Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista mexicana de cardiología
Print version ISSN 0188-2198
Rev. Mex. Cardiol vol.26 n.2 México Apr./Jun. 2015
Original Research
Regression of carotid intima-media thickness with nifedipine in hypertensive patients
Regresión del grosor de la interfase íntima-media carotídea con nifedipina en pacientes hipertensos (REINA)
Alejandra Meaney,* Gustavo Solache,* Víctor Manuel Reyes Macías,* Gabriela Gutiérrez-Salmeán,** Guillermo Ceballos,** Eduardo Meaney**
* Cardiovascular Unit, Hospital de Alta Especialidad "1o de Octubre". ISSSTE, Mexico City, Mexico.
** Laboratorio de Investigación Integral Cardiometabólica, Sección de Estudios de Postgrado e Investigación, Escuela Superior de Medicina del Instituto Politécnico Nacional, Mexico City, Mexico.
Correspondence to:
Eduardo Meaney, MD, PhD
Laboratorio de Investigación Integral Cardiometabólica.
Sección de Estudios de Postgrado e Investigación.
Escuela Superior de Medicina del Instituto Politécnico Nacional.
Plan de San Luis y Díaz Mirón s/n.
Colonia Casco de Santo Tomás,
Delegación Miguel Hidalgo. 11340, México, D.F.
Phone: (52) (55) 57296300, ext. 62820
E-mail: lalitomini@prodigy.net.mx
ABSTRACT
Background: Calcium channel blockers (CCBs) have proved to reduce both blood pressure levels and cardiovascular outcomes, including the development of atherosclerosis. The INSIGHT study showed a less pronounced progression of carotid intima-media thickness (IMT) in patients treated with nifedipine (NIF) vs. those treated with diuretics, but because IMT was normal in both groups, it was difficult to assess the anti-atherosclerotic effect of NIF. We compared the effect of NIF or hydrochlorothiazide (HCTZ) on atherosclerosis regression in hypertensive patients with abnormally thick IMT. Patients and methods: 37 hypertensive patients were randomly assigned to be treated with slow release-NIF (30 mg) and 46 to HCTZ (25 mg), all of them with IMT > 0.6 mm. IMT, lipid profile, and serum uric acid, potassium, and glucose were analyzed at baseline and 12 months later. Results: Blood pressure was equally well controlled with both treatments. No biochemical abnormality was observed in neither groups. IMT was reduced 35% in the NIF group in comparison to 9.3% in HCTZ group. Discussion: BBCs restore endothelial function, exert antioxidant activity and limit smooth muscle cells growth and proliferation, thus inhibiting fundamental atherogenic phenomena. Our results show a clear regression of IMT, marker of subclinical atherosclerosis with NIF. Conclusion: Both treatments were equally effective reducing blood pressure. HCTZ did not cause metabolic disarrays, but only NIF induced IMT regression. Basal IMT is a main determinant of regression.
Key words: Systemic arterial hypertension, nifedipine, hydrochlorothiazide, carotid intima-media interphase, subclinical atherosclerosis.
RESUMEN
Antecedentes: Los bloqueadores de los canales de calcio (BCC) han demostrado reducir tanto los niveles de presión arterial como los eventos cardiovasculares, incluyendo el desarrollo de la aterosclerosis. El estudio INSIGHT mostró una progresión menos pronunciada del grosor de la capa íntima-media de la carotídea (GIMC) en pacientes tratados con nifedipina (NIF) vs. los tratados con diuréticos, pero debido a que el GIMC fue normal en ambos grupos, resultó difícil evaluar el efecto anti-aterosclerótico de la NIF. El presente estudio comparó el efecto de la NIF o hidroclorotiazida (HCTZ) en la regresión de aterosclerosis en pacientes hipertensos con GIMC anormalmente gruesa. Pacientes y métodos: 37 pacientes hipertensos fueron asignados al azar para ser tratados con NIF de liberación lenta (30 mg) y 46 a HCTZ (25 mg), todos ellos con GIMC > 0.6 mm. GIMC, perfil lipídico, y ácido úrico en suero, potasio y glucosa se analizaron al principio y 12 meses más tarde. Discusión: Los BCC restauran la función endotelial, ejercen actividad antioxidante y limitan el crecimiento y la proliferación de las células del músculo liso, inhibiendo así fenómenos aterogénicos fundamentales. Nuestros resultados muestran una clara regresión del GIMC, marcador de aterosclerosis subclínica, con NIF. Conclusión: Ambos tratamientos fueron igualmente efectivos para reducir la presión arterial. HCTZ no causó desorden metabólico, pero sólo la NIF induce la regresión del GIMC. El GIMC basal es un determinante principal de la regresión.
