INTRODUCTION
Kidney replacement therapy (KRT) in Latin America (LA) started as peritoneal dialysis (PD) in Brazil in 1947. Shortly thereafter, the first hemodialysis (HD) was also accomplished in Brazil (in 1949) and the first kidney transplant (KT) in Argentina (in 1956)1-3. Initially, HD was considered exclusively as a therapy to support patients with acute kidney injury and who were awaiting kidney transplantation, but it quickly became incorporated as treatment for end-stage kidney disease (ESKD). The field of clinical nephrology developed almost simultaneously, with physicians and researchers consolidating into national nephrology societies, such as those of Argentina (in 1960), Brazil (in 1960), Chile (in 1964), and Uruguay (in 1967)3.
The Latin American Nephrology and Hypertension Society (Sociedad Latinoamericana de Nefrología e Hipertensión [SLANH]) was created in 1970, grouping the various national nephrology societies of 20 countries (i.e., Argentina, Bolivia, Brazil, Chile, Colombia, Costa Rica, Cuba, Dominican Republic, Ecuador, El Salvador, Guatemala, Honduras, Mexico, Nicaragua, Panama, Paraguay, Peru, Puerto Rico, Uruguay, and Venezuela). In 1991, the SLANH founded the LA Dialysis and Renal Transplant Registry to promote the knowledge and improve the care of chronic kidney disease (CKD) in KRT by collecting and analyzing data from the 20 member countries. The Registry office was housed in Montevideo (Uruguay), until 2001, when it moved to Buenos Aires (Argentina), where it remained until 2012; since then, the coordination is shared between both cities. At present, the Registry is composed of an Executive Board and delegates from each of the nephrology societies that are part of the SLANH.
The methodology used by the LADTR has been reported before. Briefly, participant countries complete an annual survey to provide data on incident and prevalent cases of patients undergoing kidney replacement treatment (KRT) by means of all modalities (HD, PD, and living with a functioning graft [LFG]), CKD etiology, number and type of kidney transplants, percent of population under KRT coverage, and number of nephrologists, as well as other relevant parameters. Analyses of these variables are performed routinely to determine correlations with gross national income and life expectancy at birth (LEB) as well as other socioeconomic indexes4,5.
In this manuscript, we will describe the development and challenges of HD in LA in the past 10 years.
Accessibility and growth of hemodialysis in Latin America
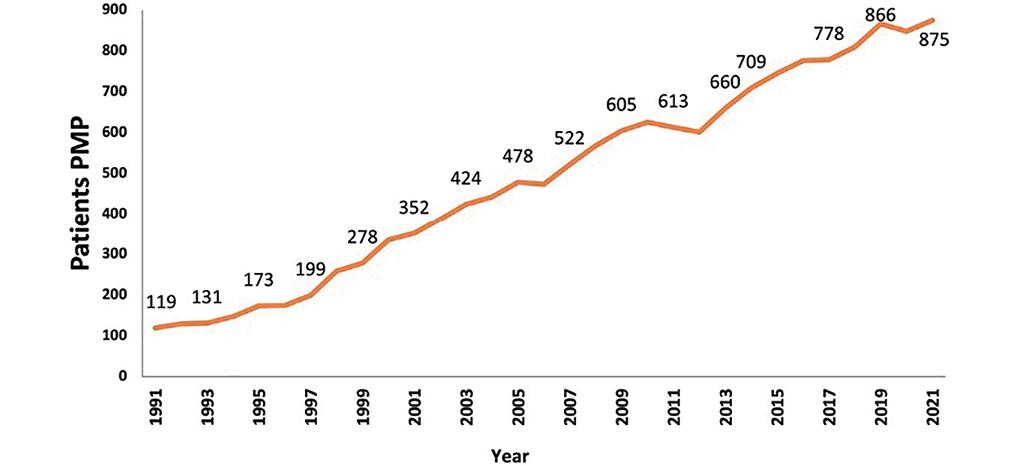
On 31 December 2021, a total of 449,683 patients were included in KRT in LA, corresponding to an overall unadjusted prevalence of 872 per million persons (pmp) (Table 1). The prevalence ranged from 2.894 pmp in Puerto Rico to 89 pmp in Nicaragua. Eleven countries showed a rate greater than 700 pmp (Argentina, Brazil, Chile, Colombia, Ecuador, El Salvador, Guatemala, the estates of Jalisco and Aguascalientes (Mexico), Panama, Puerto Rico, and Uruguay) a prevalence outlined as the main objective to reach for the region by 2019, in the joint collaboration plan signed between Pan American Health Organization (PAHO) and SLANH. In 2021, the prevalence rate resumed the progressive increase previous to the pandemic, whose deleterious effect was notorious in 2020 (848 pmp) having been 866 pmp in 2019, 810 pmp in 2018, and 778 in 2017 (Fig. 1).
