Services on Demand
Journal
Article
Indicators
Related links
Share
Salud Pública de México
Print version ISSN 0036-3634
Salud pública Méx vol.55 suppl.3 Cuernavaca 2013
Artículo de revisión
Interventions for the treatment of obesity among children and adolescents in Latin America: a systematic review
Intervenciones para el tratamiento de la obesidad en niños y adolescentes en Latinoamérica: una revisión sistemática
Brian J Nagle, MPH,(1) Christina K Holub, PhD, MPH,(1) Simón Barquera, MD, MS, PhD,(2) Luz María Sánchez-Romero, MD, MS,(2) Christina M Eisenberg, MPH, ATC,(1) Juan A Rivera-Dommarco, MD, PhD,(2) Setoo M Mehta, MPH,(1) Felipe Lobelo, MD, PhD,(3) Elva M Arredondo, PhD,(1) John P Elder, PhD, MPH.(1)
(1) Institute for Behavioral and Community Health, San Diego State University. San Diego, CA, EUA.
(2) Instituto Nacional de Salud Pública. Cuernavaca, Morelos. México.
(3) Global Health Promotion Office, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. Atlanta, GA, EUA.
Abstract
Objective. The objective of this systematic literature review was to identify evidence-based strategies associated with effective healthcare interventions for prevention or treatment of childhood obesity in Latin America.
Materials and methods. A systematic review of peer-reviewed, obesity-related interventions implemented in the healthcare setting was conducted. Inclusion criteria included: implementation in Latin America, aimed at overweight or obese children and evaluation of at least one obesity-related outcome (e.g., body mass index (BMI), z-score, weight, and waist circumference, and body fat).
Results. Five interventions in the healthcare setting targeting obese children in Latin America were identified. All five studies showed significant changes in BMI, and the majority produced sufficient to large effect sizes through emphasizing physical activity and health eating.
Conclusion. Despite the limited number of intervention studies that treat obesity in the healthcare setting, there is evidence that interventions in this setting can be effective in creating positive anthropometric changes in overweight and obese children.
Key words: overweight; quality of health care; child; adolescents; intervention studies; review.
Resumen
Objetivo. El objetivo de esta revisión sistemática de la literatura fue identificar estrategias basadas en evidencia asociadas con intervenciones en salud efectivas para la prevención y el tratamiento de la obesidad infantil en Latinoamérica.
Material y métodos. Se realizó una revisión sistemática por pares de intervenciones relacionadas con la obesidad, que fueron llevadas a cabo en clínicas de atención para la salud. Criterios de inclusión: implementadas en Latinoamérica, dirigidas a niños con obesidad y sobrepeso y evaluación de por lo menos un resultado relacionado con obesidad (ej. índice de masa corporal (IMC), puntaje Z, peso, circunferencia de cintura o grasa corporal).
Resultados. Se identificaron cinco intervenciones dirigidas a niños obesos en clínicas de salud en Latinoamérica. Todas las intervenciones mostraron cambios significativos en IMC y la mayoría obtuvo un tamaño del efecto grande a través de la promoción de actividad física y alimentación saludable.
Conclusión. A pesar del número limitado de estudios de intervención para tratar la obesidad en clínicas de salud, existe evidencia que las intervenciones en estos lugares pueden ser efectivas en alcanzar cambios antropométricos positivos en los niños con obesidad y sobrepeso.
Palabras clave: obesidad; clínica de salud; niños; adolescentes; intervención; revisión.