Palabras clave: Hipertensión arterial sistémica, nifedipina, hidroclorotiazida, capa íntima-media de la carótida, aterosclerosis subclínica.
BACKGROUND
The clinical, epidemiological and socioeconomic importance of systemic arterial hypertension (SAH) resides in its capacity to damage the entire arterial vascular tree, from aorta to capillaries, through several intertwined pathogenic mechanisms, including abnormal hydraulic forces and their associated neurohumoral derangements, nitroxidative stress, inflammation, and endothelial dysfunction. In that manner, SAH is involved in the genesis of several forms of vascular disease such as atherosclerosis, hypertensive arteriosclerosis and arteriolosclerosis, senescent arteriosclerosis, lipohyalinosis and fibrinoid necrosis. Furthermore, SAH is also implicated in the direct hypertrophic lesion of the left ventricular myocardium, base of hypertensive heart disease.1-5 Undoubtedly, atherosclerotic plaques are the most threatening lesions caused by SAH, either alone or in association with other risk factors. Atherosclerotic vascular disease is preceded by a long free-symptoms period within which the finding of such asymptomatic lesions would allow the implementation of prophylactic interventions that could significantly delay clinical outcomes. In this context, high-resolution B-mode carotid ultrasonography is a reliable, repeatable, noninvasive, safe, and reasonably low-cost study, that is capable of detecting not only the existence of advanced atherosclerotic plaques, but also the abnormally augmented thickness of intima-media interphase (IMT), a condition that presents before the development of full-blown raised atheromatous lesions, thus somehow foretelling the occurrence of stroke or coronary syndromes.6
In the other hand, although all modern antihypertensive drugs are equally useful in attenuating high blood pressure, they differ in their potential to reduce vascular damage and splanchnic outcomes. Calcium channel blockers (CCBs) are useful therapeutic agents, with solid evidence about their antihypertensive power as well as cardiovascular protection.7,8 Even when some negative statements9,10 have been published in regards of calcium antagonists as antihypertensive drugs, several seminal large-scale studies have proven, beyond any doubt, their efficacy and safety, including an antiatherosclerotic effect.8,11,12 For example, the INSIGHT study13 compared the antihypertensive, metabolic, and antiatherosclerotic effects of two therapeutic regimes in high-risk hypertensive patients: slow-release nifedipine or a diuretic combination. The trial and one of the sub-analysis, the IMT-INSIGHT,14 showed a less pronounced progression of IMT, altogether with the same grade of blood pressure control and reduction of cardiovascular risk in the nifedipine-treated patients. The fact that basal values of IMT in both groups were within normal ranges, overshadowed the clear-cut effect of nifedipine on subclinical atherosclerosis progression. Hence the purpose of this study was to compare the effects of nifedipine vs. hydrochlorothiazide on metabolic and blood pressure parameters as well as on IMT regression in hypertensive patients who presented with abnormally thickened carotid intima-media interphase at baseline.
PATIENTS AND METHODS
We conducted a randomized clinical trial with two parallel arms, one receiving slow-release calcium channel blocker (nifedipine) and the other a thiazide diuretic (hydrochlothiazide). Hypertensive outpatients, of both genders, aged ≥ 20 years old, were recruited and randomly allocated in one of the two treatment groups. A convenience sample of 94 patients was assembled.