Table 1. RRT prevalence, incidence, and kidney transplantation rates, 2021
| Country | Population in millions | Prevalence rate
pmp |
Incidence rate
pmp |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HD | PD | Total dialysis | LFG | Total | Total dialysis | % on PD | Kidney Tx rate | ||
| Argentina | 45808746 | 587.5 | 54.5 | 642.0 | 242.2 | 884.1 | 174.6 | 14.8 | 26 |
| Bolivia | 11216000 | 472.5 | 0.0 | 472.5 | 0.0 | 472.5 | 3 | ||
| Brazil | 213317639 | 654.5 | 41.0 | 695.5 | 295.3 | 990.8 | 224.5 | 22 | |
| Chile | 19493184 | 1238.3 | 78.0 | 1316.4 | 229.3 | 1545.6 | 137.7 | 15.9 | 12 |
| Colombia | 50710960 | 498.1 | 190.0 | 688.1 | 154.1 | 842.3 | 75.1 | 41.9 | 17 |
| Costa Rica | 5153957 | 44.8 | 143.8 | 188.6 | 224.5 | 413.1 | 21.1 | 88.1 | 6 |
| Cuba | 11200000 | 254.3 | 4.4 | 258.7 | 89.3 | 347.9 | 128.7 | 0 | |
| Ecuador | 17797737 | 991.9 | 56.6 | 1048.5 | 81.5 | 1130.0 | 210.6 | 7.2 | 5 |
| El Salvador | 6321042 | 443.0 | 439.3 | 882.3 | 1.6 | 883.9 | 65.5 | 4 | |
| Guatemala | 17109746 | 652.8 | 274.1 | 926.9 | 72.4 | 999.3 | 164.2 | 22.0 | 3 |
| Honduras | 9304380 | 462.1 | 22.0 | 484.2 | 13.0 | 497.2 | 95.8 | 0 | |
| Jalisco/Aguascalientes (Mex) | 9944258 | 609.5 | 419.6 | 1029.1 | 708.9 | 1738.0 | 585.4 | 11.4 | 68 |
| Nicaragua | 6851000 | 32.1 | 52.1 | 84.2 | 5.1 | 89.3 | 29.9 | 85.9 | 0 |
| Panama | 4395414 | 501.9 | 107.6 | 609.5 | 96.7 | 706.2 | 158.6 | 26.0 | 10 |
| Paraguay | 7353038 | 294.7 | 14.4 | 309.1 | 41.8 | 350.9 | 45.7 | 2.1 | 4 |
| Peru | 33715471 | 487.1 | 5.5 | 492.6 | 44.2 | 536.8 | 86.7 | 2.4 | 1 |
| Puerto Rico | 3200000 | 1989.7 | 186.3 | 2175.9 | 717.8 | 2893.8 | 21 | ||
| Dominican Republic | 11000000 | 304.5 | 84.5 | 389.1 | 45.5 | 434.5 | 159.5 | 21.5 | 4 |
| Uruguay | 3543025 | 931.7 | 84.4 | 1016.1 | 371.7 | 1387.8 | 176.7 | 9.3 | 26 |
| Venezuela | 28199867 | 255.3 | 14.2 | 269.5 | 180.6 | 450.1 | 1 | ||
| Total LA | 515635464 | 596.4 | 76.4 | 672.8 | 199.3 | 872.1 | 179.2 | 6.2 | 16 |
HD: hemodialysis; PD: peritoneal dialysis; LFG: living with a functioning kidney graft; NR: not reported; KRT: kidney replacement treatment; Tx: transplant; pmp: patients per million population; LA: Latin America.