Globalization is the increase in a country's exchange of "capital, technology, goods, and services" with other countries in the global market, and includes public health issues such as the spread of obesity throughout Latin America.1 Surveillance of trends in the prevalence of the childhood obesity epidemic is limited, inconsistent or unavailable in some Latin American countries. Data collected in Bolivia, Brazil, Colombia, Mexico, Paraguay and Peru place overweight ranges for children from 12.2 to 23.9% and childhood obesity estimates from 1.8 to 4.7%.2 Latin American countries have some of the highest rates of overweight preschool-aged children, and, as a whole, Latin America had the largest proportion of overweight preschoolers, compared to African and Asian developing countries.3 Results from national health surveys from 71 countries suggest that the proportion of overweight and obese preschoolers in Latin America is approaching proportions found in the US with greater than 20% of children overweight in some Latin American countries.4 Rates of obesity for children 5 to 17 years old in Brazil are 21.1% for girls and 23.1% for boys, 29% for girls and 28.1% for boys in Mexico, and 27.1% for girls and 28.6% for boys in Chile5 In Colombia, rates increased from 10.3% to 17.5%, between 2005 and 2010.6
In countries where prospective data are available increases in the prevalence of obesity have been found, especially in areas that are more developed.2,7 The increase in obesity prevalence is believed to be related to globalization and progression through the epidemiological transition from acute infectious diseases to chronic diseases, adoption of a Westernized diet, and decreased opportunities for regular physical activity.8
There are a variety of settings in which to intervene on the childhood obesity epidemic. The healthcare setting (i.e., medical clinics) is one such example. There are a number of missed opportunities for physicians to address unhealthy behaviors, and these opportunities can be taken advantage of by recognizing the patient's salient concerns and drawing connections between the stated concerns and unhealthy behaviors.9 Focus group findings suggest that Latino parents of preschoolers would like for their child's physician to focus on nutrition and achieving healthy habits.10 Counseling, education, provision of health education materials and motivational interviewing by physicians have been found to be effective techniques in producing significant intervention effects on behavior change.11 However, intensity may be a crucial factor, as intensive counseling in combination with behavior change in diet and exercise has been shown to be effective in weight loss, but the evidence of low to moderate intensity counseling remains mixed.12 Despite general evidence supporting the use of healthcare-based interventions to increase healthy behaviors, the efficacy of healthcare interventions in Latin America to reduce obesity has not been evaluated. Studies are needed to examine whether the efficacy varies by the intensity (e.g., the number of patient visits), delivery (e.g., by whom, whether the provider was trained to deliver the intervention) and the targeted behavior (e.g., increased physical activity, calorie restricted diet).
The objective of this systematic literature review was to identify evidence-based strategies associated with effective healthcare interventions for the prevention and treatment of childhood obesity in Latin America.
Materials and methods
Search strategy
Literature data from Project GOL, a collaborative effort between staff at San Diego State University (SDSU) and Mexico's National Institute of Public Health (Instituto Nacional de Salud Pública, or INSP), was used as the source for the present review. Electronic databases were searched for peer-reviewed journal articles and dissertations published between 1965 and December 31, 2010, including PsycInfo, Medline/PubMed, CINAHL, Cochran Library, Current Controlled Trials, LILACS, Global Health, Global Index Medicus, and Web of Science.
Outcomes of interest, including body mass index (BMI), weight, waist circumference, percent body fat, overweight, and obese (and their Spanish or Portugese translations) were selected as primary key words to guide the search. Key words related to the outcome, comparison groups, Latino ethnicity, and geographical region were searched together. Studies of interventions in the US and all Latin American countries (except Caribbean countries) were included.
Study selection
The Community Guide is a resource provided by the CDC to inform and guide program and policy development, and was adapted to guide the procedures for the literature review and intervention selection.13 Potential articles' titles and abstracts were screened and evaluated for relevance.
Seven inclusion criteria were required for full text articles to be retrieved and abstracted:
1. Intervention focused on obesity-related topics (e.g., not general health promotion).
2. At least 50.0% of the study sample was Latino/Latin American participants or study results were stratified by race/ethnicity.
3. The intervention was evaluated and included obesity-related outcome measures.
4. The evaluated intervention compared people who were exposed to the intervention to those who were not exposed or exposed to varying degrees. This included pre-post and crossover designs.
5. The intervention must have been conducted in a community setting, as opposed to a laboratory. Primary care settings were included.
6. The intervention did not only focus on one-on-one health education, counseling or advice in a healthcare setting (for a single participant).
7. The intervention details and data were published in a format with viable information for abstraction and quality evaluation.
Reviewers were trained with example articles and did not begin the screening process until a 90.0% inter-rater reliability was achieved. Five reviewers (four from SDSU, one from INSP), conducted the screening process. Two independent graduate level reviewers screened and evaluated each full text articles for inclusion in the review.