The study was approved by Institutional Ethics and Research Committees, and was conducted according with the Declaration of Helsinki, Good Clinical Practices and Mexican Federal Regulations.15-17 Patients were selected according to the following criteria: SAH grades 1 or 2 (Guidelines of the European Society of Cardiology/European Society of Hypertension),18 with systolic blood pressure (SBP) 140-179 mmHg, and diastolic blood pressure (DBP) 90-109 mmHg; IMT ≥ 0.6 mm; treatment-naïve or treated with β-blockers, ACE inhibitors or angiotensin receptor blockers. Patients were not included if they had grade 3 hypertension, diabetes mellitus, severe hypercholesterolemia, significant cardiovascular complications, severe systemic diseases (e.g., malignancies or HIV infection), history of drug or alcohol abuse. Women of child-bearing age, without a definite contraceptive method were also excluded.
In all patients, body weight was measured with a calibrated scale and recorded in kg; height was obtained in meters with a wall-stadiometer and body mass index (BMI) was further calculated. Blood pressure was measured in the sitting position, twice, with mercurial sphygmomanometers, following the standardized technique.18 Metabolic screening was performed by means of colorimetric assay kits -according with the manufacturer's instructions- and included fasting serum glucose, creatinine, uric acid, total cholesterol (TC), high-density lipoproteins cholesterol (HDL-c), and triglycerides (TG). Low-density lipoprotein cholesterol (LDL-c) was calculated using the Friedewald formula.19
IMT measurements were obtained using a high-resolution B-mode ultrasound machine (SONOS 7500) and a 7.5 MHz multi-frequency linear array probe, with the patient lying in supine decubitus, and the head, slightly hyperextended, rotated to the opposite side of examined carotid. Ultrasound examinations were performed by a single certified ultrasonographer, blinded to the type of treatment. B-mode images of the right carotid artery were obtained and IMT was measured by manual technique using electronic calipers, similar to the method described by Sidhu and Desai.20 For the purpose of this study, four points were selected for IMT measurements: the far and near the wall of the common carotid artery, one cm bellow the bifurcation (points 1 and 2), and the far and the near wall of the common carotid artery at the bifurcation level (points 3 and 4). The average IMT of these four points was considered in the final analysis.
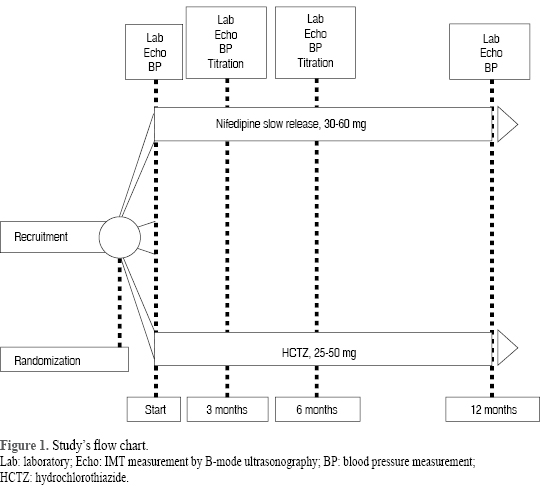
All antihypertensive medication was suspended for a wash-out period of two weeks. Patients were then randomly assigned to receive, at the beginning, either 30 mg of slow-release nifedipine (NIF), or 25 mg of hydrochlorothiazide (HCTZ); however, if no SAH control was achieved, additional therapy of 100 mg of metoprolol, daily, was allowed. Patients were examined at the start of the running period, and then at three, six and twelve months later. The examination included blood pressure determination and the IMT measurement. Also, a blood sample was drawn to measure the aforementioned biochemical variables. If blood pressures goals (< 140/90 mmHg) were not attained, medication doses could be titrated up to 60 mg of nifedipine or 50 mg de hydrochlorothiazide. Figure 1 summarizes the study's flow chart.
Statistical analysis. The software package used in the present study was SPSS v.16.0. Quantitative variables are presented as mean ± standard deviation; qualitative variables are presented as frequencies (percentages). Intragrupal differences were assed using repeated-measurements ANOVAs followed by Tukey's post hoc tests; whilst independent t-tests were performed in order to assess intergroup differences. Furthermore, we conducted bivariate and multivariate regression analysis. All tests were considered as statistically significant when p < 0.05.
RESULTS
83 (37 NIF and 46 HCTZ) patients completed the trial hence a per protocol statistical analysis was performed. The main causes of withdraw were consent retirement, lack of compliance or change of address.
