Services on Demand
Journal
Article
Indicators
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista mexicana de análisis de la conducta
Print version ISSN 0185-4534
Rev. mex. anál. conducta vol.34 n.2 México Dec. 2008
A Behavioral Self–recording Procedure in the Management of Breast Cancer: A Field Test with Disadvantaged Participants1
Procedimiento de autorregistro conductual en la atención del cáncer de mama: Prueba de campo con pacientes marginadas
Juan José Sánchez–Sosa and Salvador Alvarado Aguilar
National University of Mexico, Nacional Cancer Institute of Mexico. Corresponding author: johannes@unam.mx
Received: 24 October, 2008
Reviewed: 14 November, 2008
Accepted: 13 December 2008.
Abstract
Breast cancer prevalence in many developing nations such as those in Latin America continues to grow at a pace that deserves serious attention, since cancer accounts for high morbidity and mortality rates among relatively young women (LaVecchia & Bosetti, 2005). From a clinical standpoint, breast cancer patients suffer not only from the symptoms of cancer itself but from side–effects of invasive treatments (Burish, Shartner & Lyles, 1981; Donovan, Small, Andrykowski, Munster & Jacobsen, 2007; Falleti, Sanfilippo, Maruff, Weih, & Phillips, 2005). In addition to dealing with distress, the home–care component of breast cancer treatment demands complex routines and behaviors which patients with little or no schooling and other socioeconomic disadvantages have serious difficulty implementing. The purpose of the present study was to field test a behavioral self recording procedure with the first six patients who completed treatment, and to probe preliminary effects of a behavioral intervention to support healthcare and reduce distress. Results point toward a reliable, low–cost and practical recording system; as well as improvement in most behavioral and emotional categories for practically all participants.
Key words: hospital, women, illiteracy, relatives, survival.
Resumen
La prevalencia de cáncer de mama en países en desarrollo, como los de Latinoamérica aumenta a ritmos que demandan atención seria pues ocasiona alta morbilidad y mortalidad entre mujeres en edad productiva (LaVecchia & Bosetti, 2005). Desde una óptica clínica, las pacientes no sólo sufren por la sintomatología del cáncer sino por los efectos indeseables de tratamientos invasivos (Burish, Shartner & Lyles, 1981; Donovan, Small, Andrykowski, Munster & Jacobsen, 2007; Falleti, Sanfilippo, Maruff, Weih, & Phillips, 2005). Además de lidiar con el distrés, el autocuidado del cáncer exige rutinas y conductas complejas muy difíciles de instrumentar por pacientes con poca o ninguna escolaridad y otras limitaciones socioeconómicas. El objetivo del presente estudio fue probar un sistema de autoregistro conductual y sondear los efectos de una intervención conductual como apoyo al tratamiento y reducción del estrés en pacientes con cáncer mamario y con baja escolaridad. La prueba incluyó las primeras seis pacientes de un grupo de 87, con máximo de primaria inconclusa, que completaron el tratamiento. Los resultados apuntan hacia un sistema confiable, económico y práctico; además de mejoría notoria en la mayoría de las categorías conductuales y emocionales para prácticamente todas las participantes.
Palabras clave: hospital, mujeres, analfabetismo, familiares, sobrevivencia.
Cancer continues to be a disease for which neither preventive measures nor therapeutic interventions have shown satisfactory morbidity and mortality improvements in the last decade, especially in developing countries such as those in Latin America. As an example, in most such countries, epidemiological surveillance agencies continue to designate breast cancer as one of the main causes of mortality. In Mexico breast cancer currently represents 6% of all deaths by malignancies, with its highest incidence (six times–fold) in the 35–44 age bracket (LaVecchia & Bosetti, 2005).
Breast cancer patients suffer not only the symptoms of the condition itself, but extreme discomfort and/or pain stemming from invasive treatments such as surgery, radiation and chemotherapy (Burish, Shartner & Lyles, 1981; Donovan, Small, Andrykowski, Munster & Jacobsen, 2007; Falleti, Sanfilippo, Maruff, Weih & Phillips, 2005). Indeed, the treatment of breast cancer requires the systematic implementation of a wide array of assessment and therapeutic actions. Some such tasks are carried out by physicians, nurses, laboratory technicians and other health professionals in a hospital but others depend primarily on the patient and/or her home primary caregiver in case one is available. Caring for cancer at home requires displaying rather systematic and sometimes complex sets of behaviors needed to support successful medical treatment (Richardson, Shelton, Krailo & Levine, 1990).
THERAPEUTIC ADHERENCE
Patients are expected to abide by a series of directions and recommendations prescribed by the medical team (Miaskowski, Dodd, West, Paul, & Tripathy, 2001; Perna, Craft, Charles & Antoni, 2008). Some of the most important include: showing up for hospital appointments (Drury, Harcourt & Minton, 1996), punctually taking medications in definite amounts and modes (Horne & Weinman, 1999), reducing exposure to specific environmental situations such as high temperatures and sunlight (Teas, Davis, Raghavan, Oman & Nitcheva, 2003), keeping a well balanced diet excluding some specific food types and including others (Cerully, Klein & McCaul, 2006; Rooney & Wald, 2007) and engaging in moderate amounts of distinct types of physical activity (Perna, Craft, Carver & Antoni, 2008) among others. For chronic–degenerative diseases in general and cancer in particular, therapeutic adherence is a key element predicting survival with reasonable quality of life, two top priorities in its treatment.