Data collection and abstraction
Articles meeting the inclusion criteria were abstracted by two reviewers. The details of the intervention were entered into the Community Guide's online system for article abstraction. A third reviewer reconciled any discrepancies found between the initial two abstractions. Quality evaluation of each study (i.e., the type and number of limitations) was conducted by investigators.
Data synthesis
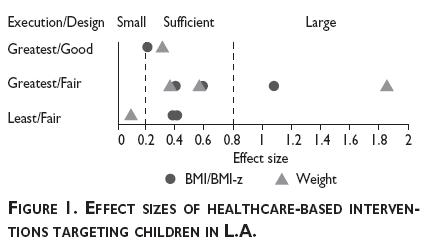
Three categories of study design suitability were used to evaluate studies: greatest (i.e., concurrent comparison groups and prospective measurement of exposure and outcome), moderate (i.e., multiple pre or post measurements, but no concurrent comparison group), and least (i.e., single pre- and post-intervention measurements and no concurrent comparison group).14 The intervention quality or "execution" was based on a possible nine limitations that are considered a threat to the study validity: 1) failure to maintain intervention integrity, 2) selection bias, 3) measurement bias, 4) misclassification bias, 5) analytic bias, 6) attrition bias, 7) confounding, 8) secular trends, and 9) any other limitations noted by the reviewers.15 Study execution was then categorized as: good (i.e., zero to one limitations), fair (i.e., two to four limitations), or limited (i.e., five or more limitations). When sufficient data was available, a Cohen's d effect size was calculated as the difference between pre- and post-treatment scores divided by the pooled pre- and post-standard deviations [d = (x1 – x2) / s]. Main outcome effect sizes were categorized into three categories: small (0.20 and below), sufficient (0.21-0.79), and large (0.80 and above).16 For pre-post designs, Cohen's d was calculated using the last follow-up measure.
Interventions were further categorized based on the target population (i.e., children or adults), whether the intervention was intended for the prevention or treatment of obesity, and the type of strategy used based on various intervention components. Component categories ranged from working with individuals to community- and policy-level changes, increasing physical activity, healthy eating behaviors, or a combination of the two. Categorization of intervention strategies allowed for the grouping of interventions with similar strategies together for comparison. For the present review, all interventions that contained at least one healthcare-based component were included.
Results
Of 325 obesity-related interventions identified in the GOL Review, 113 met the criteria for inclusion in the review and were abstracted, excluding interventions with same-source data. Investigators later excluded eight interventions due to the utilization of prescribed medications (e.g. Sibutramine) or a study sample solely comprised of mental health patients, for a final total of 105 interventions (53% conducted in the US, 23% in Mexico, 15% in Brazil, and 9% in other Latin American countries).
Of the 105 studies abstracted, four (included in the current review) were categorized by interventions delivered in the healthcare setting aimed at obese children (>95th percentile based on the CDC growth chart) in Latin America.17-20 Table I contains details of each study, including the country where the intervention was conducted, the focus and duration of the intervention, frequency of sessions, effect sizes for primary outcomes, and study designs. The total number of sessions for the entire duration of the intervention ranged, from 4 to 120 with a median of 41 sessions. Of the four studies, effect size (Cohen's d) was considered small for one intervention,20 sufficient for two interventions17,18 and large for one intervention.19 Figure 1 depicts the effect sizes for two outcomes. Study execution was based on the number of limitations identified through abstraction. One study was classified as having good execution17 and three considered fair.18-20 Study design was rated as greatest for two studies (i.e., randomized controlled trial [RCT])17,19 and least for three (i.e., pre-post design).18,20
Various healthcare settings were used to implement interventions. Apart from those interventions taking place in health clinics and medical offices, one intervention also included a home follow-up component to supplement the main healthcare-based component.18 Another unique setting was a rehabilitation facility. Most interventions were delivered by one or two health professionals (e.g., nutritionists, registered dietitians or physicians). However, one intervention utilized a multidisciplinary team.19 Intervention details are outlined in table II. All interventions targeted children considered to be obese, and one intervention had components that involved the parents.17 Sample sizes for the interventions ranged from 20 to 43 individuals, and the percentage of female participants in three studies ranged from 45 to 60%, while one study did not provide information on the gender distribution of participants.19 The average age of participants for four studies was found to be 11.5 years, with study means ranging from 9.9 to 16.9 years. One study only provided an age range for participating adolescents.20
Intervention groups in all four studies demonstrated significant improvements between pre- and post-intervention measurements. Every study had significant changes in BMI, three had significant changes in weight,17,18,20 and one had a significant change in percent body fat.17 Other significant outcomes found were BMI-z score (n=2), waist circumference (n=2) and waist-to-hip ratio (n=1). One study found significant differences between intervention and control groups at post-intervention follow-up for BMI, BMI-z score, total body fat, percent body fat, waist circumference, and weight.17 This study was a RCT delivered by registered dietitians and physicians in the clinic and medical offices. The intervention consisted of 12 weekly 2-hour group sessions and monthly consultations for the remainder of the year. Participants were provided with individualized diet plans and food guides. Physicians monitored BMI and blood pressure on a monthly basis. This study had the longest duration (12 months) of the studies in this review, and the session frequency was comparable to the other studies examined (once per week).