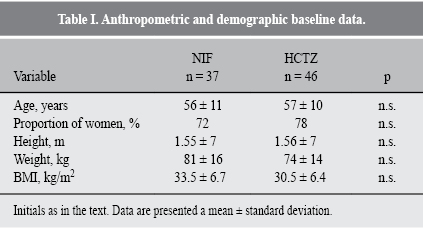
Anthropometric and demographic basal data were similar in both groups (Table I). Is worth mentioning that overweight and obesity presented as the prevalent nutritional phenotype, considering both means and standard deviations. In terms of gender, the proportion of women was greater in both groups.
Both treatments significantly reduced blood pressure levels in the vast majority of patients (Table II). It was noticeable that such reduction occurred since the first trimester, but the maximal descent was seen at the end of the study.
Neither metabolic nor anthropometric variables showed significant differences, in both, intragroup or intergroup analysis (Table III). Regarding adverse effects, only 5 cases of moderate ankle edema were observed in the nifedipine-treated patients, against nil in the diuretic treated group.
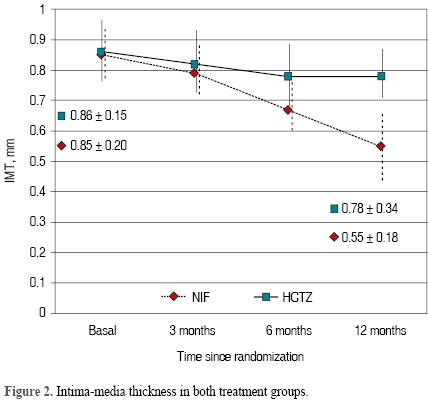
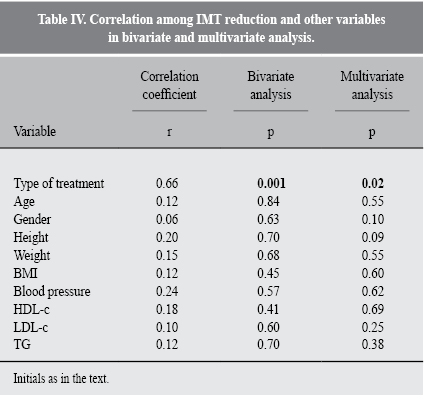
Finally, as seen in figure 2, mean carotid IMT was similarly abnormal at baseline: 0.85 mm in NIF group and 0.86 in the HCTZ group. However, while IMT descended scarcely and not significantly (≈9% by the end of the study) in HCTZ-treated patients, strikingly, in NIF-treated patients, such descent was ≈35% (from 0.85 to 0.55 mm, p < 0.05). Table IV shows the coefficient values comparing IMT reduction and other variables; the only significant correlation (p < 0.05, r = 0.66) was, precisely, the type of treatment (i.e., either NIF or HCTZ).
DISCUSSION
It has been established that the main goal in the treatment of SAH is the reduction and/or delay of vascular and organ damages.18-24 Although all modern antihypertensive drugs have been proven to lower both, high blood pressure and overall cardiovascular risk, there are pronounced differences -among antihypertensive drug families- regarding specific vascular and end-organ damage protection, e.g., regression of left ventricular and arterial hypertrophy, renal safeguard, antidiabetic effects, and antiatherosclerotic or antischemic effects, amidst others. As coronary and cerebral atherosclerotic lesions are common cause of death and disability in modern societies, the main purpose of antihypertensive treatment must be the reduction of atherosclerotic complications in those essential target organs. Very unfortunately, atherosclerosis is clinically silent during a long period of time, hence its first clinical manifestation is often a devastating or lethal coronary or cerebrovascular event.25,26 In this sense, ultrasonographic IMT measurement is a relatively cheap and reliable method to determine early atherosclerotic changes, thus allowing the implementation of pharmacologic and lifestyle interventions aimed to slow down or even induce regression of the atherosclerotic process. Nevertheless, data from multiple studies have pointed out that although IMT has an acceptable correlation with future cardiovascular outcomes and the extent of coronary atherosclerosis,27,28 it is not superior to the traditional stratification of risk factors for cardiovascular risk.29
Carotid IMT is reduced by several therapeutic interventions, among them, the use of antihypertensive drugs.30 In several studies, CCBs have been proven to effectively reduce the progression of carotid IMT,31 and in fact, much better than diuretics, β-blockers or ACE inhibitors.30,32 The IMT-INSIGHT substudy,14 showed that while a combination of two diuretics, hydrochlorothiazide and amiloride, did not influence carotid thickening, a slow-release form of nifedipine retarded the atherosclerotic progression. Nevertheless, baseline values of IMT, in both groups, were within the limits of normality, so the clear-cut antiatherosclerotic effect of both treatments was only revealed by a rather complicated analysis in which histograms of individual slopes of IMT modifications during a period of four years were plotted in order to visualize small differences in the thick of carotid wall. The yielding results were that the diuretic combination did not change the progression of IMT, while nifedipine caused a somehow negative slope, indicating a scanty regression of