Adherence behaviors are naturally based on personal learning histories which, in turn, assume a minimum of competence, schooling and interpersonal skills (Bradley, Johnston, Hagglund, Davidson, Hutchinson, Walker & Kelly, 2001; Hotz, Kaptein, Pruitt, Sanchez–Sosa & Willey, 2003). Many breast cancer patients under treatment at public healthcare institutions in developing countries, however, come from such socioeconomic conditions that they lack many of the required prerequisites to engage in treatment–supporting behaviors (Budakoglu, Maral, Ozdemir & Bumin, 2007; Chandra, Chaturvedi, Channabasavanna, Anantha, Reddy, Sharma & Rao, 1998; Wan, Zhang, Tang, Zhang, Li, Ren, He & Wang, 2003). Some such prerequisites may even include reading and writing or being able to understand directions.
VERBAL PRIVATE EVENTS AND EMOTIONAL REACTIONS
In addition, many patients hold convictions leading to or associated with mal–adaptive behaviors regarding healthcare. These private verbal events are frequently based on faulty information on health in general and cancer in particular, or on culturally biased aphorisms. Some examples drawn from participants in the present study include: "cancer is practically a death sentence, there is nothing anyone can do about it" or, "medicines are toxic and poisonous, they will end up killing me before cancer does" or "cancer is a punishment for something terrible I must have done" or "I am sure praying will make cancer go away" or "cancer treatment is painful and terrible, I will never endure it". These and other similar interfering (with healthcare) statements by cancer patients have also been documented in the research literature (Cerully, Klein, & McCaul, 2006; Friedman, Romero, Elledge, Chang, Kalidas, Dulay, Lynch & Osborne, 2007; Rabin & Pinto, 2006).
These types of convictions and the lack of self–care abilities also facilitate the appearance of such respondents as emotional reactions of various types and intensities. Some of the most frequent involve severe anxiety, deep sadness, crying and utterances associated to helplessness and hopelessness, and associated with generalized behavioral de–activation and poorer medical prognostic (Anagnostopoulos, Kolokotroni, Spanea, & Chryssochoou, 2006; Garssen, 2004; Greer, 2008; Izdebski, 2007).
Since these components and the lack of schooling severely limit the viability of interventions aimed at improving the patients condition and reducing distress, the establishment of self–care skills, modifying incompatible private verbal events and behaviorally regulating maladaptive emotional responses become an important applied behavioral priority in the case of breast cancer patients. Some such interventions have shown improvements in cancer patients functioning and wellbeing (Kim, Lee, Choe, Yi, Choi & Kwon, 2005; Pojoga, 2001; Yan, Wenjuan, Xinfan, Zhang, Hardy & Mauntainbear, 2001).
THE SCOPE OF INTERVENTIONS
Addressing the general level of education and learning of these patients as a dependent variable is not a practical option. Thus, the design and application of materials and strategies to support cancer treatment must feature attributes seeking to compensate for such deficiencies. A crucial methodological prerequisite needs to be addressed first, since evaluating applied interventions normally requires direct behavioral observation and recording conducted in the home of participants. When such tasks prove onerous or non–viable, reliable self recording becomes a practical next option. Reliable behavioral self–recording has been documented in experimental studies with participants such as adolescents with multiple handicaps (Morrow, Burke & Buell, 1985), preschool children (Lee & Piersel, 1989), anxious undergraduates (Hamilton & Bornstein, 1977), and college students (Lipinski, Black, Nelson & Ciminero, 1975; Lipinski & Nelson, 1974) among others.
Research studies on the behavioral effects of experimentally–evaluated interventions on breast cancer are few, probably due to the predominance of approaches derived from the biological and medical areas or from psychometric scaling traditions. The first usually involve such measurements as count of immune Natural Killer cells "NK" (Levy, Herberman, Lippman & D'Angelo, 1987) or patient survival rates (Spiegel, Bloom, Kraemer & Gottheil, 1994). Despite the natural high validity of these dependent measures, there are very few studies linking such effects to behavioral ones (Safren, Hendriksen, Desousa, Boswell & Mayer, 2003; Safren, Otto, Worth, Salomon, Johnson, Mayer & Boswell, 2001). On the other hand, questionnaire–based studies usually rely on the assumption that there are few or no relevant contingencies affecting actual correspondence between participants' verbal responses and the specific non–verbal behaviors that comprise self care and therapeutic adherence (Piña–López, Dávila–Tapia, Sánchez–Sosa, Togawa & Cázares–Robles, 2008).
This context emphasizes the importance of developing reliable and practical low–cost behavioral self recording procedures which will allow for the evaluation of interventions aimed at effective home–based self care of breast cancer. Thus, the purpose of the present study was to develop and pilot test one such procedure with low schooling breast cancer patients in a public healthcare facility in Mexico City.
METHOD
Participants
From a total of 87 patients currently participating in an overall behavioral protocol, the data from the first six who completed both pre–intervention measurements and at least one posttest measurement were analyzed (see e.g. Kazdin, 1982). All six participants had a confirmed diagnostic of breast cancer with at least three months of evolution and were recipients of healthcare services at the main hospital of Mexico's National Cancer Institute. This facility belongs to one of three Mexican public healthcare systems and provides services to individuals with no employment and no institutional affiliation qualifying them for alternate healthcare systems (Sanchez–Sosa, 2007). Potential participants were initially excluded from the protocol if they had a psychiatric diagnostic, including retardation, were in an unambiguous terminal phase or were participating in another study. All participants (or their household) had a monthly income situating them at, or slightly above minimum wage. Four of the six patients had not finished elementary education and two had completed this cycle (six years in the Mexican system). It should be noted that many individuals completing the elementary cycle still show functional illiteracy (Parra, Mazón, Rojas–Drummond & Espinosa–Velez, 2005).
