Introduction
Smoking remains a major public health problem, and preventing smoking initiation, particularly among early adolescents (aged 10 to 14), is critical.1 Experimenting with cigarettes during adolescence predicts future smoking, and therefore, identifying adolescents who may be more likely to try a cigarette may help develop prevention strategies that target at-risk youth.2 Measures of tobacco use susceptibility are useful in cross-sectional research on youth smoking because they help reduce concerns about reverse causality from prior and current engagement in smoking behavior. Indeed, susceptibility to smoking is the primary pathway by which diverse factors promote tobacco use behavior amongst never-smokers, similarly to the concept of “behavioral intentions” in different theories of behavior change.3 An established measure of smoking susceptibility predicts smoking initiation in high-income countries,4,5 although its predictive validity in Latin American countries has not been assessed, nor has a measure to predict e-cigarette initiation. Furthermore, the growing array of nicotine products suggests that, eventually, it will be important to determine whether product-specific measures of susceptibility are needed to discriminate between youth at risk of using different types of tobacco products.
Susceptibility to smoking is the absence of a firm decision not to smoke in the future, and appears to be influenced by smoking among parents and friends,4 as well as by exposure to advertising at the point of sale (POS).6,7,8,9 A 3-item susceptibility measure was developed in the early 1990s, based on two key domains: intentions (e.g “Do you think that you will try a cigarette soon?” “Do you think you will be smoking cigarettes one year from now?”) and expectations for future smoking behavior (e.g., “If one of your best friends were to offer you a cigarette, would you smoke it?”). In order to be classified as not susceptible to smoking, respondents had to answer “no” to the first question and “definitely no” to the other two.4 The predictive validity of this measure has been confirmed with several nationally representative, longitudinal samples of adolescents in the United States (US).5,10,11 Some cross-sectional studies have assessed 2- or 3-item measures of susceptibility as an outcome in low- and middle-income countries like Cambodia, Laos and Vietnam,12 Mexico13,14 and Argentina.7,15 These studies assumed that susceptibility predicts future cigarette smoking behavior; however, this has not been evaluated.
It is important to assess the discriminative validity of cigarette susceptibility when studying the emergence and spread of electronic cigarette use. Longitudinal studies in the US16 and Mexico17 have found that e-cigarette use among adolescents increases the likelihood of smoking cigarettes. Evaluation of the public health impact of e-cigarettes requires assessing whether or not e-cigarette users who become cigarette smokers would have done so in the absence of e-cigarettes.18 Cross-sectional studies in the US19 and Mexico20 indicate that exclusive e-cigarette use is being undertaken by adolescents with smoking-related risk factors that are intermediate between those of non-users and those of individuals who use cigarettes, e-cigarettes or both. Exclusive e-cigarette use among these “medium-risk” youth is of potential public health concern because they might not have initiated nicotine use in the absence of e-cigarettes. This would be supported if susceptibility is more strongly associated with the initiation of cigarette use than with e-cigarette use.
Our study aimed to assess whether or not a 2-item susceptibility measure predicts smoking behavior in a sample of early adolescent students in Argentina and Mexico (figure 1). As a secondary outcome, we aimed to assess whether susceptibility to smoking predicted e-cigarette initiation, and the strength of this association. Results should inform future approaches to measurement, as well as informing debates around the public health impact of e-cigarettes in two countries where e-cigarettes are banned but can still be bought.
Materials and methods
A school-based longitudinal study was carried out in three of the largest cities in Argentina (Buenos Aires, Córdoba, and Tucumán) and in Mexico (Mexico City, Guadalajara, and Monterrey), with baseline data collected from first-year secondary school students. The parents or caretakers of participating students provided passive consent; the students signed an active consent form. A detailed description of the school selection in both countries and the survey used in this study have been published elsewhere.20,21
The baseline data collection took place during 2014 in Argentina and during 2015 in Mexico, with a follow-up survey in 2015 in Argentina (mean between-wave interval=17.1 months; range=16 to 19.3 months), and in 2016 in Mexico (mean between-wave interval=20.4 months; range=19.5 to 21.4months). An anonymous linking procedure was used to allow for follow-up while ensuring anonymity.22
The research protocol was approved by an NIH-certified human subjects research board in Buenos Aires (CEMIC) and by the Mexican National Institute of Public Health ethics committee.