wall thickening. It was also noticed, that this lower slope correlated with increased baseline IMT. Of course, it is illusory to expect a great reduction of carotid IMT if there is no thickening at all at the base. This methodological flaw explained, for example, the "failure" of the combination of simvastatin/ezetimibe in diminishing the carotid IMT in patients with familial hypercholesterolemia (ENHANCE study),33 but no subclinical atherosclerosis. As one of the ENHANCE study stated:34 the "most important determinant of any clinical trial... is to have the presence of disease at baseline". In contrast, the present study included only patients with abnormally gross carotid IMT, i.e., with "disease at baseline". It was certainly surprising that the NIF-treated patients showed such significant IMT reductions, far out of the common results found in other trials. There is a possible explanation, raised by Orio's findings of an IMT reduction ≈20% in women with polycystic ovary syndrome treated with metformin:35 the anti-inflammatory effect of certain drugs (e.g., statins, metformin, pioglitazone, CCBs) can shrink -in a short time- the carotid wall due to the attenuation the inflammatory process that accompanies all vascular risk factors. These antinflammatory changes that result in diminishing wall volume and thickness, are significantly more rapid than the slower process of true atherosclerotic regression. Of course, this is just a speculative consideration that is not sustained with the data of this study.
Yet another hypothesis for elucidating the herein found results is the fact that there are substantial pleiotropic effects of CCBs beyond their remarkable antihypertensive effects. As it is well known, the starting point of vascular damage, cause by all vascular risk factors is a triad composed by endothelial dysfunction, nitroxidation and inflammation.36 Dihydropyridine or nifedipine-like CCBs (DHP-type CCBs), block the membrane L-type calcium channel thus decrease intracellular calcium. This increase of intracellular calcium activates endothelial nitric oxide (NO) synthase (eNOS) enhancing NO availability. Moreover, some CCBs, like nifedipine, have notorious effects as superoxide scavengers. Since a practical (although excessively simple) definition of endothelial dysfunction is a reduced NO availability and an augmented production of reactive oxygen substances, CCBs can restore the equilibrium between these two dialectic antagonists. Furthermore, there are evidences that DHP-type CCBs exert antioxidant effects limiting the oxidation of LDL cholesterol, fundamental phenomenon in atherogenesis. In the same manner, vascular smooth muscle cells (VSMC) growth and proliferation is another complex and multifactorial event in atherogenesis, in which calcium is directly involved.37 So, the reduction of intracellular calcium inhibits the development of both, the primary atherosis, and the later phenomenon, sclerosis, that in sequence yield to the growth of atherosclerosis plaques. The bivariate and multivariate analysis in our study showed that the only responsible of the IMT reduction was the type of treatment.
Otherwise, both treatments were equally effective in attaining therapeutic goals. In the patients of this study, no were observed the frightful metabolic disarrays attributed to diuretics. In fact, at the end, serum potassium was lower, and uric acid was higher in the diuretic-treated group, but the statistical differences were not significant.
CONCLUSION
Our data show that both treatments (CCBs and HCTZ) are equally effective as antihypertensive regimes. Also, they show that in these patients, the metabolic effects of thiazides were unimportant. The reduction of carotid IMT, observed by a blind to treatment researcher, is in accordance with other observation around the world. Our results emphasizes that the basal magnitude if IMT is a main determinant of its pharmacological regression. We admit the limitations of the study: the essay was not double blind; the lack of two different sonographers, the relative small size of the sample and the semi-automatized measuring of wall borders.
