INTRODUCTION
The COVID-19 pandemic, declared by the World Health Organization in March 2020, has wreaked unprecedented havoc and difficulties in the quality and development of human life, impacting cultural, political, economic, social, physical, and mental (Gloster et al., 2020).
The closure of educational institutions to reduce the transmission of COVID-19 puts education at risk and damages the mental health of millions of children and young people (Caldera-Villalobos et al., 2020; O’Byrne, Gavin, & McNicholas, 2020; Sanchez, Peña, & Ng, 2020). Recent international reports show that during the pandemic, 26 and 40% of university students show symptoms of anxiety, 21.6% of depression and up to 84% of students show stress (Lai et al., 2020; Lasheras et al., 2020; Ramón-Arbués et al., 2020).
Moreover, these restrictions predispose to feelings of loneliness, despair, and dysfunction in emotional regulation that may lead to alcohol consumption and abuse (Alsoufi et al., 2020; Chodkiewicz, Talarowska, Miniszewska, Nawrocka, & Bilinski, 2020; Meo, Abukhalaf, Alomar, Sattar, & Klonoff, 2020; Testino, 2020; Killgore, Cloonan, Taylor, Lucas, & Dailey, 2021). In this respect, people with depression or anxiety comorbidity with alcohol dependency, up to 70% (Pitchot & Dor, 2019). Among medical students, the prevalence of alcohol use is high, ranging between 66% and 97% (Coker, Coker, & Sanni, 2018; Freire, Castro, & Petroianu, 2020). This has been linked to absenteeism, school dropout, learning difficulties, poor academic performance, and other psychiatric disorders (Freire et al., 2020). As well as high rates of unemployment, social conflicts, domestic violence, and legal penalties (Soares, Farias, & Monteiro, 2019; Witkiewitz, Litten, & Leggio, 2019; Nasui et al., 2021).
Mindfulness-Based Intervention programs (MBI) employ mindfulness techniques in the present moment. Some research has shown that MBI is effective in reducing stress, anxiety, and depression by up to 41% in different types of populations, including university students (Sancho et al., 2018; Huberty et al., 2019). However, it reports that MBIs have low compliance rates and high dropout rates, which reduces their effectiveness (Danilewitz et al., 2018). On the other hand, with the restrictions on physical interaction due to the COVID-19 pandemic, the online MBI application may be an alternative strategy to prevent the development of psychopathologies and alcohol consumption among students (Farris et al., 2021). Morledge et al. (2013) conducted a randomized controlled trial of an online MBI and found a significant reduction in stress levels in medical students. Nevertheless, the research evaluating the effectiveness of online MBIs on psychopathologies and alcohol consumption is still recent; little is known about the factors that might influence the effectiveness of such interventions.
To prevent and improve the mental health conditions of the student population, as well as to propose and refine cost-effective and flexible intervention strategies in their application, this study aimed to evaluate the effectiveness of the online MBI on mental health and alcohol consumption in medical students during the COVID-19 pandemic.