Measurement
The primary dependent variable for this study was smoking behavior at follow-up. Smoking initiation was based on the positive answer to: “Have you ever tried a cigarette?” and a negative answer to “Have you smoked a cigarette in the last 30 days?” Current smoking was based on a positive answer to “Have you smoked a cigarette in the last 30 days?” E-cigarettes initiation was assessed by asking: “Have you ever tried an e-cigarette?” Dual use was defined as any use of cigarettes and any use of e-cigarettes.
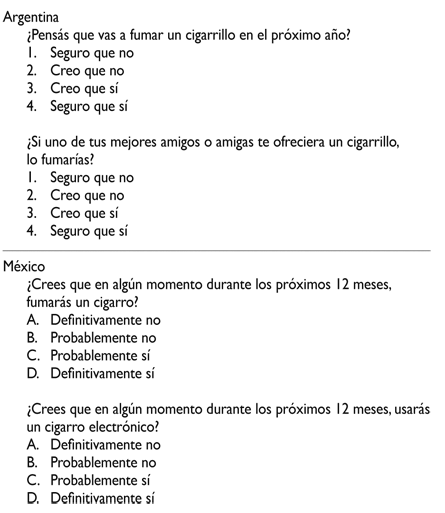
The main independent variable was susceptibility to smoking, which was assessed based on two questions: “If one of your best friends were to offer you a cigarette, would you smoke it?” (“friends cigarette offers”) and “Do you think you will be smoking cigarettes one year from now?5 (“next year smoking”). Response options were “definitely not,” “probably not,” “probably yes” and “definitely yes.” To be classified as non-susceptible, a student had to answer “definitely not” to both questions; otherwise, the student was considered “susceptible”.3
Having at least one family member (mother, father, sibling) or close friend who smoked (out of five closest friends) was considered positive network exposure to smoking. Exposure to advertising at the point of sale (POS) was assessed with two questions on how often students went to stores that sell cigarettes near their schools or further away.6 In both countries, POS pack displays are the only marketing allowed, making them the primary venue for tobacco advertising exposure. Students who answered “often” or “very often” to either question were classified as exposed at POS.
Sociodemographic variables included: age, sex, type of school (public vs private) and educational attainment of parents (i.e., highest level reported for either parent). Personal variables included poor school performance (held back a grade in school in Argentina; grades below 7/10 in Mexico); a 4-item sensation-seeking scale with higher scores indicating higher sensation seeking tendencies (range 1-5).23 Parenting behavior was assessed using the Jackson’s Authoritative Parenting Index.24 Scores were averaged for both parents, with higher scores indicating more authoritative parenting (range 1-5).25
Analysis
Analyses were conducted using Stata version v13 (Stata Corp, College Station, TX). The analytic sample included students who, at baseline, had never tried cigarettes or e-cigarettes and who completed both surveys. In an attrition analysis, we examined differences between students who were and were not followed-up using t-test for continuous variables and chi-square test for categorical variables. Multilevel logistic regression models with random intercepts for schools were used to assess the association between baseline susceptibility and initiation and current tobacco use at follow-up. For cigarette behavior outcomes, we analyzed each susceptibility question separately, as well as using the combined measure. For models that integrated e-cigarette initiation, we estimated three different outcomes: 1. Trial of e-cigarettes only; 2. Trial of cigarettes only; 3. Trial of both. Fully adjusted models for all outcomes controlled for age, sex, type of school, parental education, sensation seeking, parenting, poor school performance, network cigarette smoking, and POS exposure.
We estimated the sensitivity, specificity, positive predictive value and negative predictive value of the smoking susceptibility measure.