By treatment modality, 68% of the prevalent patients were treated by HD (n = 307.514) and 9% by PD (39.397) and 23% of the patients had a living functional graft (n = 102.772). HD continues to be the most prevalent modality over the years. While PD reached a plateau on its prevalence, KT increased steadily throughout the past 10 years (Fig. 2). HD was the most frequent modality in all countries except in Costa Rica, where LFG reached 224 pmp and PD 144 pmp while HD only 45 pmp. Considering both dialysis modalities together, these were more frequent compared to LFG in the region as a whole and in each country separately. Puerto Rico should be highlighted as the region with the highest prevalence of LFG (718 pmp) (Fig. 3).

Figure 2. Unadjusted prevalence rates per million population (pmp) of patients in kidney replacement therapy by modality.

Figure 3. Unadjusted prevalence rates per million population (pmp) of patients under renal replacement therapy, by treatment modality.
In 2021, 92,411 patients started KRT in LA, representing a total unadjusted incidence rate of 179 pmp (Table 1). The majority of the patients started KRT in HD modality while only 6% in PD. PD represented more than 10% of the incident modality in only nine countries (Jalisco/Aguascalientes [in Mexico] 11%, Argentina 15%, Chile 16%, Dominican Republic and El Salvador 22%, Panama 26%, Colombia 42%, Nicaragua 86%, and Costa Rica 88%).
Kidney transplant rate in the region was 16 pmp, varying from countries with rates close to 1 pmp in Peru and Venezuela to 68 pmp, as is the case of Jalisco/Aguascalientes (Table 1).
The total prevalence of KRT correlated positively with gross domestic product per capita and LEB (Fig. 4A and B).
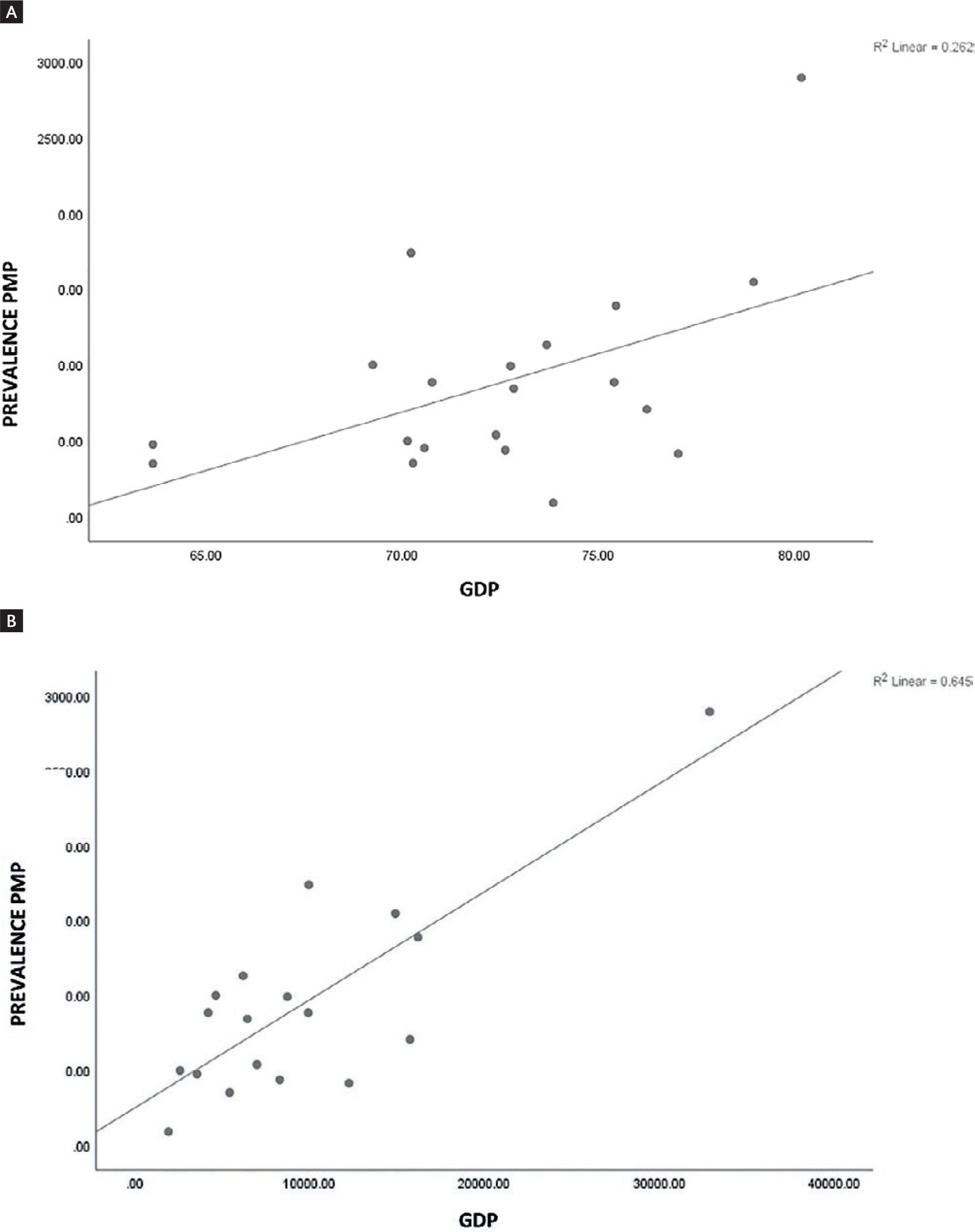
Figure 4. (A) Association between gross domestic product per capita and prevalence of KRT pmp. (B) Association between life expectancy at birth and prevalence of KRT per pmp.
Finally, great heterogeneity was reported in the number of nephrologist/population rate, from 3 pmp in Honduras to 52 pmp in Uruguay. Only Argentina, Brazil, Cuba, Ecuador, Puerto Rico, and Uruguay have more than 20 nephrologist pmp.
Fourteen countries reported data for mortality showing a significant heterogeneity between them. The overall unadjusted mortality rate was 17%.
Development of renal registries in Latin America