METHOD
Study design and subjects
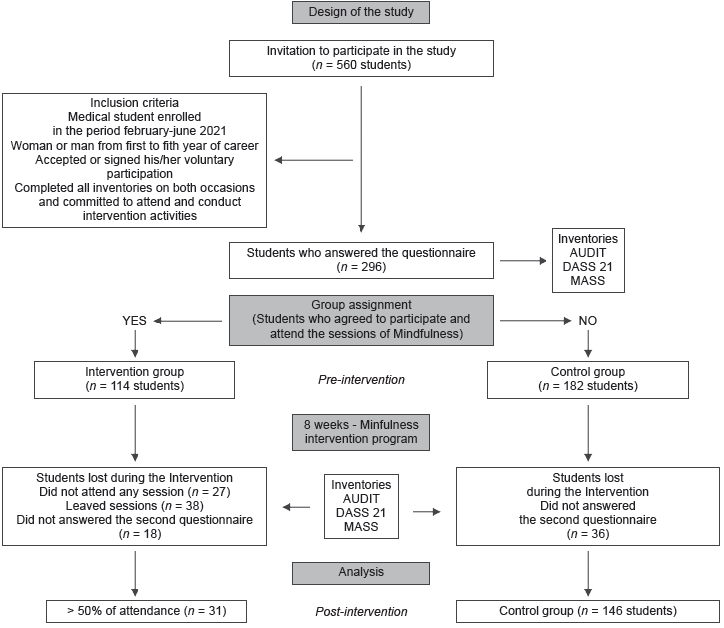
A longitudinal, quasi-experimental, interventional study was carried out on medical students at the University of Veracruz, Minatitlán campus, in March-July 2021. Was used a non-probabilistic sample of medical students invited of both sexes (n = 560), from the first to the fifth year of the degree, who had accepted and signed their voluntary participation in the study, and who answered completed pre- and post-intervention inventories. Students under psychiatric/psychological treatment or who wanted to drop out of the intervention were excluded and eliminated.
Measurements
Sociodemographic Questionnaire
A questionnaire was applied to collect sociodemographic data that included: sex, age, school semester, school grades, family characteristics, health, hygiene measures, isolation, activities, hobbies, perception of the situation, and online classes, as well as nutritional quality and sleeping time during the pandemic.
Depression, Anxiety, and Stress Scale - 21 (DASS-21)
The DASS-21 is a set of three self-report scales designed to measure the emotional states of depression, anxiety, and stress (Zanon et al., 2021). Each of the three DASS-21 subscales contains seven items, scored from 0 to 3, added up, and interpreted separately. In the data analysis, we used cut-off scores established by Román, Santibáñez, and Vinet (2016) to identify youth at risk of mental health problems.
Alcohol Use Disorders Identification Test (AUDIT)
This test was applied to identify people with patterns of risk of alcohol harm. It has three evaluation domains, consisting of 10 items in total. The first three items: evaluate risky drinking (8-15 points) with questions aimed at knowing the frequency of drinking; items 4 to 6 determined the symptoms of dependence (from 16 to 19 points), looking for data on loss of control over drinking; and questions 7 to 10, evaluate the high-risk of alcohol consumption (from 20 points or more), with questions about the sense of guilt and alcohol abuse consequences (Kamboj et al., 2017; Wielgosz, Goldberg, Kral, Dunne, & Davidson, 2019; Shuai, Bakou, Hardy, & Hogarth, 2020).
Mindfulness Attention Awareness Scale test (MASS)
This instrument measures the frequency of the state of dispositional mindfulness in daily activities without the need for prior training, that is, the open or receptive awareness of attention to what is happening in the present. It consists of 15 items that score individually from 1 to 6. The total score is a result of the arithmetic mean of all items: where high scores indicate a higher level of attention fully and consciously (Schuman-Olivier et al., 2020).
Procedure
The dissemination project and its objectives were addressed to the university medical students through social networks (Facebook and WhatsApp), employing infographics and posters. Subsequently, the first assessment (pre-intervention): was determined using a digital form in Google Forms, where the levels of symptoms of stress, anxiety, and depression were measured using the DASS-21 scale, as well as the high risk of alcohol consumption using the AUDIT. Finally, we used the MASS scale to determine the student's level of the state of dispositional mindfulness.
Subsequently, the online MBI was performed: for eight sessions supervised by a psychologist, one session every week, lasting approximately one to two hours, using the Zoom platform. Finally, the efficacy of the MBI on the symptomatology of stress, anxiety, depression, alcohol consumption, and full awareness: was evaluated post-intervention through the same inventories (Figure 1).