In order to assess potential biases from attrition, we re-estimated all models while adjusting for individual weights based on the inverse probability of being followed up. These models did not result in any meaningful differences in the statistical significance of estimates. Therefore we present only the unweighted results.
Results
Overall, 3 172 students in Argentina (83% participation rate) and 10 123 students in Mexico (84% participation rate) completed the survey at baseline. Of these, 2 482 students in Argentina and 7 147 in Mexico had never tried a cigarette or an e-cigarette and were considered eligible for our analysis. In Argentina, adolescents lost to follow-up were more likely to be male and older, to attend public schools, and to have parents with lower educational attainment (table I). They also had more household members or friends who smoked and were more susceptible to smoking. In Mexico, adolescents lost to follow-up were more likely to be older and to have parents with lower educational attainment.
Table I Characteristics of the non smoking students who completed the follow up survey and those who didn´t. México-Argentina, 2014-02016
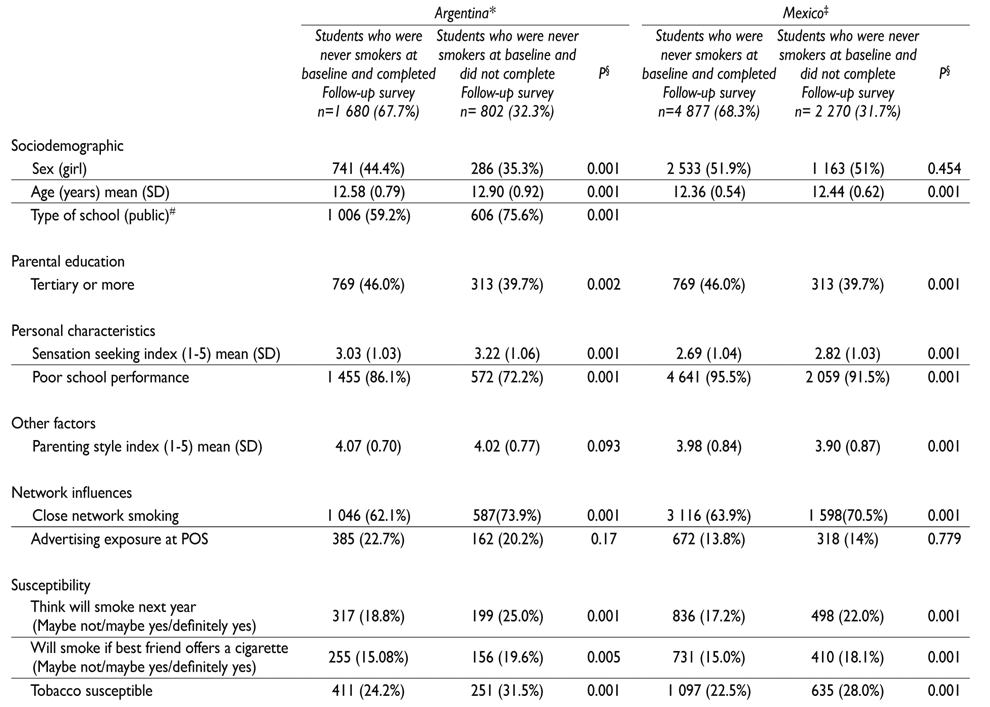
* Survey implemented in Buenos Aires, Córdoba and Tucumán. Baseline survey during May-July 2014. Follow up survey during October-November 2015
‡ Survey implemented in Mexico City, Guadalajara, and Monterrey. Baseline survey during February March 2015. Follow up survey during October- November 2016
§ t-test for continuous variables and chi-square test for categorical variables comparing students that were follow up and those who were not.
# In Mexico all schools were public
SD: Standard Deviation
At followup, in Argentina 14.8% of the analytic sample had tried a cigarette (but not in the last 30 days), 6.1% had tried an e-cigarette, and 9.4% were current smokers; in Mexico, 18.8% had tried a cigarette (but not in the last 30 days), 22.6% had tried an e-cigarette, and 5.7% were current smokers.