A patient registry is an organized system that applies methodology derived from observational studies to collect standardized data (clinical records and others) to evaluate specific results. Collected information is used to achieve predetermined scientific, clinical, or health policy purposes, such as describing the natural history and rising awareness of the disease, estimating the clinical and cost-effectiveness relationship of the products of healthcare services, and measuring or monitoring the risk profile and patient safety, as well as evaluating the quality of healthcare6-8.
The implementation of a registry of patients with CKD (including all stages in the progression of disease) is difficult to achieve, given the high costs involved. On the other hand, patients with ESKD are easily accessible and constitute the most severe subgroup in terms of comorbidities and healthcare costs9.
A KRT registry (KRTR) involves the systematic and continuous collection of a population-based data set of patients with ESKD who are treated with dialysis or kidney transplant (KT). In this way, the KRTR represents a useful tool for epidemiological research and planning and improvement in quality of care, as well as enabling countries to monitor and evaluate the progress made. Moreover, it allows estimation of the impact of interventions on patients in their previous stages of CKD, and accordingly, planning of health-care policies to prevent disease progression. To that end, having good-quality records make it possible to set up the databases required to carry out such analyses. From this perspective, the capacity of a KRTR to achieve these objectives is based on the quality of its data and on the control procedures used to obtain quality information9-11.
The lack of available data, particularly in emerging economies, leaves information gaps in health care and outcomes in patients with kidney disease12. The heterogeneity, or even the absence, of KRTRs in some countries is consistent with the inequities in access to KRT for patients with ESKD worldwide11,12. Many low- and middle-income countries (and also some high-income countries) do not have kidney registries yet, and if they do, the registries collect data on an incomplete and voluntary basis and at an aggregate level. In response to this inequality, various actions have been carried out at regional, as well as global, levels.
