Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Salud Pública de México
Print version ISSN 0036-3634
Salud pública Méx vol.55 suppl.4 Cuernavaca 2013
Artículos originales
"La Familia" HIV prevention program: A focus on disclosure and family acceptance for Latino immigrant MSM to the USA
Programa de prevención de VIH "La Familia": Un enfoque en la divulgación y aceptación de la familia en los inmigrantes latinos HSH en los Estados Unidos
Rita M Melendez, PhD,(1) Jorge Zepeda, ACSW, MSW,(2) Rafael Samaniego, PhD,(3) Deepalika Chakravarty, MS,(1,4) Gabriela Alaniz, MPH.(2)
(1) Sexuality Studies Department, Center for Research and Education on Gender and Sexuality, San Francisco State University. San Francisco, California, EUA.
(2) San Francisco AIDS Foundation. San Francisco, California, EUA.
(3) Área de Ciencias de la Salud de la Universidad Autónoma de Zacatecas. Zacatecas, México.
(4) Center for AIDS Prevention Studies, University of California at San Francisco. San Francisco, California, EUA.
Abstract
Objective. The objective of this study was to pilot test and evaluate a HIV prevention program that used a Freirean approach to engage Latino immigrant MSM (men who have sex with men) on issues of sexual orientation, family acceptance, stigma as well as HIV prevention and sexual risk behaviors.
Materials and methods. Participants were evaluated using a survey before and after participation in the program and compared to a control group. Focus groups where participants discussed their experiences in the program as well as perceptions of the program were held and analyzed.
Results. Survey results indicate that after their participation in the program, participants increased their safer sex behaviors, comfort disclosing their sexual orientation and support from friends.
Conclusions. HIV prevention needs to incorporate cultural, social and structural factors.
Key words: latinos; immigrants; HIV; prevention; family; disclosure; stigma; homophobia.
Resumen
Objetivo. El objetivo de este estudio fue probar de manera piloto y evaluar un programa de prevención de VIH que usó una aproximación Freiriana que motivaba a los HSH (hombres que tienen sexo con hombres) en temas de orientación sexual, aceptación familiar, estigma, prácticas sexuales de riesgo y prevención de VIH.
Material y métodos. Los participantes contestaron un cuestionario antes y después de participar en el programa mismo que se comparó con un grupo piloto. También se llevaron a cabo grupos focales donde los participantes discutieron sus experiencias y percepciones sobre el programa.
Resultados. El análisis de los resultados señala que después de su participación en el programa, los HSH reportaron más prácticas sexuales seguras, más comodidad en revelar su orientación sexual y apoyo de amistades.
Conclusiones. La prevención del VIH debe tomar en cuenta factores culturales, sociales y estructurales.
Palabras clave: latinos; inmigrantes; VIH; prevención; familia; revelación; estigma; homofobia.
Latinos accounted for 17% of new HIV infections during 20061 and comprised 18% of people living with HIV.2 In the USA, AIDS cases are most prevalent among MSM, and this is also the case for Latino MSM.1 For Latino men, male-to-male sexual contact accounts for 60% of reported HIV cases.1 In 2007, the CDC estimated that the number of AIDS cases among Mexican-born individuals was 1 431 (18.5%) out of a total of 7 752 AIDS cases among all Latino subgroups.1 In California, the HIV prevalence among Latino MSM varies considerably; studies have found prevalence rates ranging from 5 to 35%.3 Further, it is possible that the actual HIV/AIDS rates are higher than reported due to the lack of access to health care among many Latino immigrants in the USA.