Measurement
The selection of behaviors to be recorded was based on three sources. The first involved a review of the research literature on the most frequent complaints by breast cancer patients regarding suffering related to the condition itself or to its medical treatment (McDaniel, Musselman, Porter, Reed & Nemeroff, 1995). Second, weekly meetings with the oncologists of the hospital's breast cancer service led lo listing patient behaviors identified in the hospital medical practice as either supporting or interfering with treatment from the medical standpoint. The third was a series of preliminary interviews with the patients themselves in order to add or adjust the specific description of behaviors or complaints listed from the other two sources. Thus validity of the dependent measures was set up through registering the actual experience by the hospital's oncologists and psycho–oncologists as well as comparing specific outcomes of the research literature relating cancer treatment–prognostic and behavioral variables. Variables reflecting consistent findings were then adopted for the design of recording materials and procedures (See e.g., Garssen, 2004; Horne & Weinman, 1999; Izdebski, 2007; Rabin & Pinto, 2006; Stanton & Reed, 2003).
The main behavioral self–recording instrument consisted in a portable (passport size) booklet containing twelve pages with expressly designed spaces for recording the behavioral categories described below and other pertinent additional information, for one week. The cover registered such data as name, age, home telephone number (if any), phone number to leave messages with a nearby neighbor or relative, name of behavior therapist, date and time of the next hospital appointment, and space for brief notes on the back cover. Except for the written information required on the covers, usually inserted by the therapist or a nurse if the patient could not write, all recording spaces contained a clearly visible pictogram representing individuals exhibiting the behavior in question or the object needed to engage in such behavior (e. g., food, toothbrush, bed, etc.). Thus, patients only had to tick the appropriate space in order to register one occurrence of the behavior. All pictograms were previously tested for clarity and pertinence through revisions by the project staff and at least one patient per therapist.
Once the research team agreed on the final set of behaviors, definitions were developed as follows:
Taking medication
Having taken the specific amount of pills (drops, spoonfuls, etc.) as prescribed by the physician and recorded on the hospital files, at no more than one hour off the specified times in 24 hour periods.
Diet
It involved daily number of food portions prescribed by the hospital, including sources of protein, carbohydrates, dairy products, cereals, vegetables and water as prescribed by the physician.
Physical exercise
Engaging in physical activity for a minimum of twenty minutes daily and until breaking a sweat, except when alternate specific instructions were provided by the physician.
Performance at work
The number of days (for employed patients) in a week in which they attended work and remained on task as usually distributed for all similar employees. For unemployed patients, the number of usual home activities such as cleaning, doing the laundry and/or other house chores.
Restful sleep
Number of days in a week in which the patient slept at night with only minor interruptions (adding to less than an estimated total of thirty minutes) and waking up refreshed.
Deep muscle Relaxation
Carrying out the specified (as trained) deep muscle relaxation procedures (alternating tension–relaxation) in a specific cephalous–caudal sequence as follows: forehead, cheeks, lips, jaw, neck, shoulders, arms, hands, abdomen, buttocks, legs, ankles and feet. Breathing specifications during relaxation included three requirements: deep, diaphragmatic (as opposed to clavicular breathing) and slow (approximately eight seconds from the start of inhaling to finishing exhaling) as modeled by the experimenters during training (Fahrion & Norris, 1990; Lehrer, 1996).
Sexual activity
Number of days in a week in which the patient engaged in some kind of intimate sexual encounter.
Time with family or friends
Number of days in a week in which the patient spent a minimum of thirty minutes in amenable chatting or similar activity with one or more relatives or friends.
Recreation
Number of days in a week in which the patient engaged in some recreational activity (watching a movie, listening to the radio, dancing, etc.) with family, friends or by herself.
Hygiene and body care
The weekly frequency of Ave behaviors: showering, tooth brushing, keeping skin hydrated, wearing comfortable clothes and avoiding personal exposure to high temperature situations.
Risky behaviors
Weekly frequency of smoking, drinking alcoholic beverages, eating (specified) foods containing preservatives such as nitrates and nitrites, canned foods, foods with high animal fat content and industrially processed ("junk") foods.
Identifiable emotional reactions
Weekly frequency of predominating self–perceived emotional reactions in 24hour periods: sad, happy, angry, anxious, and other.
Additional records
Finally, the booklet contained space for notes regarding doubts or questions by the patient in relation to treatments, medical estimates/statements, opinions, etc. These data, as well as listing specific home tasks for the patients and/or their home caregivers (if any) were asked/assigned by the behavior therapist to the patient every week and written down and explained to both patient and caregiver in case the patient could not write.
All therapists were provided with specially designed forms to be filled out by him/her during each and every session with a patient. These sheets, called "Treatment Binnacle" (as in a marine log chart or book) were designed so as to support decisionmaking in each successive session and to record therapists clinical notes and comments. The binnacle was labeled so that it specifically requested a written description of any relevant behavior by the patient which would fall in any of the three general categories to be addressed during the intervention. Thus the binnacle included specific writing spaces requesting therapaists to note down three types of events: first, patient behaviors as reported by the patients or as exhibited in the office. These included emotional reactions, verbal events incompatible with self–care and wellbeing, and the need for new behaviors to be established. The second type of event included explicit procedures implemented by the therapist in the session aimed at modifying such verbal events and emotional reactions or at establishing new self–care behaviors. The third category involved specific goals or issues to be addressed in the next session, clinical notes and observations or significant requests by the patients, and general patient ID information. Thus the binnacle called for recording both observations, interventions and patient progress notes and other relevant clinical descriptions.
