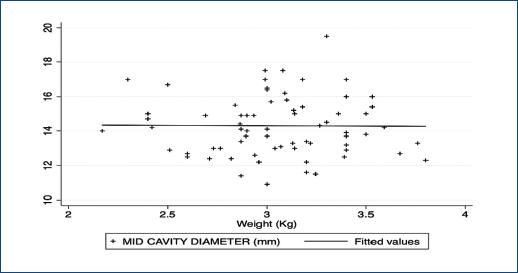
Figure 4 Weight versus observed value of mid cavity diameter measurement in mm. The mean is indicated by a solid black line.
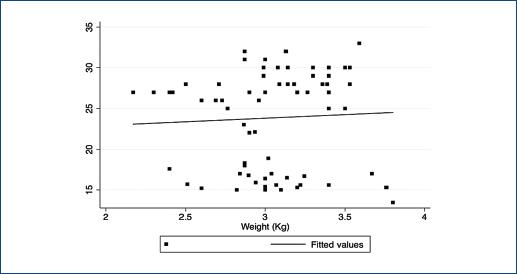
Figure 5 Weight versus observed value of right ventricular length measurement in mm. The mean is indicated by a solid black line.
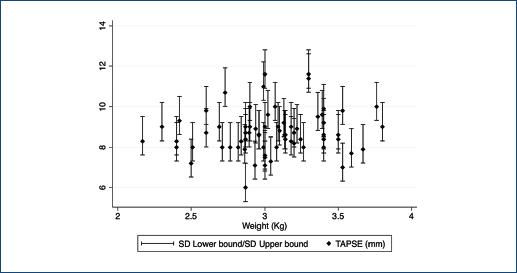
Figure 6 Mean tricuspid annular plane excursion values with error bars of ± 2 SD of the mean values for weight.
All values for TAPSE and TV measurements were in normal values based on Z score5,6, myocardial velocities on the peak systolic (s´), early diastolic (e´), and late diastolic (a´) contraction velocities were 8 (± 2.7), 9.6 (± 2.4), and 6.9 (± 1.2), respectively, MPI index mean was 0.5 (± 0.1). Finally, 13% neonates had flattening of interventricular septum and the mean PAAT was 58.8 ms ± 14.9.
Discussion
The RV function is recognized as a critical prognostic factor in the management of cardiopulmonary disorders and congenital heart defects in neonates7,8. This study establishes anatomic and functional parameters in Mexican healthy term infants during the transitional period.
The mean TAPSE value reported correlates with the study by Koestenberger et al. reporting a mean value of 8.6 mm for neonates around 38 weeks of gestation. This parameter was one with the lowest variation (± 1.1) and one of the most simple and reproducible echocardiographic parameters for RV function assessment5.
Mean RVFAC is similar to that reported by Levy et al. of 33% ± 5 in 25 term babies. However, in the same study, the FAVD 4C was higher in patients with a weight > 2.5 kg, reaching values above the 35% similar to our study involving healthy infants with good weight and height9.
Alp et al. reported values for MPI and myocardial velocities performed in neonates in the 1st day after birth in 50 term infants, values for tricuspid EA radio was 0.85 (vs. 0.7 in our study), E´ 6.4 cm/s ± 1.2, A´ 8.7 cm/s ± 1.3, S´ 6.5 cm/s ± 1.4 and MPI of RV of 0.46 ± 0.02 (vs. 8 cm/s ± 2.7, 9.6 cm/s ± 2.4, 6.9 cm/s ± 1.2, and 0.5 ± 0.1, respectively, in our study), their study group was very similar to ours with a mean birth weight and height of 3085 ± 256 g and 46.7 ± 3.4 cm, respectively10.
The use of Doppler measurement of PAAT is commonly used for the evaluation of PAP is well-established in adults and values <100 ms showed a linear inverse relationship between the PAAT and mean PAP in adults. A shorter PAAT suggests elevated pulmonary artery pressure (PAP) and PVR. From a study involving 113 neonates, Koestenberger et al. reported a mean PAAT value of 81 ms (range 53-104 ms) when mean heart rate was 131 beats per minute, he concluded PAAT value has an inverse relationship with the heart rate. In our study, we established a mean value for PAAT of 58.8 ± 14.9 ms, unfortunately we could not establish a correlation between the heart rate and the value of PAAT11,12.
The novel of this study was established reference values based on weight for basal diameter, RV length, mid cavity, and RV-AIB diameters, actually does not exist z score for this parameter so it is important to continue with this kind of studies to establish normal values in neonates.
Finally, in our cohort nine patients (13%) had mild flattening of interventricular septum, this group did not have any evidence of pulmonary hypertension, the mean value of TR was 18.7 mmHg (8-25 mmHg) and the mean value for PAAT was 56.8 ms (45-80 ms), this neonates were follow until their hospital discharge without any medical condition or complication and did not have readmission.
Study strengths and limitations
This study report for first time RV anatomical and functional parameters in Mexican neonates, for novel we could establish in base weight normal anatomical parameters for RV. Although the number of patients is small (70), as compared to previously reported studies this is 2nd largest study establishing normal reference values for RV function assessment in neonates.
The main limitation of this study was that we could not have interobserver variability due to the fact that only one pediatric cardiologist performed and analyzed the images. On the other hand, to our strength, the analysis was performed by said cardiologist who is highly trained and experienced in functional echocardiography. This study was not designed to measure cardiac output, assess left ventricle function, or measure size of foramen ovale. Finally, this study protocol did not include speckle-tracking, strain assessment and 3D imaging as a result of a lack of resources. Speckle tracking and 3D -imaging techniques seem promising to assess the RV function but till date they remain primarily research tools and need special expertise, currently available only in few centers around the world. Hence, we believe our protocol is simple and feasible to apply in clinical practice across the majority of neonatal and cardiac intensive care units.
Conclusions
The assessment of RV with echocardiogram is of utmost importance to the neonatologists and pediatric cardiologists providing care to sick neonates. To the best of our knowledge, this is the first study with important anatomical measurements and functional information in Mexican healthy term newborns. We recommend performing further prospective studies using similar protocols in preterm and sick neonates with underlying pathologies.











 text new page (beta)
text new page (beta)