Online Mindfulness-Based Intervention programs (MBI)
The online MBI was taught in eight sessions, lasting approximately one to two hours, once a week, using the virtual platform Zoom, consisting of group meditation guided and supervised by an expert psychologist. The content of each session was based on: relaxation techniques, breathing, movement meditation, guided meditation, single-pointed focus meditation, formal meditation, informal meditation, and body scanning. Were recommended that the students were in a space large enough to perform the movements, in a comfortable posture, seated and with a straight back, preferably wearing comfortable clothing. After each session, was recommended to the participants to do a series of meditation exercises, recorded in a logbook, which was reviewed in subsequent sessions to promote concentration for a longer time.
Statistical analysis
Qualitative variables were analyzed as frequencies and percentages, and quantitative variables as means and standard error. The Chi-square test and Pearson R were used to verify the association and, or correlation between dependent; and independent variables. Comparisons of psychopathologies, alcohol consumption, and sociodemographic variables were performed using Student's t statistics and dependent and independent analysis of variance (ANOVA). The tests were selected depending on normality and homoscedasticity of variance. All data were analyzed with the SPSS 25 for Mac OS (IBM Corp., Armonk, NY, USA). Were considered a 95% confidence level for all statistical tests, and p ≤ .05 as statistically significant.
Ethical considerations
The project was approved by the Ethics and Institutional Research Committee (CI-001-2021). In addition, it is subject to the General Health Law of Mexico in Articles 13, 14, 16, 20, and 36, Chapters 96, 100, and 102, and following with the Declaration of Helsinki for Medical Research Involving Human Subjects (Ley General de Salud, 1984; Asociación Médica Mundial, 2013).
RESULTS
The final sample consisted of 177 students, of which 105 (59.3%) were women and 72 (40.7%) men, with an average age of 20.8 ± .13 years (range 18 to 25 years), most with overall school grades between 8.5 and 9.0 and whose only concern was studying. Only one student (.6%) was living as a concubine, and the remainder of the students were single (99.4%). Most lived with both their parents (61.6%), and about 50% mentioned mental health problems, followed by economic issues for which they might drop out school (Table 1).
Table 1 Sociodemographic characteristics of medical students
| Frequency | Percentage | ||
|---|---|---|---|
| Sex | Women | 105 | 59.3 |
| Men | 72 | 40.7 | |
| Age (years old) | 18-19 | 43 | 24.3 |
| 20-21 | 70 | 39.5 | |
| > 22 | 54 | 30.5 | |
| Semester | 2 | 59 | 33.3 |
| 4 | 35 | 19.8 | |
| 6 | 32 | 18.1 | |
| 8 | 34 | 19.2 | |
| 10 | 17 | 9.6 | |
| School grades | 7.51 to 8.0 | 10 | 5.7 |
| 8.01 to 8.50 | 24 | 13.6 | |
| 8.51 to 9.0 | 72 | 40.7 | |
| 9.01 to 9.5 | 60 | 33.9 | |
| 9.51 to 10 | 9 | 5.1 | |
| Working status/work situation | Just study | 138 | 78.0 |
| Mainly works and also studies | 28 | 15.8 | |
| Studies and also looking for work | 11 | 6.2 | |
| Reasons to drop out school | Neither or does not apply | 89 | 50.3 |
| Physical health problems | 4 | 2.3 | |
| Mental health problems | 41 | 23.2 | |
| Economic problems | 30 | 16.9 | |
| Family problems | 7 | 4.0 | |
| Other | 6 | 3.4 | |
| Family conformation | Married parents live together | 109 | 61.6 |
| Married parents live separately | 13 | 7.3 | |
| Divorced parents | 23 | 13.0 | |
| Single mother | 16 | 9.0 | |
| Widowed father/mother | 6 | 3.4 | |
| Other | 10 | 5.6 | |
| Head of
household’s educational attainment |
Primary school | 7 | 4.0 |
| Middle school | 24 | 13.6 | |
| High school | 42 | 23.7 | |
| Bachelor’s degree | 88 | 49.7 | |
| Post-graduate education | 16 | 9.0 |
The lifestyle and routines that students had maintained during the pandemic show that 73.4% practiced social distancing, health care, and hygiene basics; additionally, about 60% of students mentioned having social interaction with people outside their family and having some hobbies. Likewise, most of them did some physical activity twice to thrice times a week for no longer than one hour. In addition to 39.7% of students reported having poor or regular sleep quality, sleeping less than six hours a day (Table 2).