Therapist training
All interviews, data collection and intervention procedures were conducted by seven advanced licensing–degree students from the School of Psychology of Mexico's National University. Students were first selected on the basis of their GPA and specific grades in applied, behaviorally oriented courses (all above 8.5 in a 0 to 10 scale). After successfully passing an advanced course on cognitive and behavioral therapy they received additional training on behavioral interventions for breast cancer patients. The advanced course included a detailed analysis of selected readings from the contemporary literature on the experimental evaluation of behavior change in the health area. Readings included such topics as: experimental single–subject designs, extraneous variables control techniques, definition criteria for abnormal behavior, retrospective risk–factor analysis, behavioral observation and data collection procedures, effective client–therapist interaction and communication, techniques for detecting and changing dysfunctional beliefs, establishing health self–care behaviors, detecting and modifying dysfunctional emotional reactions, and formulation of clinical reports, among others.
The additional training on behavioral interventions for breast cancer patients lasted for two semesters after completing course, laboratory and practicum work in the typical licensing degree university education for psychologists in Mexico, described elsewhere (Burgess, Sternberger, Sanchez–Sosa, Lunt, Shealy & Ritchie, 2004; Hernández–Guzmán & Sánchez–Sosa, 2005; Sanchez–Sosa, 2007), which resembles a professional degree similar to a PsyD in the US.
During this additional year students worked in weekly seminar sessions covering the analysis of selected readings from the contemporary research literature on psychological interventions for breast cancer patients. The seminar included analysis of contemporary research articles and case studies on experimentally evaluated healthcare interventions in the area of cancer in general and breast cancer in particular. Titles included a wide array of topics such as stress management (Bower & Segerstrom, 2004), long–term outcomes of breast reconstruction (Wilkins, 1998), insomnia (Quesnel, Savard, Simard, Ivers & Morin, 2003), uncertainty management (Mishel, Germino, Gil, Belyea, Carlton–Laney, Stewart, Porter & Clayton, 2005) coping strategies (Owen, Klapow, Roth, Shuster, Bellis, Meredith & Tucker, 2005) weight loss in chemotherapy (Kumar, 2001) and self administered alternative medicines (Bennett, Montgomery, Steinberg, & Kulp (2004) among others. Trainees later worked as therapists under the supervision of an advanced postgraduate licensed assistant and the program's principal investigator.
Setting and procedure
Patients were recruited in the hospital's waiting rooms and/or in the medical offices, on the basis of their acceptance to participate in the project. They first listened to a general description of the program with emphasis on the role of behavioral and psychological factors in cancer treatment and the potential benefits of participating. In accordance to ethical requirements potential participants were also assured that they could drop out from participation at any time with no negative consequences whatsoever. Therapists also described potential benefits of participating, and offered additional counseling after completion of the project's protocols should the patient request so.
Once recruited through granting their informed consent, patients were assigned to a session schedule to be held in one of three specific office spaces temporarily assigned to the project in the hospital. In exceptional cases sessions were conducted in the patient home depending on medical conditions (such as surgery recovery) or having difficulty transporting themselves to the hospital. In order to facilitate appointment compliance the distribution of sessions was adjusted, whenever possible, to the patients medical visits and/ or her transportation needs.
Patient self–recording training
During the initial sessions patients and one accompanying relative, if one was available, were trained in the use of the self recording booklet, including independent reliability checks. Training consisted in a detailed description of each behavioral category with its respective printed pictogram. It also detailed the self–recording methods by describing specific procedures and providing concrete examples relating to the patient herself, on an actual booklet. At the end the therapist asked them to make a sample recording by simply ticking the appropriate space, on the basis of a short series of verbally described sample vignettes.
Patients were then given one or several self–recording booklets enough for the number of days until the next hospital appointment, and instructed to record their behavior for as many days as were in such interval. Specific clear–cut directions instructed both patients and caregivers not to communicate in any form during the recordings of the reliability checks and not to copy or alter any record. In order to reduce the possibility of therapist–induced biases, patients were commended for completing self recordings without mention of inter–observer agreement.
Clinical procedures
During the first intervention session, after collecting the corresponding self–recording booklets the therapist explored the patient's knowledge on her condition and exposed her to a standard four–page text on breast cancer with emphasis on relevant behavioral aspects. The text was expressly designed for the project and was prepared in very simple Spanish. If the patient could not read, the therapist read, explained and exemplified the text contents in everyday terms and invited questions. The therapist then explained the rationale behind three terapeutic goals: a) the establishment of behaviors aimed at supporting the medical treatment, b) the modification of private verbal events incompatible with such support or with stable/positive emotional responses, and c) the acquisition of self–regulating skills to facilitate such responses. Patients were also told that further questions and queries would be welcome at any time during treatment. Once initial questions had been answered the therapist explained the behavior therapy general plan and, if time allowed so, started specific interventions.
The procedures toward the establishment of specific healthcare behaviors and skills followed the problem–solving line of Safren, Otto, Worth, Salomon, Johnson, Mayer & Boswell (2001); Nezu, Palmatier & Nezu (2004) and D'Zurilla, Nezu & Maydieu–Olivares (2004). Thus therapists would go over a list of adherence problems and possible solutions titled "Pasos vitales" (Life steps) (Safren, Otto & Worth, 1999). For each identified problem the therapist analyzed, together with the patient the viability of possible solutions and swayed the patient to put them into practice. The main actions addressed included: showing up for appointments, asking questions to physicians and nurses, obtaining and properly storing medications, tolerating medication side effects, taking medications on time, and personal hygiene and grooming care.
The intervention procedures related to detecting and shifting verbal private events was conducted along the lines of both traditional procedures aimed at altering appraisal patterns (Brewin, 1996) and those of Functional Analytic Psychotherapy (Kanter, Landes, Busch, Rusch, Brown & Baruch, 2006; Kohlenberg, Kanter, Bolling, Parker & Tsai, 2002; Vandenberghe, 2008). Thus, when a patient verbalized one such event, as exemplified in the introduction of the present paper, the therapist either challenged its plausibility directly or conducted a question–answer exercise leading the patient to develop any or both of two conclusions: how unreasonable or groundless the statement was, and how it could stand in the way of progress on behalf of her wellbeing and medical treatment. Also, if the patient made a verbal description how she had managed to achieve engaging in one or more of the desired behaviors in her own context, immediate and unambiguous verbal recognition and praise by the therapist followed.