Discussion
This systematic literature review found sufficient evidence to recommend interventions in the healthcare setting for the treatment of obesity among Latin American youth. Out of the four interventions identified, two were RCTs and one of these RCTs showed significant results for obesity-related outcomes between intervention and control groups at post-intervention follow-up. The remaining studies (one RCT and three pre-post design) showed significant improvements between pre- and post-intervention measures.
Although the studies varied from each other, there were some commonalities between them, aside from the fact that they all took place in the healthcare setting, that may have contributed to their successes. All interventions were delivered by a healthcare professional, which may imbue the intervention with credibility. This was especially seen in Prado, et al (2010), which had the largest effect size and utilized a multidisciplinary team of professionals to address various aspects of weight loss behavioral change. Additionally, the interventions had a minimum duration of three months, and met with participants at least once a month. A majority of the interventions also incorporated components to increase both healthy eating behaviors and physical activity.
Several common limitations existed among many of the studies. The most notable was the limited number of randomized controlled studies included in our review. The remaining studies relied solely on the results of pre- and post-intervention data points, which limit the internal validity of the study (due to maturation, secular trends, etc).21 Additionally, observed anthropometric changes due to behavioral modifications could also be driven by participants' or their parents' heightened awareness of weight and other pretest anthropometric measurements.21 Another limitation was a lack of measurements for intervention exposure, such as the percent of the total sessions that individuals attended. This information could prove useful in further analysis to determine a minimum number of sessions that participants must attend to be impacted by the intervention. Finally, though less common, some interventions (n=2) used convenience sampling methods,17,19 limiting the generalizability of the findings, whereas others (n=2) relied on researcher- and self-selected sampling methods.20,18
This literature review, although extensive, also contains limitations. Interventions to reduce obesity in Latin American children that did not report obesity-related measures were not included. As such, studies that included physical activity (e.g., strength and endurance tests) or healthy eating (e.g., number of fruits and vegetables consumed per week) as primary outcomes without including obesity-related outcomes were excluded from the review. The strategies that the excluded studies implemented could potentially influence obesity outcomes. Also, this review includes only interventions from peer-reviewed literature and dissertations. It is probable that effective obesity prevention and interventions are being implemented in Latin American communities, but are not being published or even evaluated. Although we searched peer-reviewed articles from all of Latin America, intervention studies that qualified for inclusion commonly came from Mexico and Brazil, where resources may be more abundant for research and evaluation opportunities compared to other Latin American countries.