Research on HIV prevention with Latino immigrant MSM recommends approaches to HIV prevention that integrate individual behavioral factors with social, cultural, and structural factors.4-10 Immigration to the US is an essential contextual issue with regard to Latino MSM and their HIV risk. Although it is widely assumed that Latino immigrants only migrate for economic reasons, another type of migration –sexual migration4– provides insight into barriers to safer sex for Latino MSM who are immigrants. Sexual migration can entail leaving their home country to protect their family from the shame and stigma of having a gay or bisexual son. Men may also migrate away from their home country to escape the stigma they feel towards their desires and behaviors and to be able to live more openly as a gay or bisexual man.4
Latino gay and bisexual men report the highest mean number of negative family reactions to disclosure about their sexual orientation, as compared to whites (males and females) and Latinas.11 Participants with high levels of family rejection were 3.4 times more likely to report engaging in unprotected sexual intercourse, 8.4 times more likely to have attempted suicide, and 5.9 times more likely to report high levels of depression than participants with no or low levels of family rejection.11 Oppression, as measured by experiences of homophobia, poverty, and racism, contributes to the risk of HIV infections.7 In measuring homophobia, the study reported that 70% of participants felt that their homosexuality hurt and/or embarrassed their families.7 Furthermore, the study found that Latino men who were considered "high risk" – defined as those engaging in unprotected anal intercourse with casual partners - also reported more experiences of homophobia and oppression in general, than Latino men considered "low risk".7
Materials and methods
La Familia was implemented by the San Francisco AIDS Foundation (SFAF) as part of their services for HIV prevention among Latino MSM. The objective of this study was to conduct and evaluate a pilot HIV prevention intervention that asks men to discuss and explore issues relating to their families and sexual disclosures. Because the program was developed and implemented as part of service provision at the San Francisco AIDS Foundation the San Francisco State University Institutional Review Board (IRB) for the protection of human subjects informed us that it was exempt from IRB approval process. However, we followed the ethical guidelines as outlined by IRB procedures to ensure the protection of participants. Participants were verbally informed that the program would be evaluated and that their answers to the surveys and focus groups could be used to evaluate the effectiveness of the program and to make recommendations for changes. Additionally, we informed participants that their names would not be used in any way. Instead of having participants enter their names for the questionnaires a code was used for each survey so that names were never attached to the questionnaires or the data in any way. All participants were asked to sign their agreement to participate in the program and evaluation, on November 6, 2010 in San Francisco, California at the Instituto Familiar de la Raza where the program was held.
Development and description of the La Familia Program: We created and pilot tested an HIV prevention program titled La Familia that specifically addresses issues of disclosure of sexual orientation, family rejection, and issues relating to oppression for immigrant Latino MSM in the USA. La Familia is a 12-session program offered over a 6-week period guided by Paulo Freire's principle of "popular education."12 We designed a program that did not see participants as lacking in knowledge on HIV prevention, but rather one where participants were viewed as experts in their lives and challenges to safer sex behavior. Discussion rather than lecture was the main component of the program. This approach allows for cultural nuances to shine through from the participants rather than through the creators of the program. The program was named La Familia to emphasize its focus on the relationships Latino immigrant men have with their families.
As the first step in development, we conducted a focus group with 12 Latino immigrant MSM. The men were recruited through the SFAF and conducted by the facilitator of the support groups that are regularly held at the SFAF. These initial focus group participants emphasized the importance of the family in the development and acceptance of their sexual identities. Participants felt that disclosure involved having the skills and confidence to disclose their sexual identity if and when they choose to, as well as to whom they choose to disclose to.
In light of the participants' desire for "real world" examples and assistance, we incorporated the use of "sexual scenes" in the sessions to help participants identify HIV risk factors and HIV preventive strategies by reconstructing a scene we presented to them as well as one they created themselves.13 Further, we incorporated a story-telling component through which participants tell their own stories related to the topics discussed in each session.
Recruitment: We recruited Latino immigrant MSM, 18 years or older, living in the USA for 10 years or less, currently residing in the San Francisco Bay Area, and who speak Spanish as a primary language. Interested men provided their name and phone number to project staff and were contacted later to determine eligibility. Potential participants were recruited through the SFAF as well as social venues where Latino men are found such as bars, restaurants, and cafes. Because there were more men interested in the program than available spaces, we divided the group into an intervention and a control group – where the intervention group received the program immediately and the control group was asked to come in for assessments and encouraged to attend the regular support groups for Latino MSM through the SFAF. Selection into the intervention and control groups did not happen by traditional randomization. Participants who we reached in the first call, who were eligible, and who were available for Saturday sessions were enrolled into the intervention arm of the study. In total we enrolled 35 men for the intervention group and 14 men for the control group.