Finally, the main procedure aimed at diminishing the physiological correlates of anxiety included training on diaphragmatic breathing and deep progressive muscle relaxation (Fahrion & Norris, 1990; Lehrer, 1996). After explaining the link between anxiety and physiological muscle tension in simple terms, the therapist prompted the patient to sit comfortably, loosen up clothes, etc. and imitate the therapist modeling of diaphragmatic breathing. This involved taking a deep breath and monitoring the diaphragmatic component by either having the patient place a hand on her abdomen or positioning her fingertips along the lower edge of her ribs. She was then instructed to make sure each breath pushed up or outward her hand or fingertips. During patient practice, therapists used slow–paced phrases to mark a steady and deep breathing rhythm. These phrases included describing breathing as deep, slow (approximately eight seconds from the start of inhaling to finishing exhaling), "from the stomach" and comfortable, as well as commending the patient for her progress. Once this routine was mastered patients were asked to leave diaphragmatic breathing "as a constant background" during the remainder of the relaxation excersises.
Once the therapist described and modelled the tensing–relaxing contrast patients were successively instructed to tense for five seconds (counted out–loud by the therapist) and then relax specific muscle groups. This alternating tension–relaxation procedure included the folloing sequence: forehead, cheeks, lips, jaw, neck, shoulders, arms, hands, abdomen, buttocks, legs, ankles and feet.
At the end of each session the therapist assigned tasks to be performed at home by the patient and those acting as primary caregivers. In these cases, relatives assisted also by carrying out reliability checks. As an attempt to control for experimenter biases, therapist training included specific instructions to abide by the intervention protocols as described above and avoid any verbal interaction with the patients or their relatives that might spuriously induce behavioral or verbal changes.
RESULTS
Reliability
Each therapist and two additional experimentally naive assistants transferred and double checked all recordings into a database for a total of six patients who had completed at least the posttest measures. Reliability was computed by dividing agreements by agreements plus disagreements for the total of opportunities provided for data recording in the self recording booklets and those collected for reliability and then multiplied by 100, and it was assessed for all (100%) such available booklets. Reliability resulted in the following percent agreement for the corresponding behaviors: 65.8% for appropriate diet, 85.0% for physical exercise, 85.8% for performance at work, 69.8% for deep muscle relaxation, 96.6% for sexual encounters, 75.2% for time with friends, 88.6% for recreation, 95.0% for hygiene/body care, 69.4% for risky behaviors and 86.2% for emotional reactions. Reliability analysis was also conducted for the specific subset of emotional reactions yielding: 90.6% for sad, 84.6% for cheerful, 79.2% for angry and 89.8% for anxious.
Changes in Behaviors and Emotions
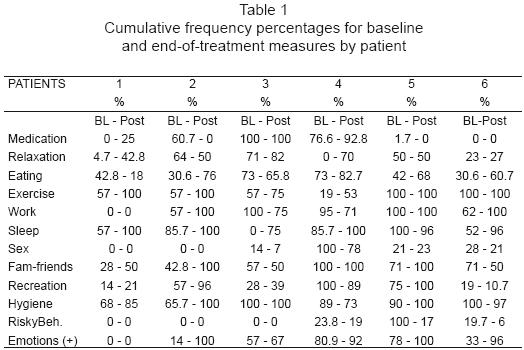
Table 1 shows the percentage for the cumulative frequencies of behavior recorded for a total of 72 prescribed sets of opportunities to display the appropriate behavior/emotion (six patients times twelve categories). Change occurred in the direction of clinical improvement in 56 out of 72 sets of opportunities (77.8%). The categories showing the largest positive change included exercising, spending time with family and friends, reduction of risky behaviors, positive emotional reactions and repairing–refreshing sleep. Those showing the smallest improvement included sexual activity, performing at work or in home chores, and recreation.
DISCUSSION
The purpose of the present study was twofold: first, to test the viability of using a behavioral self–recording procedure specifically designed for breast–cancer patients, and probe its utility and reliability with participants with little or no schooling. Second, to explore in a preliminary fashion changes in behaviors aimed at both, supporting the medical treatment of breast cancer and reducing distress related to the condition and to its treatment.
Regarding reliability, eight out of twelve behavioral categories yielded percentages of 80% or higher, two were marginal (deep muscle relaxation and time spent with friends and family) and two showed agreement percentages between 65 and 70 percent (risky behaviors and appropriate eating). Reliability on emotional reactions showed one marginal reading of 79.2% (angry) and the remainder ranged from 82.7% to 90.6%.
In general, data point in the direction of a useful, practical and reliable behavioral self–recording procedure. The fact that some specific behavioral categories yielded lower reliability data deserves some comment. It was interesting to observe, for example, that it was risky behaviors such as smoking the ones frequently noted in the treatment binnacles as behaviors which patients tended to do in relative hiding or seclusion. This would naturally represent a difficulty during independent reliability checks since patients would try not to let their caregiver observe it, and the same would probably apply to other risky behaviors such as eating inappropriate foods, especially when the patients did not have meals while someone else (namely the reliability observer) was present.
Regarding behavioral change, most pre–post measure comparisons yielded change in the direction required to support patient therapeutic adherence and reduce distress. The preliminary exploration of such effects was only a secondary purpose of the present study, thus further analysis comprising a larger number of individual replications of the effects will help ascertain a more definite set of conclusions related to clinical (or otherwise) significance of the outcomes.
