Introduction
According to the International Association for the Study of Pain, pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage (IASP, 1979). This already classic definition (and its most recent version currently open to comments; Raja et al., 2020), makes it clear that pain is a multidimensional concept of three interrelated elements: 1. tissue injury and the resulting stimulation of pain receptors; 2. injury or alteration of pathways and nerve and sensory transmission mechanisms of pain stimuli; and 3. alteration of the perception and cognitive and behavioral experience of pain (Fuentes, 2020).
In this regard, the approach to pain must also be multidimensional, taking into consideration the influence of sensory, cognitive, affective, and behavioral factors in the maintenance of the painful experience and the resulting intensity of the distress and disability it causes (Dalton, Feuerstein, Carlson, & Roghman, 1994; Dehghani, Sharpe, & Nicholas, 2003; Turk & Okifuji, 2003). This becomes even more crucial in the case of chronic pain, which, unlike acute pain, with its clearly protective function, lasts for three or more months, exceeds the healing period of a tissue injury, or is associated with a chronic medical condition, whereby it loses adaptive value and causes significant levels of stress and suffering (Katz, Rosembloom, & Fashler, 2015).
A key cognitive component, as regards its relevance for the maintenance of pain and the exacerbation of emotional distress and related disability (Camacho, Anarte, & Ramírez-Maestre, 2002; Herrero, Ramírez-Maestre, & González, 2008; Esteve, Ramírez-Maestre, & López-Marínez, 2007; Janowski, Steuden, & Kuryłowicz, 2010; Ramírez-Maestre, Esteve, & López, 2008; Craig, 1984), is the perception, interpretation, or cognitive assessment of the painful experience. This is a dynamic, evaluative process whereby an individual assesses the effect that an adverse circumstance has on their well-being (primary assessment) and their ability to cope with it (secondary assessment; Lazarus & Folkman, 1984).
During the past decade, increasing attention has been paid to the measurement of this component (Meade, Wang, Lin, Wu, & Poppen, 2010; Ahmad, 2005), since it is a factor that can be modified by cognitive-behavioral psychological interventions such as adjunctive psychotherapy (Cunningham, 2000). Thus, for example, the identification and resulting modification of the perception of pain as a restrictive experience, which tends to generalize a negative perception of life (Craig, 1984), which is closely linked to depression (Herrero et al., 2008; Esteve, Ramírez-Maestre, & López-Marínez, 2007), would allow both for the reduction of distress and disability (Janowski et al., 2010; Ramírez-Maestre et al., 2008), and effective coping, adaptation to chronic pain and improve the quality of life in those suffering from it.
The Cognitive Assessment of Pain Inventory (CAI; Ramírez Maestre, Esteve Zarazagay, & López Martínez, 2008) was developed for the purpose of evaluating this construct, specifically the primary cognitive assessment of pain as loss/damage, a threat, or a challenge. It is a measure with robust theoretical bases and adequate psychometric properties in the Spanish population, and its score is regarded as a good predictor of an individual’s adaptation to chronic pain. In this regard, the purpose of this study was to adapt the CAI to Mexican Spanish and to determine its validity and reliability in Mexican patients with chronic pain.
Method
This is a cross-sectional study for psychometric validation (instrumental or process) based on a convenience sample recruited between May and August 2013, of 191 adult patients (18 years and older) with chronic pain, treated at the Pain Clinic of the Salvador Zubirán National Institute of Medical Sciences and Nutrition (Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, INCMNSZ). These patients were referred to this clinic because they had presented secondary pain due to an underlying disease (such as osteoarthritis) for three or more consecutive months.