Evaluation: We created three self-administered questionnaires for our quantitative analysis: a pre-test questionnaire, a post-test questionnaire, and a follow-up questionnaire. Participants completed the pre-test during Week 1 of the program, the post-test during Week 6, and the follow-up questionnaire two months after the end of the intervention sessions. The control group completed the questionnaires at approximately the same intervals as the intervention participants. To account for varying literacy levels within the sample population, facilitators read the questions out-loud to participants.
The 92-item pre-test and the 75-item post-test include relevant demographics and outcome measures. The assessments have five main sections: demographics (pre-test only), sexual behavior, oppression and harm, disclosure, and social support/communication. The post-test questionnaire includes an additional 14 questions to assess the participants' perceptions about whether their behavior or attitudes have changed after participating in the intervention. The follow-up questionnaire is identical to the post-test questionnaire.
In addition to the questionnaires, the intervention group also participated in a focus group during the final session. Two women who worked on the project and somewhat known to the participants of the intervention came to the final session and asked questions to the men concerning comfort with disclosure, comfort with sexual identity, and risk-taking behavior. Their aim was to initiate conversation among the men. The facilitators of the intervention were not present for the focus group to allow the men to speak freely about their thoughts on the program and changes or improvements that could be made. A separate assistant took notes of the men's statements because some men felt uncomfortable being audio recorded.
The four objectives of the program guided the evaluation of La Familia:
1. Decrease in HIV risk-taking behavior: a) condom use, b) intentions to use condoms, and c) use of substances or sexual intercourse to cope with depression and/or loneliness.
2. Reduction in internalized homophobia: a) self-acceptance, b) self-esteem, and c) self-comfort with sexual identity.
3. Increased comfort with disclosure of sexual identity to family and loved ones: a) comfort level, and b) intention to disclose.
4. Increased social support, sense of belonging to a community/group, and sense of connectedness.
Data analyses: Questionnaires had an identification code containing participants' initials and a number; this helped match pre, post, and follow-up questionnaires. Data from the paper questionnaires was first entered into SPSS and then transferred to SAS for analyses. All data were cleaned and the accuracy of the data was verified. The pre-and post-data were compared for the control and intervention groups separately. Because the total sample size as well as that of the various groups (pre, post, control, and intervention) is small, the p-values reported are from the Fisher's Exact test which is specially formulated for small samples (almost all statistical tests done were for categorical variables).
The notes from the focus group were analyzed using a combination of open and closed coding. For open coding themes emerged from what the participants revealed during the focus group. Closed coding was used to focus on the specific goals of the program such as comfort disclosing sexual identity.
Results
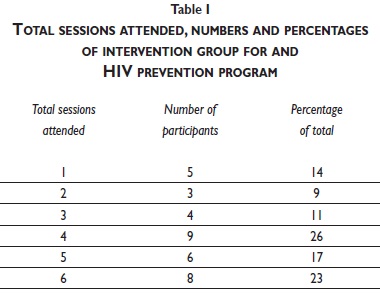
Attendance in La Familia: Each of the 35 intervention participants attended at least one content session, with attendance at individual sessions ranging from 16 to 30 participants. A total of 23 participants (66%) participated in 4 sessions or more and 12 participants (34%) attended 3 sessions or less (table I). In accordance to the intent-to-treat principle,14 participants enrolled in the intervention group were analyzed as one group regardless of the number of sessions attended.
Sample characteristics: The sample consisted of 30 men who took the pre-test as part of the intervention group and 14 men who took the pre-test as part of the control group. Five additional men participated in the intervention group but did not take the pre-test and are not included in the quantitative analyses. Additionally, some participants chose to not respond to certain questions. The present sample characteristics are therefore for these 44 men and based on available data.
In the overall sample, the mean age was just under 38 years; however, there was a statistically significant difference (p-value ≤ 0.030) between the intervention and control groups with regard to age, with the control group being older (mean = 43.3 years; SD = 12.1 years) than the intervention group (mean = 35.5 years, SD = 9.7 years). It is unclear why this difference emerged and may be due to random chance or due to the recruitment of the control group. Participants needed to be available for Saturday meetings to participate in La Familia which may have resulted in an older group of men in the control group as compared to the intervention group.