In the meanwhile, these preliminary results point in the general direction of findings by other studies (see e.g., Graves, Schmidt, Bollmer, Fejfar, Langer, Blonder & Andrykowski, 2005; Shelby, Crespin, Wells–Di, Sharla, Lamdan, Siegel, & Taylor, 2008) in the sense that breast cancer patients may benefit from interventions in the areas addressed by the present study. Perhaps the most explicit contribution of the present study relates to the specificity of features in both recording materials and interventions so as to address needs of patients with low socio–economic status.
Although the likelihood of alternative explanations for clinical results tends to be always looming, the present study implemented specific procedures to reduce the probability of personal biases. It also kept specific tabs on events outside treatment which may vary simultaneously with behavioral interventions and changes. A more comprehensive analysis of complete group data is expected to shed more light on these methodological possibilities.
1 The authors are gratefully indebted to C. Arzate M. for designing and formatting the final version of the self–recording booklet; to A. E. Martínez B. for overseeing the administrative progress of the program, and to H. Cruz N., G. Escorza F., C. Garduño Z., I. Moreno B. and C. Sierra A. for their able work as therapists. The project was funded through grant IN–303907 from UNAM's office for Faculty Affairs and Research.
REFERENCES
Anagnostopoulos, F., Kolokotroni, P. Spanea, E. & Chryssochoou, M. (2006). The mini–mental adjustment to cancer (mini–mac) scale: Construct validation with a greek sample of breast cancer patients. Psycho–Oncology, 15(1), 79–89. [ Links ]
Bennett, L. M., Montgomery, J. L., Steinberg, S. M. & Kulp, K. S. (2004). Flor–Essence herbal tonic does not inhibit mammary tumor development in Sprague Dawley rats Breast Cancer Research and Treatment 88: 87–93, 2004. [ Links ]
Bower, J. E. & Segerstrom, S. C. (2004). Stress management, finding benefit, and immune function: positive mechanisms for intervention effects on physiology. Journal of Psychosomatic Research 56(1), 9–11. [ Links ]
Bradley, L. A., Johnstone, B., Hagglund, K. J., Davidson, D. M. Hutchinson, D. R., Walker, E. A. & Kelly, J. A. (2001). Behavior and disease. In D. Wedding (Ed.) Behavior and medicine (pp. 321–376). Ashland, OH: Hogrefe & Huber Publishers. [ Links ]
Brewin, C. R. (1996). Theoretical foundations of cognitive–behavior therapy for anxiety and depression. Annual Review of Psychology, 47(1), 33–57. [ Links ]
Budakoglu, I. I., Maral, I., Ozdemir, A. & Bumin, M. A. (2007). The effectiveness of training for breast cancer and breast self–examination in women aged 40 and over. Journal of Cancer Education, 22(2), 108–111. [ Links ]
Burgess, G. H., Sternberger, L. G., Sanchez–Sosa, J. J., Lunt, I., Shealy, C. N., & Ritchie, P. (2004). Development of a global curriculum for professional psychology: Implications of the combined–integrated model of doctoral training. Journal of Clinical Psychology, 60(10), 1027–1049. [ Links ]
Burish, T.G., Shartner, C. D. Lyles, J. N. (1981). Effectiveness of multiple muscle–site EMG biofeedback and relaxation training in reducing the aversiveness of cancer chemotherapy. Biofeedback Self Regulation.1981 Dec; Vol. 6 (4), pp. 523–35. [ Links ]
Cerully, J. L., Klein, W. M. P., & McCaul, K. D. (2006). Lack of Acknowledgment of Fruit and Vegetable Recommendations Among Nonadherent Individuals: Associations With Information Processing and Cancer Cognitions. Journal of Health Communication, 11, (Suppl1), 103–115. [ Links ]
Chandra, P. S., Chaturvedi, S. K., Channabasavanna, S. M., Anantha, N., Reddy, B. K. Sharma, S. & Rao, S. (1998). Psychological well–being among cancer patients receiving radiotherapy: A prospective study. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation, 7(6), 1998, 495–500. [ Links ]
Donovan, K. A., Small, B. J., Andrykowski, M. A., Munster, P. & Jacobsen, P. B. (2007). Utility of a cognitive–behavioral model to predict fatigue following breast cancer treatment. Health Psychology, 26(4), 464–472. [ Links ]
D'Zurilla, T. J., Nezu, A. M. & Maydeu–Olivares, A. (2004). Social Problem Solving: Theory and Assessment. In: E. C. Chang, T. J. D'Zurilla & L. J. Sanna (Eds). Social problem solving: Theory, research, and training. (pp. 11–27). Washington, DC: American Psychological Association. [ Links ]
Drury, M., Harcourt, J. & Minton, M. (1996). The acceptability of patients with cancer holding their own shared–care record. Psycho–Oncology, 5(2), 119–125. [ Links ]
Fahrion, S. L. & Norris, P. A. (1990). Self–regulation of anxiety. Bulletin of the Menninger Clinic, 54(2), 217–231. [ Links ]
Falleti, M. G., Sanfilippo, A., Maruff, P., Weih, L. & Phillips, K. A. (2005). The nature and severity of cognitive impairment associated with adjuvant chemotherapy in women with breast cancer: A meta–analysis of the current literature. Brain and cognition, 59(1), 60–70. [ Links ]
Friedman, L. C., Romero, C., Elledge, R., Chang, J., Kalidas, M., Dulay, M. F., Lynch, G. & Osborne, C. K. (2007). Attribution of blame, self–forgiving attitude and psychological adjustment in women with breast cancer. Journal of Behavioral Medicine, 30(4), 351–357. [ Links ]