Instruments
The Cognitive Assessment Inventory (CEI) for patients with pain (Ramírez Maestre et al., 2008) was developed within the framework of the Lazarus and Smith (1988) transactional model of stress and coping. This inventory yields three scores for different dimensions of the cognitive evaluation of pain: 1. loss or damage (nine items), 2. threat (ten items), and 3. challenge (twelve items). Its original version in Castilian Spanish contains thirty-one dichotomous items (yes = 1, no = 0), with adequate psychometric properties (damage/loss: 36% explained variance and Cronbach’s alpha = .77; threat: 33.6% explained variance and Cronbach’s alpha = .77; and threat: 35.1% explained variance and Cronbach’s alpha = .83).
The Sheehan Disability Questionnaire (Sheehan, Harnett-Sheehan, & Raj, 1996) was designed to assess functional disability in three domains: 1. work/school; 2. social life; and 3. family life. It consists of a series of three ten-point analogous visual scales (one per domain) in which the degree to which pain has affected functioning is recorded, with a sensitivity of 83% and a specificity of 69% in clinical populations.
The daily activities questionnaire for patients with chronic pain is an instrument based on section three of the Multidimensional Pain Inventory designed by Kerns, Turk, and Rudy (1985), comprising thirteen items organized into two factors related to leisure activities (nine items with a Cronbach’s alpha of .87) and social activities (four items with a Cronbach’s alpha of .86). Patients answer how often they perform each of the activities mentioned on a Likert-type scale with four response options ranging from 0 (never) to 3 (always). The total reliability of the adapted test is adequate (Cronbach’s alpha of .85).
Hospital Anxiety and Depression Scale (Zigmond & Snaith, 1983). This scale enables clinicians to validly and reliably identify two of the most common forms of psychological distress in patients with a medical illness: anxiety and depression (Herrmann, 1997). It comprises fourteen items divided into two subscales: one evaluating anxiety and the other depression (López-Alvarenga et al., 2002).
Procedure
Subjects responded in person to questions asked by a psychologist who recorded them in an ad hoc format. Sociodemographic and clinical data were obtained from medical records.
Adaptation of the CAI for Mexican patients
The methodological procedure used to adapt the CAI to Mexican Spanish was based on an initial review of the items contained in the original instrument (in Castilian Spanish), to identify potential comprehension problems. The items were subsequently submitted for consideration by a committee of five experts on psychometry and the clinical area to review the words contained in the statements to make the necessary modifications to improve comprehension. The experts considered that the original Spanish version was easy to understand and culturally appropriate for Mexican population. The version reviewed by the experts was applied to twenty chronic pain patients of both sexes to obtain feedback on comprehension, language, and relevance in the Mexican population with chronic pain.
Statistical analysis
As a construct validity test of the CAI, a confirmatory factor analysis (CFA) was performed for each type of cognitive assessment: loss, threat, and challenge. The fit of the models was evaluated through the following indices: discrepancy between chi-square and degrees of freedom (CMIN/DF), normalized fit (NFI), adjusted goodness of fit (AGFI), and root mean square error of approximation (RMSEA), with factor loadings per item expected to be greater than .40. Convergent and divergent validity were assessed using Pearson’s product-moment correlation analysis between the scores of each dimension of the CAI and those of disability, daily living activities, and anxiety and depression instruments, controlling for sex and age. Internal consistency was determined using Cronbach’s alpha coefficients for each dimension of the CAI. Finally, four levels of interpretation of the CAI were obtained considering the distribution by quartiles of the responses in the sample studied. All analyses were conducted using SPSS Statistics 19.0 and AMOS for Mac, setting p ≤ .05 as the level of statistical significance.
Results
All the patients referred to the study during the fieldwork period agreed to participate and completed all the evaluations. A total of 191 adult chronic pain patients with a mean age of 58.6 (SD = 15.3; range = 19-90) were included; 74.9% (n = 143) of the sample were women, and 54.9% (n = 105) reported living together or being married. A total of 24.6% (n = 47) cited primary school as the last grade they had completed in elementary school, followed by bachelor’s degrees (n = 38, 19.9%) and technical degrees (n = 37, 19.4%). Most reported not working (n = 143, 74.9%). The type of pain most frequently diagnosed by medical specialists was neuropathic (n = 74, 38.7%), followed by nociceptive (n = 60, 31.4%), and mixed (neuropathic and nociceptive pain operating simultaneously; n = 57, 29.8%). The average intensity of pain they presented at the time of application of the instruments was 4.62 (SD = 2.6) on a ten-point analog numerical scale (ANS).