Nevertheless, based on the groundwork of this review, there is evidence that interventions in the healthcare setting can be effective in creating positive anthropometric changes in obese and overweight children in Latin America. Interventions with components to increase physical activity and healthy eating behaviors in the healthcare setting could be utilized to supplement larger obesity prevention efforts. The healthcare setting facilitates interaction with health professionals who are knowledgeable about the health effects of obesity. This particular setting also allows easy access to instruments to monitor progress with obesity-related measures (e.g., weight, BMI) and physiological measurements (e.g., blood pressure, blood glucose levels) indicative of diseases related to obesity, such as hypertension and type 2 diabetes. One limitation of this approach, however, is that it assumes that individuals have regular access to healthcare. Therefore, this setting would not be ideal for populations and communities that do not have regular access to clinics and/or do not seek out healthcare on a regular basis. Due to the limited intervention literature in Latin America within the healthcare setting, it is evident that evaluations of healthcare interventions with obesity-related outcome measures are needed. As the body of literature particular to the healthcare setting grows, those components and strategies within healthcare-based interventions that are most effective at reducing obesity should become more apparent.
In conclusion, this review not only provides evidence that the healthcare setting can be effective in preventing obesity in children, but also provides a platform for encouraging research in the development of such interventions. Although studies regarding prevention or treatment of obesity among children are limited in Latin America, as the body of literature develops, it is important to utilize reviews such as this to cultivate recommendations for further research and interventions. The need to evaluate anthropometric changes is not only of importance in ensuring intervention efficacy of reducing obesity, but also crucial as it provides information about the status of the obesity epidemic in Latin American countries.
Acknowledgments
This study was approved by the Institutional Review Board of San Diego State University and was funded by the CDC 1U48 DP001917.
References
1. Popkin BM. Technology, transport, globalization and the nutrition transition food policy. Food Policy [Internet]. 2006 Dec [cited 2011 Jun 21];31(6):554-569. Available in: http://linkinghub.elsevier.com/retrieve/pii/S030691920600039X [ Links ]
2. Filozof C, Gonzalez C, Sereday M, Mazza C, Braguinsky J. Obesity prevalence and trends in Latin-American countries. Obesity reviews : an official journal of the International Association for the Study of Obesity [Internet]. 2001 May [cited 2011 May 25];2(2):99-106. Available in: http://www.ncbi.nlm.nih.gov/pubmed/12119667 [ Links ]
3. de Onis M, Blössner M. Prevalence and trends of overweight among preschool children in developing countries. The American journal of clinical nutrition [Internet]. 2000 Oct [cited 2011 May 25];72(4):1032-1039. Available in: http://www.ncbi.nlm.nih.gov/pubmed/11010948 [ Links ]
4. Martorell R, Kettel-Khan L, Hughes ML, Grummer-Strawn LM. Overweight and obesity in preschool children from developing countries. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity [Internet]. 2000 Aug [cited 2012 Apr 14];24(8):959-967. Available in: http://www.ncbi.nlm.nih.gov/pubmed/10951533 [ Links ]
5. Sassi F,Devaux M. Obesity update 2012. [Internet] OECD 2012; 1-7.Available in: http://www.oecd.org/health/49716427.pdf [ Links ]
6. Olaiz-Fernández G, Rivera-Dommarco J, Shamah-Levy T, Rojas R, Villalpando-Hernández S, Hernández-Avila M, et al. Encuesta Nacional de Salud y Nutrición 2006. Cuernavaca, México: Instiuto Nacional de Salud Pública, 2006. [ Links ]
7. Kain J, Vio F, Albala C. Obesity trends and determinant factors in Latin America. Cadernos de saúde pública / Ministério da Saúde, Fundação Oswaldo Cruz, Escola Nacional de Saúde Pública [Internet]. 2003 Jan [cited 2011 May 25];19 Suppl 1:S77-S86. Available in: http://www.ncbi.nlm.nih.gov/pubmed/12886438 [ Links ]