More than half of the men (52%; n = 23) were born in Mexico. The remaining participants were equally split between being born in Central America and South America (14% or n = 6 for each). Forty one percent of the men (n = 18) reported that most of their family live in Mexico. Over a third of the sample (36%) had completed secondary school and another 20% had completed university education (table II). There were no significant differences between the control group and the intervention group along any of the demographic variables.

Participants were asked about their feelings regarding disclosure of their sexual orientation to their families. About one-quarter (23%; n = 10) reported that they fear isolation and rejection if they disclose to their families that they are gay. Six men (14%) reported that they fear being victims of violence if they disclose to their families that they are gay. There was a remarkable history of violence among the participants in the sample. One-quarter (25%, n = 11) had experienced violence at some point in their lives due to disclosing that they are gay. Almost half (48%; n= 21) reported experiencing violence as a child.
With regard to sexual behavior, participants reported engaging in both receptive and insertive anal sex in the past three months (43 and 50% respectively). In each scenario, of those who had anal sex, less than a third (32%) reported "always using a condom." A small percentage (9%) reported engaging in vaginal sex and half of those men (n=2) reported using condoms "always" for vaginal sex.
Results for objective I – HIV risk-taking behavior: Several pre- and post-measures were used to examine changes in HIV risk-taking behavior. Although results were not significant, there were changes in men's behaviors around safer sex in the expected direction. For example, five men in the intervention group who responded in the pre-test that it was "definitely improbable" that they would use a condom when they initiate sex, later responded during the post-test (immediately following the end of the program) that it was "definitely probable" that they would use a condom. There was little to no change with regard to alcohol or drug use for the participants of the program at either follow-up assessment.
The intervention had a positive effect on participants' reports of their use of sex for emotional reasons. Three men in the intervention group who at the pre-test reported that they "definitely" and "primarily" have sex to feel better, responded "primarily no" or "definitely no" to the same question post-intervention (results significant at p ≤ 0.050); the same analyses for the control group resulted in no significant differences between pre- and post-test.
The qualitative data supports the result that participants are moving towards safer-sex practices post-intervention. One participant reported being able to talk to his partner about using protection and about health. Another participant reported that in the past he had "done it [sex] without a condom," and felt that after the program that he would change his behavior and be able to ask a partner to wear a condom.
Most behavior changes occur significantly after the end of the intervention from between 6 months to one year following post-intervention.15,16 To this end, we observed changes at the 2-month follow-up assessment. Men were asked how likely they were to use a condom the next time they have sex. A total of seven participants in the program had said that it was "definitely improbable" at the pre-test and at the 2-month follow-up said that it was "definitely probable" (p ≤ 0.010). Likewise there was movement in the direction of increased safer sex behaviors with regard to men changing their responses when asked if they would have sex with a partner who does not have a condom (p ≤ 0.010) between the pre- and 2-month assessments.
Results for objective II – Internalized homophobia: When examining internalized homophobia among participants few significant changes were observed. For example, for the statement "Heterosexuals are better than gay men," a single participant in the intervention group who responded 'absolutely agree' at pre-test, changed his response to 'absolutely disagree' at post-test. The majority, 56% did not change their answer from "absolutely disagree" that heterosexuals are better than gay men and remained the same for the 2-month follow-up assessment. Another question asked participants if they felt ashamed to be gay – while there was a significant change at the post-assessment the effect was not observed in the 2-month follow-up. Change was observed when asking men if they agreed with the statement "I am ashamed to be gay or homosexual." A total of 11 men agreed with the statement at the pre-test and later changed their responses to "disagree" at both the post-and 2-month assessments (p ≤ 0.010 at post-test and not significant 2-month follow-up).
The qualitative data reveals that most participants were, to some degree, comfortable with their sexuality. One participant reported that before participating in the program, he felt more ashamed and he was not able to talk to anyone about his sexuality and that he was not able to meet with homosexual groups.
Results for objective III – Comfort with disclosure: With regard to disclosure, several questions asked participants about their comfort and experiences disclosing their sexual identity to their family members. Of the men in the intervention group, 13 said at the initial post-test that they were able to reveal their sexual orientation to someone in their family during their participation in La Familia (marginally significant at p ≤ 0.070).