Cultural adaptation of the CAI
As a result of the preliminary IEC test, five items were modified (Table 1).
Table 1 Modifications made to original items for their cultural adaptation
| Original item | Modification criteria | Modified item |
|---|---|---|
| 1. You think that because of the pain, your sexual relations will be worse than before. |
The wording of this item was kept. However, the order of presentation within the instru- ment was changed. It was moved to item nine because it was regarded as unsuitable as a first contact item. |
9. You think that because of the pain your sexual relations will be worse than before. |
| 14. You think that if the pain continues you will have to stop doing what you like. |
This item was changed the request of 80% of the subjects evaluated, on the grounds that it was difficult to understand and not consistent with the language used. |
14. You think that if the pain continues you will have to stop doing the things you like. |
| 18. You think that if the pain continues, you will lose your appetite |
A slight modification was made due to the fact that 70% of the population indicated problems with the wording. |
18. You think that if the pain continues, you will lose your appetite |
| 23. You think that, despite the pain, you will be able to maintain your performance at work. |
Since almost the entire sample reported not being employed at the time, the impact on the individual’s daily tasks was considered. |
23. You think that, despite the pain, you will be able to maintain your performance at work or in your everyday tasks. |
| 29. You think that, despite the pain, you will be able to continue doing what you like. |
Modified due to the requests of the sample for more colloquial language. |
29. You think that, despite the pain, you will be able to continue doing the things you like. |
Cognitive Assessment of Loss Model
The cognitive assessment of loss model with the original nine items yielded satisfactory fit indices (CMIN/DF = 1.345; NFI = .900, CFI = .971; AGFI = .931; SRMR = .049; RMSEA = .043 (Figure 1).
As one can see, item 9 obtained a low value in terms of estimated regression weight (less than .40). However, when it was eliminated, fit indices outside the desired parameters were obtained, so it was decided to keep it. In addition, two covariances between residuals were established. The result obtained was a unifactorial solution with an explained variance of 33.7%.
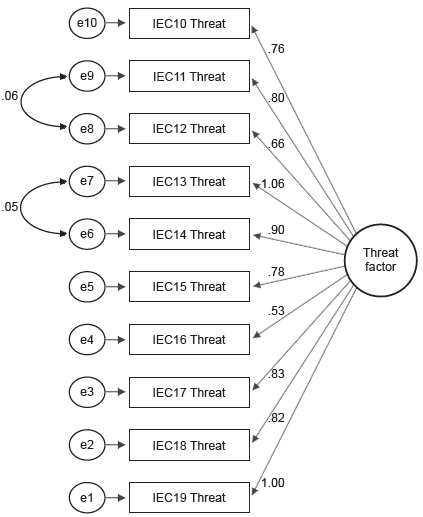
Cognitive Assessment of Threat Model
This model was also evaluated with the original number of items (ten items). The indices obtained show an adequate fit (CMIN/DF = 1.132; NFI = .935, CFI = .992; AGFI = .939; SRMR = .046; RMSEA = .026). Two covariances between residuals were established. The result obtained was a unifactorial solution with an explained variance of 40.5% (Figure 2).
Cognitive Assessment of Challenge Model
When this model was tested with all the items contained in the original version of the instrument, inadequate fit indices were obtained, so items 21, 27, and 30 were eliminated, considering their value in regression weight obtained, their significance, and the identification of shared error rates. The final model therefore comprised nine items with adequate fit parameters (CMIN/DF = 1.567; NFI = .939, CFI = .977; AGFI = .926; SRMR = .044; RMSEA = .055). Two covariances between residuals were established. The result obtained was a unifactorial solution with an explained variance of 53.4% (Figure 3).