REFERENCIAS
1. Chobanian AV. Vascular effects of systemic hypertension. Am J Cardiol. 1992; 69: 3E-7E. [ Links ]
2. Touyz RM. Molecular and cellular mechanisms in vascular injury in hypertension: role of angiotensin II. Curr Opin Nephrol Hypertens. 2005; 14: 125-131. [ Links ]
3. Hsueh WA, Anderson PW. Hypertension, the endothelial cell, and the vascular complications of diabetes mellitus. Hypertension. 1992; 20: 253-263. [ Links ]
4. Erusalimsky JD, Kurz DJ. Cellular senescence in vivo: its relevance in ageing and cardiovascular disease. Exp Gerontol. 2005; 40: 634-642. [ Links ]
5. Drazner MH. The progression of hypertensive heart disease. Circulation. 2011; 123: 327-334. [ Links ]
6. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction. The Rotterdam study. Circulation. 1997; 96: 1432-1437. [ Links ]
7. Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomized trials. Lancet. 2000; 356: 1955-1964. [ Links ]
8. Trenkwalder P. Antihypertensive treatment with calcium channel blockers: pharmacological pornography or useful intervention? Nephrol Dial Transplant. 2004; 19: 17-20. [ Links ]
9. Pahor M, Psaty BM, Alderman MH, Applegate WB, Williamson JD, Cavazzini C et al. Health outcomes associated with calcium channel antagonists compared with other first-line antihypertensive therapies: a meta-analysis of randomised controlled trials. Lancet. 2000; 356: 1949-1954. [ Links ]
10. Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckber SR et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and metaanalysis. JAMA. 1997; 277: 739-745. [ Links ]
11. Simon A, Levenson J. Effects of calcium channel blockers on atherosclerosis: new insights. Acta Cardiol. 2002; 57: 249-255. [ Links ]
12. Tzivoni D. End organ protection by calcium-channel blockers. Clin Cardiol. 2001; 24: 102-106. [ Links ]
13. Brown MJ, Palmer CR, Castaigne A, de Leeuw PW, Mancia G, Rosenthal T et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet. 2000; 356: 366-372. [ Links ]
14. Gariepy J, Simon A, Chironi G, Moyse D, Levenson J. Large artery wall thickening and its determinants under antihypertensive treatment: the IMT-INSIGHT study. J Hypertens. 2004; 22: 137-143. [ Links ]
15. World Medical Association, Declaration of Helsinki. Adopted in the 18th World Medical Assembly. Helsinki (Finland, 1964) and corrected in the 29th Assembly (Tokyo, Japan 1975), the 35th (Venice, Italy, 1983) and the 41 (Hong Kong, 1989). Available in: http://ohsr.od.nih.gov/helsinki.php3 [ Links ]
16. ICH Guidelines for Good Clinical Practice. International Conference on Harmonisation for Technical Requirements for the Registration of Pharmaceuticals for Human Use. ICH Harmonised tripartite R Guideline. London. ICH. 1996. [ Links ]
17. Ley General de Salud, Reglamento de Investigación Clínica. Título 5o. Capítulo único. Diario Oficial de la Federación, el 24 de diciembre de 1986. [ Links ]
18. TheTask Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens. 2013; 31: 1281-1357. [ Links ]
19. Friedwald WT, Levy IR, Frederickson DS. Estimation of the concentration of low density lipoprotein cholesterol in plasma without use of the preparative ultracentrifuge. Clin Chem. 1972; 18: 499-502. [ Links ]
20. Sidhu PS, Desai SR. A simple and reproducible method for assessing intimal-medial thickness of the common carotid artery. Br J Radiol. 1997; 70: 85-89. [ Links ]
21. Lim TK, Lim E, Dwivedi G, Kooner J, Senior R. Normal value of carotid intima-media thickness-a surrogate marker of atherosclersosis: quantitative assessment by B-mode carotid ultrasound. JASE. 2008; 21: 112-116. [ Links ]