At the 2-month follow-up more men who were in the intervention group as compared to the control group reported that they felt more comfortable with their sexuality (58 vs. 27%, p ≤ 0.020) and that they have tools to reveal their sexual orientation to their families (55 vs. 30%, ns). At the 2-month assessment, a total of 13 (49%) men reported that they had been able to reveal their sexual identity to a family member as compared to 19% of the control group (p ≤ 0.030).
The qualitative data confirms that disclosure occurred during the program. One participant reported sharing his sexual identity with a girl who was in love with him. He told her he was homosexual and for her to look for a man who could reciprocate her feelings. This participant also reported informing his aunt and cousins (who he lives with) about his sexual identity.
Results for objective IV – Social support: While we expected the intervention to have positive effects with regard to referrals and connections, the results of the data from the post-test immediately following the program demonstrated no statistically significant differences between pre- and post- for the intervention group – although all results were in the expected direction of increasing referrals and connections with other gay men.
At the 2-month follow-up we did see some signs of social support emerging from the program. Sixteen men from the intervention group reported they felt they had more friends who understood their problems (p≤0.010). Additionally, at the 2-month assessment four men who had previously stated that they do not feel like they are a part of the gay community in Mexico reported that they do feel a part of the gay community in Mexico (p ≤ 0.030).
One of the main themes arising from the qualitative data in this area was the closeness of the intervention group. The participants reported benefiting greatly from other group members' experiences and feeling being part of a family through their participation in the group. The interviews and focus group discussions highlight the sense of family that was felt during the program. Participants reported feeling supported by other group members and identifying with them and their experiences.
Discussion
The La Familia program incorporates the importance of disclosure to family and acceptance by the family as a means of decreasing sexual risk among Latino immigrant MSM and builds upon and strengthens skills and resiliency factors already present in the participants. While this study was only a pilot program, the preliminary results of those who participated in the program demonstrate some positive findings that can and should be expanded to a larger sample. One limitation was not observing a decrease in sexual risk behavior but only an increase in participants' intentions to use condoms. Additionally, as the Cass Identity Model17 makes clear, there are six stages of developing a gay or lesbian identity – it is possible that the men in this study had already advanced towards several steps and the program either confirmed these stages or helped them advance forward more. The program, therefore, may be better suited for those willing to attend who have already made some progress with regard to developing their sexual identity. The program may be particularly suited also for those participants who have to incorporate the affects of social stigma within their identity development. Ideally, a future study would analyze the stages of identity development along with having a larger participant sample, and a longer follow-up after completion of the program.
One of the strengths of the La Familia HIV prevention intervention is that it contextualizes HIV risk within the social and cultural experiences encountered by Latino immigrant MSM. The contextualization occurs through having participants speak as the experts of their own lives versus having experts speak to them about sexual health. Rather than create a program that defines cultural factors for participants, this program allowed participants to describe their lives and their experiences. This is not to say that HIV prevention interventions should not incorporate HIV education and prevention methods provided by knowledgeable individuals, only that this educational approach should not be the sole approach to HIV prevention. The second implication is that HIV prevention interventions need to treat the populations they serve as equal partners who are capable and knowledgeable about protecting themselves against HIV infection.7
The findings from this project have several public health and policy implications that have also been recommended in earlier studies. The first implication is that HIV prevention needs to incorporate cultural, social, and structural factors.4,7,9 This program followed the recommendations found in the literature to move beyond individual behavioral approaches. HIV prevention needs to move beyond a deficit-based approach where the individual is seen as lacking in ability to guard against HIV infection, to a discussion based approach that emphasizes the participants own experiences and as agents of change and experts on preventing HIV infection.7
Recommendations
• Increased services for Spanish-speaking Latino MSM are needed in the USA.
• Increase groups to discuss role of family in behaviors.
• Alter existing HIV prevention programs already in use may be altered to include an exercise or section where the family is discussed in relation to the lives of Latino MSM.
• Increase Support services for disclosing sexual orientation to parents and siblings should be offered to Latino MSM.