Convergent/divergent validity
Table 2 shows the correlation indices between the total scores of each CAI dimension and those of the disability, daily living activities, anxiety, and depression instruments.
Internal Consistency of the CAI
The final structure of the CAI in its version validated in Mexican population was reduced to 27 items organized into three factors, which are the same as those contained in the original version of the test, with satisfactory internal consistency coefficients (Factor 1: Loss or Damage = Cronbach’s α of .73, Factor 2: Threat = Cronbach’s α of .810 and Factor 3: Challenge = Cronbach’s α of .86).
Proposed Interpretation of CAI results
Finally, Table 3 presents the quarter distribution of the scores in the different dimensions or types of cognitive evaluations evaluated by the CAI, as well as the interpretation suggested for the sample studied.
Table 3 Interpretation of the CAI by distribution of scores by type of cognitive assessment in Mexican patients with chronic pain
|
Cognitive assessment
factor/type |
Score obtained | Interpretation |
|---|---|---|
| Loss/damage | 0-3 | None |
| 4-6 | Low | |
| 7-8 | Moderate | |
| 9 or more | High | |
| Threat | 0-4 | None |
| 5-7 | Low | |
| 8-9 | Moderate | |
| 10 or more | High | |
| Challenge | 0-3 | None |
| 4-6 | Low | |
| 7-8 | Moderate | |
| 9 or more | High |
Discussion and conclusion
This study provides evidence of the validity and internal consistency of the Spanish version of the Cognitive Assessment Instrument for Chronic Pain in Mexican patients. Confirmatory factor analyses verified the original structure of the CAI, comprising three factors: loss/damage, threat, and challenge, which coincide with those included in the theoretical model of Lazarus and Folkman on which the inventory is based. It is worth mentioning that the cognitive assessment of loss obtained a low explained variance, which was lower than the data obtained in the other types of assessment. Therefore, one element to consider in the future is the inclusion of additional items that could strengthen this factor, thereby increasing both its explained variance and its internal consistency.
At the same time, the analyses conducted to obtain convergent/divergent validity parameters provide further evidence of the relationship between cognitive evaluation and highly prevalent and disabling mental health problems in this population, such as anxiety and depression symptoms (Ahmad, 2005; Camacho et al., 2002; Craig, 1984; Herrero et al., 2008). The negative or inverse relationship between cognitive assessment of challenge and anxious and depressive symptomatology and level of disability highlights the importance of promoting this type of interpretation of chronic pain (rather than primary cognitive assessments of pain as damage/loss or a threat). This has been achieved through cognitive-behavioral interventions, such as adjuvant psychological therapy for patients with chronic diseases or conditions such as cancer (Cunningham, 2000), which suggests it should be implemented and assessed in patients with chronic pain due to different causes.
To continue advancing with this line of research, it is also suggested that additional analyses be conducted in future research to strengthen the evidence on the validity and reliability of the CAI, by exploring its predictive capacity, temporal stability, and sensitivity to change in the face of interventions, as well as its factorial structure when administered to other clinical populations.
The limitations of this study include the disparity between the sexes, the high number of unemployed subjects, and the broad age range. This sample distribution is expected as chronic pain mostly affects women and people with low socioeconomic status, and its prevalence increases with age (Schopflocher, Taenzer, & Jovey, 2011; Tsang et al., 2008; Pergolizzi et al., 2013). Also, although the correlations between the different types of cognitive assessment of pain and the variables of emotional distress and disability in this study were maintained after an analysis controlling for the sex and age of the subjects, studies are required to corroborate these findings in more homogeneous samples of patient groups of particular interest (such as those with musculoskeletal pain or the population with neuropathic pain). The results of this study should therefore be generalized with caution.











 text new page (beta)
text new page (beta)