Garssen, B. (2004). Psychological factors and cancer development: Evidence after 30 years of research. Clinical Psychology Review, 24(3), 315–338. [ Links ]
Graves, K. D., Schmidt, J. E., Bollmer, J., Fejfar, M., Langer, S., Blonder, L. X. & Andrykowski, M. A. (2005). Emotional expression and emotional recognition in breast cancer survivors: A controlled comparison. Psychology & Health, 20(5), 579–595. [ Links ]
Greer, S. (2008). CBT for emotional distress of people with cancer: Some personal observations. Psycho–Oncology, 17(2), 170–173. [ Links ]
Hamilton, S. B. & Bornstein, P. H. (1977). Increasing the accuracy of self–recording in speech–anxious undergraduates through the use of self–monitoring training and reliability enhancement procedures. Journal of Consulting and Clinical Psychology, 45(6), 1076–1085. [ Links ]
Hernandez–Guzman, L. & Sanchez–Sosa, J. J. (2005). Quality assurance of professional psychology education in Mexico [El aseguramiento de la calidad de los programas de formación en psicología profesional en México]. Revista Mexicana de Psicologia, 22(3), 271–286. [ Links ]
Horne, R. & Weinman, J. (1999). Patient's beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. Journal of Psychosomatic Research, 47, 555–567. [ Links ]
Hotz, S., Kaptein, A., Pruitt, S., Sanchez–Sosa, J. J. & Willey, C. (2003). Behavioural mechanisms explaining adherence: What every health professional should know. In: E. Sabate (Ed.) Adherence to long term therapies: Evidence for action (pp. 135–149). Geneva: World Health Organization. [ Links ]
Izdebski, P. (2007). The role of personality and temperamental factors in breast cancer: A 5–year prospective examination. Polish Psychological Bulletin, 38(4), 198–205. [ Links ]
Kanter, J. W., Landes, S. J., Busch, A. M., Rusch, L. C., Brown, K. R. & Baruch, D.E. (2006). The Effect of Contingent Reinforcement on Target Variables in Outpatient Psychotherapy for Depression: A Successful and Unsuccessful Case Using Functional Analytic Psychotherapy. Journal of Applied Behavior Analysis, 39(4), 463–467. [ Links ]
Kazdin, A. E. (1982). Single case research designs: Methods for clinical and applied settings. New York: Oxford University Press. [ Links ]
Kim, K.S., Lee S.W., Choe, M. A., Yi, M.S., Choi, S. & Kwon S.H. (2005). Effects of abdominal breathing training using biofeedback on stress, immune response and quality of life in patients with a mastectomy for breast cancer. Taehan Kanho Hakhoe Chi, 35(7), 1295–303. [ Links ]
Kohlenberg, R. J., Kanter, J. W., Bolling, M. Y., Parker, C. R. & Tsai, M. (2002). Enhancing cognitive therapy for depression with functional analytic psychotherapy: Treatment guidelines and empirical findings. Cognitive and Behavioral Practice, 9(3), 213–229. [ Links ]
Kumar, N. B. (2001). Weight Gain in Breast Cancer Patients on Chemotherapy: Exploring Hormonal, Body Composition and Behavior Mechanisms. Research Report: U.S. Army Medical Research and Materiel Command. Fort Detrick, Maryland 21702–5012. [ Links ]
La Vecchia, C. & Bosetti, C. (2005). Cancer mortality in Latin America: implications for prevention. Pan American Journal of Public Health, 18(1), 1–4. [ Links ]
Lee, S. W. & Piersel, W. C. (1989). Reliability and reactivity of self–recording by preschool children. Psychological Reports, 64(3), 747–754. [ Links ]
Lehrer, P. M. (1996). Varieties of relaxation methods and their unique effects. International Journal of Stress Management, 3(1), 1–15. [ Links ]
Levy, S. M., Herberman, R. B., Lippman, M. & d'Angelo, T. (1987). Correlation of stress factors with sustained depression of natural killer cell activity and predicted prognosis in patients with breast cancer. Journal of Clinical Oncology. 5, 348–353. [ Links ]
Lipinski, D. P., Black, J. L., Nelson, R. O. & Ciminero, A. R. (1975). Influence of motivational variables on the reactivity and reliability of self–recording. Journal of Consulting and Clinical Psychology, 43(5), 637–646. [ Links ]
Lipinski, D. P. & Nelson, R. O. (1974). The reactivity and unreliability of self–recording. Journal of Consulting and Clinical Psychology, 42(1), 118–123. [ Links ]
McDaniel, J. S., Musselman, D. L., Porter, M. R., Reed, D. A. & Nemeroff, C. B. (1995). Depression in patients with cancer: Diagnosis, biology, and treatment. Archives of General Psychiatry, 52(2), 89–99. [ Links ]
Miaskowski, C., Dodd, M. J., West, C., Paul, S. M. & Tripathy, D. (2001). Lack of adherence with the analgesic regimen: a significant barrier to effective cancer pain management. Journal of clinical oncology, 19, 4275–4279. [ Links ]
Mishel, M. H., Germino, B. B., Gil, K. M., Belyea, M., Carlton–Laney, I., Stewart, J., Porter, L. & Clayton, M. (2005). Benefits from an uncertainty management intervention for african–american and caucasian older long–term breast cancer survivors. Psycho–Oncology 14(11), 962–978. [ Links ]
Morrow, L. W., Burke, J. G. & Buell, B. J. (1985). Effects of a self–recording procedure on the attending to task behavior and academic productivity of adolescents with multiple handicaps. Mental Retardation, 23(3), 137–141. [ Links ]