22. Simon A, Gariepy J, Chironi G, Megnien JL, Levenson J. Intima-media thickness: a new tool for diagnosis and treatment of cardiovascular risk. J Hypertens. 2002; 20: 159-169. [ Links ]
23. Jarauta E, Mateo-Gallego R, Bea A, Burillo E, Calmarza P, Civeira F. Carotid intima-media thickness in subjects with no cardiovascular risk factors. Rev Esp Cardiol. 2010; 63: 97-102. [ Links ]
24. Dahlöf B. End-organ damage: does it really matter how we prevent it? Eur Heart J. 2003; 5 (Suppl F): F33-F39. [ Links ]
25. Toth PP. Subclinical atherosclerosis: what it is, what it means and what we can do about it. Int J Clin Pract. 2008; 62: 1246-1254. [ Links ]
26. Espeland MA, Craven TE, Riley WA, Corson J, Romont A, Furberg CD. Reliability of longitudinal ultrasonographic measurements of carotid intimal-medial thicknesses for the Asymptomatic Carotid Artery Progression Study Research Group. Stroke. 1996; 27: 480-485. [ Links ]
27. Hulthe J, Wikstrand J, Emanuelsson H, Wiklund O, de Feyter PJ, Wendelhag I. Atherosclerotic changes in the carotid artery bulb as measured by B-mode ultrasound are associated with the extent of coronary atherosclerosis. Stroke. 1997; 28: 1189-1194. [ Links ]
28. Baldassarre D, Amato M, Bondioli A, Sirtori CR, Tremoli E. Carotid artery intima-media thickness measured by ultrasonography in normal clinical practice correlates well with atherosclerosis risk factors. Stroke. 2000; 31: 2426-2430. [ Links ]
29. Agewall S, Fagerberg B, Berglund G, Schmidt C, Wendelhag I, Wikstrand J et al. Multiple risk intervention trial in high risk hypertensive men: comparison of ultrasound intima-media thickness and clinical outcome during 6 years of follow-up. J Intern Med. 2001; 249: 305-314. [ Links ]
30. Cuspidi C, Negri F, Giudici V, Capra A, Sala C. Effects of antihypertensive drugs on carotid intima-media thickness: Focus on angiotensin II receptor blockers. A review of randomized, controlled trials. Integr Blood Press Control. 2009; 2: 1-8. [ Links ]
31. Terpstra WF, May JF, Smit AJ, de Graeff PA, Crijns HJ. Effects of nifedipine on carotid and femoral arterial wall thickness in previously untreated hypertensive patients. Blood Press Suppl. 2003; 1: 22-29. [ Links ]
32. Tropeano AI, Saleh N, Hawajri N, Macquin-Mavier I, Maison P. Do all antihypertensive drugs improve carotid intima-media thickness? A network meta-analysis of randomized controlled trials. Fundam Clin Pharmacol. 2011; 25 (3): 395-404. [ Links ]
33. Kastelein JJP, Akdim F, Stroes ESG, Zwinderman AH, Bots ML, Stalenhoef AFH et al. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med. 2008; 358: 1431-1443. [ Links ]
34. Stein EA. After ENHANCE: is more LDL cholesterol lowering even better? Clin Chem. 2008; 54: 940-942. [ Links ]
35. Orio F Jr, Palomba S, Cascella T, De Simona B, Manguso F, Savastano S et al. Improvement in endothelial structure and function after metformin treatment in young normal-weight women with polycystic ovary syndrome: results of a 6-month study. J Clin Endocrin Metab. 2005; 90: 6072-6076. [ Links ]
36. Mason RP. Pleiotropic effects of calcium channel blockers. Curr Hypertens Rep. 2012; 14: 293-303. [ Links ]
37. Mason RP, Marche P, Hintze TH. Novel vascular biology of third-generation L-type calcium channel antagonists. Ancillary actions of amlodipine. Arterioscler Thromb Vasc Biol. 2003; 23: 2155-2163. [ Links ]
Nota
Este artículo puede ser consultado en versión completa en: http://www.medigraphic.com/revmexcardiol