Predictors of smoking initiation
In adjusted, multivariate analysis (table II), smoking susceptibility was associated with increased risk of smoking initiation in both countries (Argentina: AOR 2.28; 95%CI 1.66-3.14; Mexico: AOR 2.07; 95%CI 1.74-2.45). When analyzed separately, each susceptibility question was independently associated with an increased risk of smoking initiation in Argentina (AOR 1.95; 95%CI 1.38-2.75 and AOR 2.50; 95%CI 1.75-3.59, respectively) and Mexico (AOR 2.15; 95%CI 1.79-2.59 and AOR 2.11; 95%CI 1.74-2.56, respectively).
Table II Smoking initiation and current smoking at follow up among never smokers at baseline in Argentina* (A) and Mexico‡ (B). 2014-2016
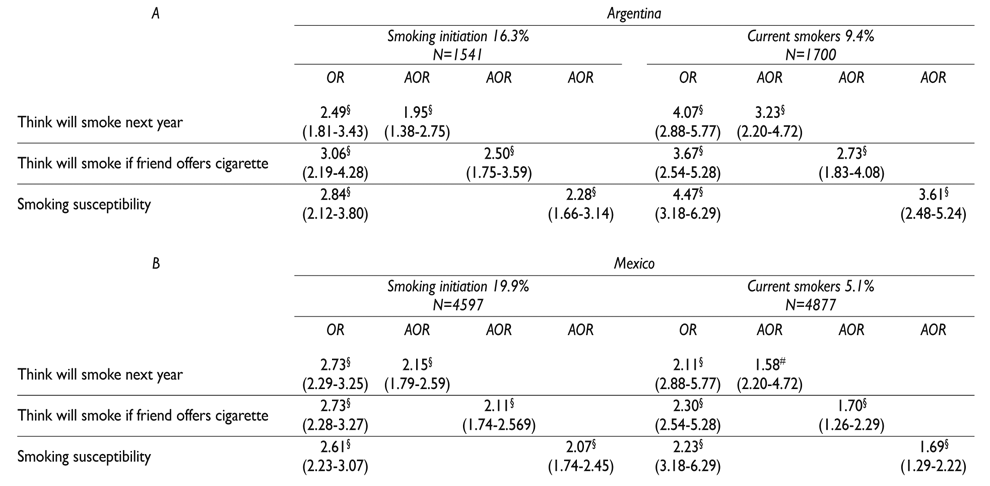
* Surveys in Buenos Aires, Cordoba and Tucuman. October- November, 2015
‡ Surveys in Mexico City, Guadalajara, and Monterrey. October- November 2016
§ p<0.001
# p<0.01
The model was adjusted by age, sex, type of school, parental education, sensation seeking index, poor school performance, parenting style, network exposure to tobacco and POS exposure
Predictors of current smoking
Susceptibility was also independently associated with an increased risk of being a current smoker at follow-up in Argentina (AOR 3.61; 95%CI 2.48-5.24) and Mexico (AOR 1.69; 95%CI 1.29-2.22; table II). When analyzed separately, each susceptibility question was independently associated with an increased risk of smoking initiation in Argentina (AOR 3.23; 95%CI 2.20-4.72 and AOR 2.73; 95%CI 1.83-4.08, respectively) and Mexico (AOR 1.58; 95%CI 1.19-2.11 and AOR 1.70; 95%CI 1.26-2.29, respectively).
Table III shows the association between the independent variables with trial of only cigarettes, only e-cigarettes, or both at follow-up. In Argentina, susceptibility to smoking predicted cigarette initiation (AOR 2.85; 95%CI 2.15-3.77) but not e-cigarette initiation, whether exclusive (AOR 0.39; 95%CI 0.13-1.14) or in conjunction with cigarette (AOR 1.50; 95%CI 0.82-2.76). In Mexico, susceptibility to smoking predicted cigarette initiation (AOR 1.61; 95%CI 1.31-1.98), e-cigarettes initiation (AOR 1.29; 95%CI 1.02-1.63) and trial of both (AOR 1.97; 95%CI 1.62-2.39).