Table 2 Habits and lifestyles during the pandemic of medical students
| Frequency | Percentage | ||
|---|---|---|---|
| Current situation at home | Does not apply isolation, social dis- tancing, or basic healthcare mea- sures |
1 | .6 |
| Only basic healthcare measures | 9 | 5.1 | |
| Social distancing and basic health- care measures |
130 | 73.4 | |
| Strict home isolation | 37 | 20.9 | |
| Social interaction | No | 67 | 37.9 |
| Yes | 110 | 62.1 | |
| Hobby | No | 67 | 37.9 |
| Yes | 110 | 62.1 | |
| Physical activity | No | 77 | 43.5 |
| Yes | 100 | 56.5 | |
| Time spent on
physical activity |
Neither or does not apply | 77 | 43.5 |
| < 1 hour | 73 | 41.2 | |
| 1-2 hours | 11 | 6.2 | |
| > 2 hours | 16 | 9.0 | |
| The weekly amount
of physical activity |
Neither or does not apply | 77 | 43.5 |
| 1-2 times per week | 17 | 9.6 | |
| 3-4 times per week | 46 | 25.9 | |
| > 4 times per week | 37 | 20.9 | |
| Sleep quality | Bad | 69 | 38.9 |
| Regular | 80 | 45.2 | |
| Good | 28 | 15.8 | |
| Hours of sleep | 1-3 hours | 15 | 8.5 |
| 4-6 hours | 127 | 71.8 | |
| 7-8 hours | 29 | 16.4 | |
| > 8 hours | 6 | 3.4 | |
| Nutritional quality | Bad | 25 | 14.1 |
| Regular | 63 | 35.6 | |
| Good | 89 | 50.3 |
On the other hand, it was observed that about 29% of the students were not afraid of SARS-CoV-2 infection, however, 31.6% reported being afraid of the transmission. In addition, 69.5% said they were afraid that a family member would die from COVID-19 and about 30% were afraid of returning to face-to-face classes (Figure 2A). Regarding the perception of taking online classes during the pandemic, most of the medical students considered their experience, learning, academic performance, and relationship with teachers as “regular”, while their relationship with classmates was considered mostly “good” (Figure 2B). Finally, 13.1% of the students indicated having thought about suicide.
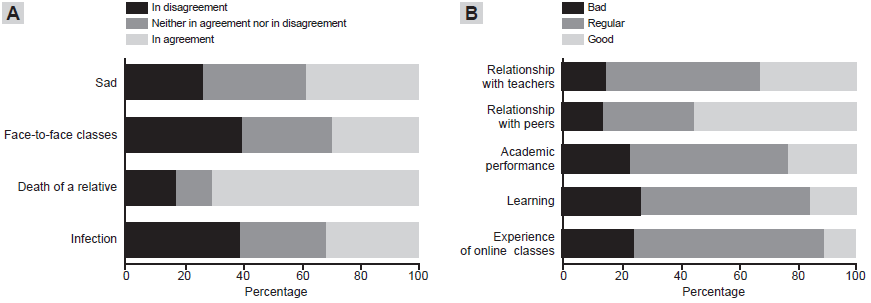
Figure 2 A) Students’ perception of the situation and the fears they face during the pandemic. B) Studentsʼ perception of the experience of taking online classes during the pandemic.