References
1. CDC. HIV/AIDS Surveillance Report 2009. [Internet]. Atlanta: CDC. [Cited February 21, 2010]. Available from: http://www.cdc.gov/hiv/topics/basic/index.htm#hiv. [ Links ]
2. Kaiser Family Foundation. HIV/AIDS Fact Sheet. [Internet]. [Cited 2010]. Palo Alto: Kaiser Family Foundation. [Retrieved on December 12, 2012]. Available from: http://www.kff.org/hivaids/upload/6007-07.pdf. [ Links ]
3. Sanchez M, Lemp G, Magis-Rogriguez C, et al. The epidemiology of HIV among Mexican migrants and recent immigrants in California and Mexico. J Acquir Immune Defic Syndr 2004; 37 Suppl 4: S204-214. [ Links ]
4. Carrillo H, Fontdevila J, Brown J, et al. Risk Across Borders: Sexual Contexts and HIV Prevention Challenges among Mexican Gay and Bisexual Immigrant Men. [Internet]. San Francisco: UCSF. [Cited 2008]. [Retrieved on December 12, 2012]. Available from: http://caps.ucsf.edu/uploads/projects/Trayectos/monograph/index.html. [ Links ]
5. Minkler M, Wallace S, MacDonald M. The Political Economy of Health: A Useful Theoretical Tool for Health Education Practice. Int Quart of Com Health Ed. 1995; 15(2): 111. [ Links ]
6. Diaz RM. Latino Gay Men and HIV: Culture, Sexuality, and Risk Behavior. 1998; New York: Routledge. [ Links ]
7. Diaz R, Ayala G. National Gay and Lesbian Task Force Report: Social Discrimination and Health, the Case of Latino Gay Men and HIV Risk. [Internet]. 2001. Washington, DC: The Policy Institute of the National Gay and Lesbian Task Force. [Retrieved on December 12, 2012]. Available from: http://www.thetaskforce.org/reports_and_research/social-discrimination-and-health-case-latino-gay-men-and-hiv-risk. [ Links ]
8. Organista K, Carrillo C, Ayala G. HIV prevention with Mexican migrants: review, critique, and recommendations. J Acquir Immune Defic Syndr. 2004; 37 Suppl 4: S227-S239. [ Links ]
9. Poundstone K, Strathdee S, Celentano D. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev 2004; 26: 22-35. [ Links ]
10. Magis-Rodriguez C, Lemp G, Hernandez M, et al. Going North: Mexican migrants and their vulnerability to HIV. J Acquir Immune Defic Syndr. 2009 51 Suppl 1: S21-S25. [ Links ]
11. Ryan C, Huebner D, Diaz R, et al. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics 2009; 123(1): 346-352. 26 [ Links ]
12. Freire P. Pedagogy of the Oppressed. 1970. New York: Continuum Books. Translated by Myra Bergman Ramos. [ Links ]
13. Paiva V. Analyzing sexual experiences through 'scenes': a framework for the evaluation of sexuality education. Sex Education: Sexuality, Society and Learning 2005; 5(4): 345-358. [ Links ]
14. Fisher J, Fisher W. Changing AIDS-risk behavior. Psychological Bulletin 1992; 111(3): 455-474. [ Links ]
15. Fisher J, Fisher W. Theoretical Approaches to Individual-Level Change in HIV Risk Behavior. Handbook of HIV Prevention. Peterson JL, DiClemente RJ (Eds). 2000; New York, Plennum: 3-55. [ Links ]
16. Montedori A, Bonacini MI, Casazza G, Luchetta ML, Duca P, Cozzolino F, Abraha I. Modified versus standard intention-to-treat reporting: are there differences in methodological quality, sponsorship, and findings in randomized trials? A cross-sectional study. Trials 2011; 28 (12): 58. [ Links ]
17. Cass, V. Homosexual identity formation: A theoretical model. Journal of Homosexuality 1979; 4 (3) 219-235. [ Links ]
Received on: April 18, 2012
Accepted on: May 28, 2013
 Corresponding author:
Corresponding author:
Rita M. Melendez.
Sexuality Studies Department,
Center for Research and Education
on Gender and Sexuality, San Francisco
State University. 835 Market Street,
Suite 524, San Francisco, CA 94103, USA.
E-mail: rita.melendez@gmail.com
Declaration of conflict of interests. The authors declare that they have no conflict of interests.