In 2014, the PAHO proposed to reach the prevalence of patients on dialysis for at least 700 patients per million inhabitants by 2019 in every LA country. Since then, PAHO and the SLANH have been providing training and certification courses for national delegates and workshops to strengthen the national registries and regional workshops to evaluate results and planning activities, with participation of representatives of all the 20 countries of SLANH13.
In this setting, the event included the participation of at least one representative of PAHO, a representative of the Ministry of Health, a representative of the National Society of Nephrology, and the current or potential delegates of the National Registry in each country. A visit to a dialysis centre (possibly public), where the case report originates for registration, and there was practical teaching activity of evaluation in situ with local actors. The preliminary results were variable and not uniform. There was a concordance between the characteristics of each country of the region and the results. The outcome always depended on the strength of the relationship between each of the main stakeholders: the National Nephrology Societies, the Ministry of Health, and the Social Security administration. Overall results also depended on the political scenario and continuity of the health-care policies.
In 2017, in Panama, it was possible to verify the progress in the construction and operation of the National Registries of almost all the participating countries, according to a novel classification of categories of registries by complexity and data quality13 (Table 2). PAHO and LARDRT provided technical support to a group of countries that showed significant progress (Dominican Republic, Panama, and El Salvador) and others that showed modest progress (Guatemala, Peru, Mexico, Paraguay, and Ecuador). The registries of Mexico and Brazil were still partial and did not cover the entire country. Honduras, Bolivia, and Costa Rica suggested little or no progress. The registries with the highest qualification were those from Argentina, Colombia, and Puerto Rico, followed by Uruguay and Cuba.
Table 2. Categories of registries by complexity and data quality
| 1 | There is no basic type of dialysis and/or kidney transplant systematic registry. |
| 2 | There are only partial (institutional/regional) systematic records of dialysis and/or kidney transplantation, not subject to quality control and not mandatory. |
| 3 | There is a systematic population-based national registry of dialysis and/or kidney transplantation, which collects basic data (incidence, prevalence, and mortality), based on efforts of non-governmental organizations or health-care providers (scientific societies and health-care institutions). 3A: with < 90% of the patients registered; 3B: with > 90% of the patients registered. |
| 4 | The registration of dialysis and transplantation is national in scope, with > 90% of the patients registered, is multi-institutional, covers the entire population and all techniques of renal replacement and performs an annual report of basic data. |
| 5 | The registration of dialysis and transplantation is national in scope, with > 90% of the patients registered, is regulated by legislation, norms or ministerial decrees, and is multi-institutional. It collects basic, evolutionary data and includes quality control of the provision. It produces an annual report in which the results of the treatment, the quality of the service, and the performance of the providers are detailed. |
Despite these efforts, although the situation of KRTRs has improved in LA, the heterogeneity and inequities in their development still remain. Table 3 shows the current situation of the national LA dialysis and transplant registries, recently presented at the World Congress of Nephrology (Thailand, 2023).
Table 3. Situation of the national LA dialysis and transplant registries, recently presented at the World Congress of Nephrology (Luxardo, 2023)15
| Country | Character | National | Type | Completeness | Digital | Category |
|---|---|---|---|---|---|---|
| Argentina | Mandatory | X | Patient | > 90 | X | 5 |
| Bolivia | NO Registry | Center | Only SS 32% | 1 | ||
| Brazil | Voluntary | X | Center | ≤ 50 | X | 3 |
| Chile | Voluntary | X | HD: centers/ DP y TR: patient | > 90 | 3 | |
| Colombia | Mandatory | X | Patient | > 90 | X | 5 |
| Costa Rica | Mandatory | X | Patient | > 90 | X | 2 |
| Cuba | Mandatory | X | Patient | > 90 | 4 | |
| Ecuador | Mandatory | X | Center | > 90 | X | 2 |
| El Salvador | Mandatory | X | Patient | > 90 | X | 3 |
| Guatemala | Mandatory | X | Patient | Only SS > 90 | X | 3 |
| Honduras | NO Registry | Center | > 90 | 1 | ||
| Aguascalientes (MX) | Voluntary | Center | > 90 | X | 2 | |
| Jalisco (MX) | Mandatory | Center | > 90 | X | 2 | |
| Nicaragua | NO Registry | Center | > 90 | 1 | ||
| Panama | Mandatory | X | Patient | Only SS 84% | X | 2 |
| Paraguay | Mandatory | X | Patient | > 90 | 3 | |
| Peru | Voluntary | Patient | Only SS 77% | X | 1 | |
| Puerto Rico | Voluntary | X | Patient | > 90 | X | 3 |
| Dominican Rep. | Mandatory | X | Patient | > 90 | X | 3 |
| Uruguay | Mandatory | X | Patient | > 90 | X | 4 |
| Venezuela | Voluntary | X | Center | > 90 | 1 |
KRT: kidney replacement treatment; LA: Latin America; HD: hemodialysis.