By the end of the MBI was observed that 31 (17.5%) students attended more than four sessions, and 146 (82.5%) did not attend any sessions. When comparing pre- and post- MBI values, no significant differences were observed in any variable between the previously established groups. On the contrary, when comparing pre- and post- MBI values, the group that did not attend any session showed significant changes in most of the variables, except AUDIT. In contrast, the group that assisted more than 50% of the MBI sessions did not show significant differences in any variable (Table 3).
Table 3 Comparative analysis between the groups that attended or not the sessions of MBI
| Not attended (n = 146) | Attended to > 50% of sessions (n = 31) | ||||
|---|---|---|---|---|---|
| Pre-MBI | Post- MBI | Pre-MBI | Post- MBI | ||
| AUDIT | 2.527 ± .297 | 2.472 ± .266 | 2.548 ± .474 | 2.283 ± .520 | |
| Stress | 6.932 ± .423 | 4.199 ± .384 | 7.516 ± .689 | 5.581 ± 1.004 | |
| *Wilcoxon = -4153, p < .001 | |||||
| Depression | 5.411 ± .432 | 3.336 ± .370 | 5.839 ± .994 | 4.355 ± .805 | |
| *Wilcoxon = -3130, p < .001 | |||||
| Anxiety | 4.925 ± .393 | 2.822 ± .324 | 5.419 ± .917 | 4.581 ± .931 | |
| *Wilcoxon = -3191, p < .001 | |||||
| MASS | 59.58 ± 1.425 | 65.12 ± 1.529 | 62.68 ± 3.291 | 64.03 ± 3.318 | |
| *Wilcoxon = 2431, p = .015 | |||||
*Significant intra-group differences between pre- and post-MBI scores, analyzed with the Wilcoxon sign range test. No intergroup differences were observed in any variables.
Elevated levels of stress, anxiety, depression symptoms, and alcohol consumption were associated with: the experience of taking online classes, poor sleep quality, poor perception of academic performance, their learning, relationship with teachers and peers, less physical activity, thoughts of dropping out of medical school, increased measures of social distancing and health care, and hygiene basics.
Besides that, it observed that students with higher levels of anxiety and stress symptomatology presented a higher attendance at the MBI sessions (supplementary table). In addition, about 20% of the students who showed high-risk alcohol consumption had considered suicide and dropped out of medical school during the pandemic.
In the MASS inventory, lower scores were associated: with non-attendance at MBI sessions. Conversely, higher scores were positively associated with a better experience of online classes and a higher educational level of the head of household (X2 = 22.635, p = .031), where higher levels of education were associated with higher levels of concentration (supplementary table).
Other variables such as gender, school grades, nutritional quality, number of people at home, having a hobby, fear of COVID-19, and fear of death of a family member caused by COVID-19, fear of returning to face-to-face classes, among others were not associated with the symptomatology of stress, anxiety, depression, and alcohol consumption.
DISCUSSION AND CONCLUSION
The findings in this study showed that the online MBI was not effectiveness on stress symptomatology, anxiety, depression, alcohol consumption, or mindfulness in medical students. Those could be associated: with the size sample, the high levels of psychopathology of the participants at the beginning of the intervention, the high dropout rate, and the low voluntary participation.
In this regard, in a recent review, the authors analyzed ten studies of Mindfulness intervention in medical students indicating that these interventions did not produce significant reductions in the levels of stress, anxiety, or depression, compared to the groups without intervention (Sekhar et al., 2021) which is consistent with the results obtained in this research. It has also been reported, that the lower effectiveness of the MBIs is due to small sample sizes, high dropout rates from the program, the timeframe implemented intervention, and the lack of participation, commitment, and development of the activities during the sessions (Chmielewski, Łoś, & Łuczyński, 2021) characteristics observed in this study.