Nezu, C. M., Palmatier, A. D. & Nezu, A. M. (2004) Problem–Solving Therapy for Caregivers. In E. C. Chang, T. J. D'Zurilla, L. J. Sanna & J. Lawrence (Eds.) Social problem solving: Theory, research, and training (pp. 223–238). Washington, DC: American Psychological Association. [ Links ]
Owen, J. E., Klapow, J. C., Roth, D. L., Shuster, J. L., Bellis, J., Meredith, R. & Tucker, D. C. (2005). Randomized pilot of a self–guided internet coping group for women with early–stage breast cancer. Annals of Behavior Medicine, 30(1), 54–64. [ Links ]
Parra, N., Mazón, C., Rojas–Drummond, S. & Espinosa–Vélez, M. (2005). Efectos de un programa de fortalecimiento de habilidades de comprensión de textos en educandos de primaria [Effects of a program to promote text comprehension abilities in primary students]. Revista Mexicana de Psicología, 22(1), 91–102. [ Links ]
Perna, F. M., Craft, L. C., Charles, S. & Antoni, M. H. (2008). Negative affect and barriers to exercise among early stage breast cancer patients. Health Psychology, 27(2), 275–279. [ Links ]
Piña López, J. A., Dávila Tapia, M., Sánchez–Sosa, J.J., Togawa, C. & Cázares–Robles O. (2008). Association between stress and depression levels, and treatment adherence in HIV–positive persons in Hermosillo, Mexico [Asociación entre los niveles de estrés y depresión y la adhesión al tratamiento en personas seropositivas al VIH en Hermosillo, México. Pan American Journal of Public Health [Revista Panamericana de Salud Pública, 23(6), 377–383. [ Links ]
Pojoga, C. (2001). Quality of life and breast cancer: A review from a behavioral medicine point of view. Romanian Journal of Cognitive and Behavioral Psychotherapies, 1(1), 57–70. [ Links ]
Quesnel, C., Savard, J., Simard, S., Ivers, H. & Morin, C. M. (2003). Efficacy of Cognitive–Behavioral Therapy for Insomnia in Women Treated for Nonmetastatic Breast Cancer. Journal of Consulting and Clinical Psychology, 71(1), 189–200. [ Links ]
Rabin, C. & Pinto, B. (2006). Cancer–related beliefs and health behavior change among breast cancer survivors and their first–degree relatives. Psycho–Oncology, 15(8), 701–712. [ Links ]
Richardson, J., Shelton, D., Krailo, M. & Levine, A. (1990). The effect of compliance with treatment on survival among patients with hematologic malignancies. Journal of Clinical Oncology, 8(1), 356–364. [ Links ]
Rooney, M. & Wald, A. (2007). Intervention for the management of weight and body composition changes in women with breast cancer. Clinical Journal of Oncology Nursing, 11(1), 41–52. [ Links ]
Safren, S. A., Hendriksen, E. S., Desousa, N., Boswell, S.L. & Mayer, K. H. (2003). Use of an on–line pager system to increase adherence to antiretroviral medications. AIDS Care, 15(6), 787–793. [ Links ]
Safren, S. A., Otto, M. W. & Worth, J. L. (1999). Life–steps: Applying cognitive behavioral therapy to HIV medication adherence. Cognitive and Behavioral Practice, 6(4), 332–341. [ Links ]
Safren, S. A., Otto, M. W., Worth, J. L., Salomon, E., Johnson, W., Mayer, K. & Boswell, S. (2001). Two strategies to increase adherence to HIV antiretroviral medication: Life–steps and medication monitoring. Behaviour Research and Therapy, 39(10), 1151–1162. [ Links ]
Sanchez–Sosa, J. J. (2007). Psychotherapy in Mexico, practice, training and regulation. Journal of Clinical Psychology, In Session, 63(8), 765–771. [ Links ]
Shelby, R. A., Crespin, T. R., Wells–Di, G., Sharla M.; Lamdan, R. M., Siegel, J. E., & Taylor, K. L. (2008). Optimism, social support, and adjustment in African American women with breast cancer. Journal of Behavioral Medicine, 31(5), 433–444. [ Links ]
Spiegel, D., Bloom, J. R., Kraemer, H. C. & Gottheil, E. (1994). Effect of psychosocial treatment on survival of patients with metastatic breast cancer. In A. Steptoe & J. Wardle (Eds.) Psychosocial processes and health: A reader (pp. 468–477). New York: Cambridge University Press. [ Links ]
Stanton, A. L. & Reed, G. M. (2003). Coping with treatment side effects. In: A. L. Stanton & G. M. Reed (Eds.) The breast cancer notebook: The healing power of reflection. (pp. 79–96). Washington, DC, US: American Psychological Association. [ Links ]
Teas, J., Davis, J.., Raghavan, S.,Oman, L., & Nitcheva, D. (2003). Do the Effects of Exercise on Breast Cancer Prevention Vary With Environment. Research Report: US Department of Defense Defense Technical Information Center U.S. Army Medical Research and Materiel Command. Fort Detrick, Maryland 21702–5012. [ Links ]
Vandenberghe, L. (2008). Culture–sensitive functional analytic psychotherapy. The Behavior Analyst, 31(1), 67–79. [ Links ]
Wan, C., Zhang, D., Tang, X., Zhang, W., Li, W., Ren, H., He, R. & Wang, W. (2003). Revision of the Chinese version of the FACT–B in patients with breast cancer. Chinese Mental Health Journal, 17(5), 298–300. [ Links ]
Wilkins, E. G. (1998). The Michigan Breast Reconstruction Outcome Study. Research report U.S. Army Medical Research and Materiel Command, Fort Detrick, Maryland 21702–5012. [ Links ]
Yan. L., Wenjuan, L., Xinfan, L., Gigang, Z., Hardy, E. & Mountainbear, M. (2001). The effect of psycho–behavioral intervention on the emotional reaction and immune function in breast cancer patients undergoing radiotherapy. Acta Psychologica Sinica, 33(5), 437–441. [ Links ]