Table III Exclusive trial of tobacco, exclusive trial of e-cigarette and trial of both among never smokers at baseline in Argentina* and Mexico‡. 2014-2016
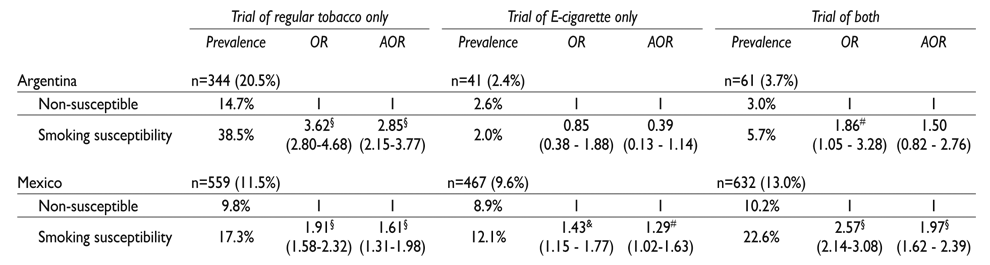
* Surveys in Buenos Aires, Cordoba and Tucuman. October- November, 2015
‡ Survey in Mexico City, Guadalajara, and Monterrey. October- November 2016
§ p<0.001
# p<0.05
& p<0.01
The model was adjusted by age, sex, type of school, parental education, sensation seeking index, poor school performance, parenting style, network exposure to tobacco and POS exposure
The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the susceptibility measure for all outcomes by country is shown in table IV. The PPV of the measure was adequate for predicting cigarette initiation in both countries (29.3% in Argentina and 33.7% in Mexico); however, it was lower for current smoking (21.2% in Argentina and 9.7% in Mexico) and for e-cigarette initiation (7.7% in Argentina and 12.1% in Mexico).
Table IV Susceptibility measure: sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the susceptibility to smoking measure among students who tried a regular cigarette but are not current smokers, current smokers and those who only tried an e-cigarette. México-Argentina, 2014-2016
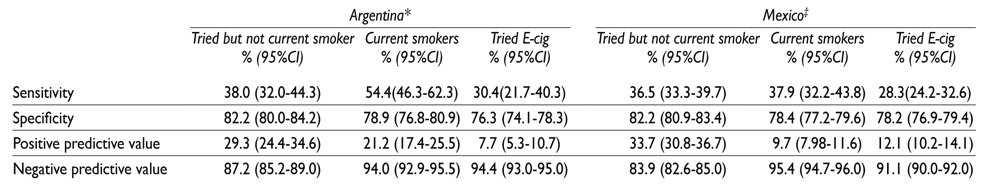
* Surveys in Buenos Aires, Cordoba and Tucuman. October- November, 2015
‡ Surveys in Mexico City, Guadalajara, and Monterrey. October- November 2016
Discussion
The 2-item measure of susceptibility to cigarette smoking was significantly associated with subsequent smoking initiation and current smoking among early adolescents in Argentina and Mexico, although the association was relatively weaker in Mexico where initiation rates were lower. The measure, however, did not predict e-cigarette initiation in Argentina and predicted it only weakly in Mexico, suggesting that e-cigarettes may appeal to youth who were unlikely to become cigarette smokers.