Likewise, the lack of reduction in the psychopathologies levels after the MBI could be associated with: the severity of the symptoms presented by the students who attended the sessions since they showed elevated symptomatology (severe or extreme) in the indicators of stress, anxiety, and depression before the intervention, compared to those who did not attend. These findings suggest that the practice of Mindfulness may have limitations in subjects with some psychological disorders (Schuman-Olivier et al., 2020). Similarly, despite the great popularity that MBIs have recently gained, a recent meta-analysis revealed the low or almost null effectiveness of this type of intervention on emotional problems (anxiety and depression) in young students (Zenner, Herrnleben-Kurz, & Walach, 2014), which is consistent with the results obtained in this study.
On the contrary, it was observed on an intra-group level that individuals who did not attend the MBI showed reduced levels of psychopathology and an increase in mindfulness between the first and second measurements. Those could be due to the timeframe or date when the questionnaires were applied (Puig-Lagunes, Vargas-Álvarez, Salinas-Méndez, Ricaño-Santos, & Puig-Nolasco, 2020). Other papers suggested: that the timeframe of the study is crucial, as it may bias the results on the effectiveness of the MBIs (Godara et al., 2021) and a similar situation occurred in the present study, where the first measurement was performed in May when students were in the final evaluations and could present high levels of psychopathologies, while the second measurement was carried out near the vacation period when there was a less academic load.
On the other hand, although the mental health needs of medical students are evident, they are reluctant to seek treatment and to use psychological care services (Rodriguez, Corse, & Rosen, 2017), the main barriers to seeking them are: the feeling that their problems are not important, economic costs, the concern that nobody understands them, and the lack of time due to their rotations and extensive study schedules (Arenas-Monreal, Hernández-Tezoquipa, Valdez-Santiago, & Bonilla-Fernández, 2004; Givens & Tjia, 2002; Rodriguez et al., 2017), this, at the same time, decreases their autonomy and willingness to participate in sports, hobbies and social life, negatively affecting the balance of work life, family life and self-care (Arenas-Monreal et al., 2004; Picton, 2021).
It has been reported that some medical students underestimate other areas of health and the effectiveness of non-medical treatments such as psychotherapy, reducing their voluntary approach and attachment to interventions (Constantinou, Georgiou, & Perdikogianni, 2017). Moreover, most students ignore conventional healthcare routes, formal consultations, promoting self-diagnosis, and peer counseling, with whom they can take informal treatments that, in most cases, are inefficient (Gold, Johnson, Leydon, Rohrbaugh, & Wilkins, 2015; Thistlethwaite, Quirk, & Evans, 2010).
Likewise, there has been reported significant concern about the use of mental health services by students due to the fear of losing the confidentiality of any diagnosis of an emotional problem (Givens & Tjia, 2002; Gold et al., 2015; Rodriguez et al., 2017), as it may represent a danger to their academic record, for the stigma of using mental health services, since students who receive psychological counseling are less likely to obtain residency positions (Givens & Tjia, 2002).
The foregoing is evidence of a lack of policies, programs, and spaces that promote self-care in medical schools, so it is essential to promote the development of self-care skills within these schools, so that future health professionals may be able to induce a favorable change in themselves and people (Arenas-Monreal et al., 2004), considering that some research shows that education in self-care of medical students can contribute to laying the foundation for the formation of physicians more capable of serving patients by taking care of themselves (Ayala, Omorodion, Nmecha, Winseman, & Mason, 2017; Ball & Bax, 2022).
Regarding alcohol consumption, there was no post-MBI reduction or change compared to the non-intervention group, which could be explained by a reduced number of students with high-risk alcohol consumption (8.4%) or problematic alcohol consumption (.56%). However, the prevalence of alcohol consumption observed is higher than in other reports (6.1%; Killgore et al., 2021; Pitchot & Dor, 2019). It has been reported that individuals with higher levels of alcohol consumption tend to present a more gradual or less significant reductions after IMB, presenting less effectiveness in situations of high-risk alcohol consumption (Kamboj et al., 2017; Wielgosz et al., 2019). Furthermore, the Mindfulness effects in reducing alcohol consumption are higher in subjects who also showed a reduction in emotional triggers associated with alcohol consumption (Wielgosz et al., 2019; Shuai et al., 2020) in combination with other prevention programs, or implementation of more intensive MBIs, in terms of duration, which together favor a decrease of the severity and craving to consume, and same time increase abstinence (Huberty et al., 2019; Kamboj et al., 2017; Li, Howard, Garland, McGovern, & Lazar, 2017; Schuman-Olivier et al., 2020). All of the aforementioned may be associated with the lack of reduction in alcohol consumption observed in this study.