8. Fraser B. Latin America's urbanisation is boosting obesity. Lancet [Internet]. 1995 [cited 2011 May 25];365(9476):1995-1996. Available in: http://www.ncbi.nlm.nih.gov/pubmed/15954218 [ Links ]
9. Cohen DJ, Clark EC, Lawson PJ, Casucci B, Flocke S. Identifying teachable moments for health behavior counseling in primary care. Patient education and counseling [Internet]. 2011 Nov [cited 2012 May 24];85(2):e8-e15. Available in: http://www.ncbi.nlm.nih.gov/pubmed/21183305 [ Links ]
10. McKee MD, Maher S, Deen D, Blank AE. Counseling to prevent obesity among preschool children: acceptability of a pilot urban primary care intervention. Annals of family medicine [Internet]. 2010 [cited 2012 May 24];8(3):249-255. Available in: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2866723&tool=pmcentrez&rendertype=abstract [ Links ]
11. Sargent GM, Pilotto LS, Baur L. Components of primary care interventions to treat childhood overweight and obesity: a systematic review of effect. Obesity reviews : an official journal of the International Association for the Study of Obesity [Internet]. 2011 May [cited 2011 May 25];12(5):e219-e235. Available in: http://www.ncbi.nlm.nih.gov/pubmed/20630025 [ Links ]
12. Cabodi J, Kelsberg G, Safranek S. Clinical inquiry: does brief physician counseling promote weight loss? The Journal of family practice [Internet]. 2011 Sep [cited 2012 May 24];60(9):548-550. Available in: http://www.ncbi.nlm.nih.gov/pubmed/21901183 [ Links ]
13. CDC. The Community Guide Home Page [Internet]. 2011 [cited 2011 Aug 8]; Available in: www.thecommunityguide.org/index.html [ Links ]
14. Briss PA, Zaza S, Pappaioanou M, Fielding J, Wright-De Agüero L, Truman BI, et al. Developing an evidence-based Guide to Community Preventive Services--methods. Am J Prev Med. 2000 Jan;18(1 Suppl):35-43. [ Links ]
15. Zaza S, Wright-De Agüero LK, Briss PA, Truman BI, Hopkins DP, Hennessy MH, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Task Force on Community Preventive Services. American journal of preventive medicine [Internet]. 2000 Jan [cited 2012 Apr 23];18(1 Suppl):44-74. Available in: http://www.ncbi.nlm.nih.gov/pubmed/10806979 [ Links ]
16. Morris SB. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. The British journal of mathematical and statistical psychology [Internet]. 2000 May [cited 2012 Mar 28];53 ( Pt 1):17-29. Available in: http://www.ncbi.nlm.nih.gov/pubmed/10895520 [ Links ]
17. Díaz RG, Esparza-Romero J, Moya-Camarena SY, Robles-Sardín AE, Valencia ME. Lifestyle intervention in primary care settings improves obesity parameters among Mexican youth. Journal of the American Dietetic Association [Internet]. 2010;110(2):285-290. Available in: http://libproxy.sdsu.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2010557220&site=ehost-live [ Links ]
18. Velázquez-López L, Rico-Ramos J, Torres-Tamayo M, Medina-Bravo P, Toca-Porraz L, Escobedo-de la Peña J. [The impact of nutritional education on metabolic disorders in obese children and adolescents]. Endocrinol Nutr. 2009;56(10):441-446. [ Links ]
19. Prado DM, Silva AG, Trombetta IC, Ribeiro MM, Nicolau CM, Guazzelli IC, et al. Weight loss associated with exercise training restores ventilatory efficiency in obese children. International journal of sports medicine [Internet]. 2009 Nov [cited 2011 Jul 18];30(11):821-826. Available in: http://www.ncbi.nlm.nih.gov/pubmed/19685411 [ Links ]
20. Dâmaso AR, Tock L, Tufik S, Prado WL, Stella SG, Fisberg M, et al. Tratamento multidisciplinar reduz o tecido adiposo visceral, leptina, grelina e a prevalência de esteatose hepática não alcoólica (NAFLD) em adolescentes obesos. Revista Brasileira de Medicina do Esporte [Internet]. 2006 Oct;12(5):263-267. Available in: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1517-86922006000500008&lng=pt&nrm=iso&tlng=pt [ Links ]
21. Mitchell M, Jolley J. Problems with the Pretest-Posttest Design. In: Research Design Explained. Fort Worth: Harcourt College Publishers, 2001:157-164. [ Links ]
Received on: July 4, 2012
Accepted on: November 5, 2012
 Correspondence author:
Correspondence author:
Brian J. Nagle.
Institute for Behavioral and Community Health 9245 Sky Park Ct, Suite 221, San Diego, CA 92123, USA.
E-mail: naglebj@gmail.com
Declaration of conflict of interests: The authors declare not to have conflict of interests.