Susceptibility to smoking has been defined using different questions.26,27We used a short version of the susceptibility measure proposed by Pierce et al., without the question “Do you think that in the future you might experiment with cigarettes?” that had been previously used.15,28 The effectiveness of the Pierce measure in a sample of U.S. adolescents was validated approximately 20 years ago, and it proved to be a stronger predictor of smoking initiation than the existence of smokers among either the family or the best-friend network. However, contrarily to our study, they found that exposure to smokers in the close network was more important than susceptibility for distinguishing those adolescents who progressed to established smoking.4 A study performed among adolescents with Mexican origin also found that the susceptibility to smoking measure was the strongest predictor of smoking initiation.29
The index used by Pierce classified 48% of the 12 to 15 year old population of California in 1996 as susceptible to smoking. In our sample, 24% of the students were susceptible to smoking regular cigarettes, which is similar to earlier data collection efforts among similarly aged Mexican adolescents (27.5% of females and 29% of males).14In our study, the sensitivity for current smoking was 54.4% in Argentina and 37.9% in Mexico. The positive predictive value for current smoking was 21.1% in Argentina and 9.7% in Mexico. The specificity and the negative predictive value were high in both countries, which shows that the measure is effective for detecting students who will not progress to smoking. Nodora et al. added a question about curiosity in regard to smoking to the original index, which increased from 25.1 to 46.9% in the proportion identified as “at-risk to smoke”.30
The cigarette susceptibility measure showed mixed evidence around the prediction of e-cigarette initiation. In Argentina, the susceptibility measure did not predict e-cigarette initiation. The non-significant tendency suggested that susceptible never-smokers were equally or less likely to try e-cigarettes than non-susceptible never-smokers (i.e., 2.0 vs 2.6%, respectively). Therefore, this susceptibility measure seems to discriminate between initiation of cigarettes relative to e-cigarettes. In Mexico, we found a relatively weak but positive association with exclusive e-cigarette initiation, and a stronger association with dual trial. This significant association may be due to higher rates of e-cigarette trial in Mexico (10%) compared to Argentina (3%). This may mean that the norms and risk factors for e-cigarette initiation are somewhat different in both countries. Standard risk factors for cigarette use (e.g., friend smoking, sensation seeking, ad exposure) were associated with e-cigarette initiation in both countries. However, other factors that are not associated with conventional cigarette use may help explain e-cigarette susceptibility and use, such as “technophilia” (i.e., pleasure from new electronic devices).20 Results indicate a need to find measures that better predict e-cigarette initiation. Substituting key terms in standard cigarette susceptibility questions may help (i.e., “using e-cigarettes” for “smoking”), but the predictive validity of this measure should be assessed, and other potential risk factors should be identified and valid measures developed.
This study has several limitations that should be acknowledged. Students lost to follow-up were more likely than followed-up students to have risk factors for cigarette use, such as higher sensation seeking or network smoking. Hence, we may have underestimated the transition to smoking initiation and current smoking in this population. Schools were not randomly selected, and the sample of schools may not be representative of the general population of Argentina or Mexico. However, schools were selected to represent the range of socioeconomic diversity in three large cities in each country, which suggests that the results might be similar for other urban populations. In our study, we only assessed cigarette smoking. Results from the Global Youth Tobacco Survey show that 12.6 % of Argentinean students31 and 9.6% of Mexican students32 refer use of other tobacco products. A recent study showed that in 2015, 8% of second-year secondary students in Argentina had tried an e-cigarette.33 Further research should evaluate whether this measure can be reworded to assess other kinds of tobacco use or e-cigarette consumption (i.e. Do you think you will be using e-cigarettes one year from now?). Our study did not include a question about curiosity; we suggest assessing whether or not adding such question to the Spanish version would result in a higher proportion of detected susceptible students. Recently, four trajectories have been identified in the smoking uptake behavior: experimenters, quitters, early established smokers and late escalators.34 Our study only considered experimenters and current smokers.
In spite of these limitations, our results support the use of this two-item measure of susceptibility to smoking as a valid tool to detect adolescents at risk of experimenting with and using cigarettes in Argentina and Mexico. Futures studies about smoking behavior among adolescents should use this short measure although other measurement approaches appear necessary to study susceptibility to e-cigarette use. These measurement approaches can help evaluate specific public health campaigns and policies, as has been documented in Costa Rica35 and Uruguay,36 where the implementation of comprehensive tobacco control public policies have reduced the susceptibility to tobacco consumption.











 text new page (beta)
text new page (beta)