On the contrary, the MBIs that have shown less efficacy in the treatment of alcohol consumption have in common: high dropout rates from the program, lack of participation, commitment, and development of the activities during the sessions, and small sample sizes (Witkiewitz & Bowen, 2010) therefore, it is clear that the favorable effects of Mindfulness is positively correlated between the interest of the participants, the time of participation and monitoring of the activities (Sancho et al., 2018) strengths that were not observed in this study.
In addition, many variables (e.g., suicidal thoughts, college dropout, poor relationship with teachers and peers, poor social interaction, poor sleep quality, and home background) were found associated with high levels of psychopathologies and alcohol consumption. These variables could also be restricting the effectiveness of the online MBI. These results are on par with a study conducted in 78 countries during the COVID-19 pandemic, which reported a strong association between the onset of mental health problems and the severity of the restriction measures adopted during quarantine. Likewise, important indicators such as social support and interaction, educational level, and economic-financial status are also important (Gloster et al., 2020).
About the experience of online classes, it was observed a connection with the perception of poor learning, data that are consistent with other studies, where 53.8% of medical students mentioned that the COVID-19 pandemic affected their learning, 75.7% had poor online education, 59.1% presented fear of transmission of the SARS-CoV-2 virus, and 23.5% reported sadness and hopelessness (Coker et al., 2018; Freire et al., 2020).
The results obtained in this research support and contribute to previous reports, which point out that the main factors limiting the effectiveness of online MBI is: low adherence to the program, high dropout rate, loss of interest due to poor virtual interaction, lack of time for medical students, concerns about digital privacy, stigma about psychopathologies, and lack of emotional openness (Puig-Lagunes et al., 2020; Sancho et al., 2018; Schuman-Olivier et al., 2020).
It has also been described that poor motivation to practice meditation outside of sessions, little or complete lack of response to self-report forms or logs, inability to check and count total minutes of meditation, difficulty in scheduling daily sessions, and attendance at more than one session are limitations related to attrition and lack of adherence to MBI (Walsh, Saab, & Farb, 2019; Yang, Schamber, Meyer, & Gold, 2018).
Finally, we emphasize continuing with studies that contribute to the reduced prevalence of stress, anxiety, and depression symptomatology, as well as alcohol consumption in medical students. This unfavorable context exposes the importance of informing students about the consequences of such behaviors on their physical, social, and emotional condition, as well as their academic performance and learning. It also demonstrates the importance of making the medical-student community aware of the need to seek medical and psychological help. In addition, it shows a strong need for educational institutions to implement effective programs focused on mental health and alcohol consumption in students, which can effectively detect, and early treatment of the psychopathologies exposed in this study.
For all the above, we conclude that the online MBI was not effective among the population under study, which: was evidenced by the lack of reduction in the levels of stress symptomatology, anxiety, depression, and alcohol consumption, as well as an increased absence of mindfulness. Our findings suggest that the high prevalence of psychopathologies and alcohol consumption during the COVID-19 pandemic requires the most intensive interventions, with greater adherence and participation. Therefore, we recommend implementation of courses, or workshops, about the promotion of health and wellness, the generation of strategies in which medical students are involved and complete intervention programs, as well as awareness of the short and long-term biopsychosocial consequences inherent to psychopathologies and alcohol abuse.











 text new page (beta)
text new page (beta)