HEMODIALYSIS TECHNOLOGY IN ACUTE KIDNEY INJURY AND CHRONIC KIDNEY DISEASE
There are few reports in the literature that describes the type of KRT used for acute kidney injury (AKI) in LA. With this goal in mind, the AKI Committee of the SLANH conducted a survey in 2014, which for the first time provided information on the infrastructure, human resources, and equipment available for KRT in AKI patients in the region14. Although 246 units from 14 countries responded to the survey, the vast majority (220 units) came from only five countries, namely Argentina, Brazil, Uruguay, Chile, and Peru. This heterogeneous response was likely related to many aspects, including population size, socioeconomic development, health system organization, and the presence of an active national nephrology society. The authors found that the majority of patients were treated in units managed by the nephrology divisions of teaching hospitals. Economic support was mostly provided by public health systems. Intermittent HD (IHD) was universally performed by all of the units, whereas 40% performed prolonged intermittent renal replacement therapies (PIRRTs) and only 23% provided continuous renal replacement therapies (CRRTs). These past two techniques were mainly available in larger units14. More recently, the EPILAT-IRA study, an observational study performed to understand the epidemiology of AKI in LA, showed that the most common type of KRT performed was IHD (68%), followed by PIRRT (22%), CRRT (10%), slow continuous ultrafiltration (8%), and PD (5%). Several patients received more than one type of KRT. Reasons for initiation of KRT were electrolyte and/or acid-base disturbances (70%), fluid overload (54%), and solute control (48%)16,17.
The COVID pandemic prompted further development of CRRT and adsorption therapies in critically ill patients with AKI in LA17.
Regarding HD in patients with CKD, the technological development of recent years has ensured a better quality of water treatment, enabling perform convective treatments such as high-flux HD and high-volume online hemodiafiltration (HVHDF). The development of online HVHDF techniques using the dialysis fluid itself as a replacement fluid was achieved through dialysis machines modified to perform online HVHDF, incorporating safety filters to ensure the quality of this replacement fluid (ultrapure dialysate). Studies carried out in developed countries have shown the superiority of online HVHDF over conventional HD18,19.
Online HVHDF is a growing technique in LA, and in some countries like Argentina, it has become the most frequent dialysis technique, after conventional HD20. On the other hand, a survey carried out by the SLANH HD committee in 2021 showed that only 38% of HD units in LA practiced HVHDF online. Likewise, those surveyed highlighted as the greatest barriers to developing this practice, its cost, and non-recognition by funders.
Technological advances reach the LA region; however, more cost-effective dialysis techniques such as PD are not expanding and when performed, and they are not adequately applied.
CONCLUSIONS
In the past 10 years, hemodialysis is the KRT that has had the greatest growth in LA, in terms of incidence and prevalence, as well as in the incorporation of technology. However, this does not mean that full accessibility has been achieved for all patients, LA shows heterogeneity between the various countries, including for PD and kidney transplantation, as well as for renal dialysis registries. A similar situation is observed for renal dialysis registries, where some countries have few efforts for implementation. PD is an underutilized dialysis modality in most countries in the region, and many countries do not have the desired number of nephrologists. SLANH has played and will play an important role in the challenge of improving these inequalities.











 text new page (beta)
text new page (beta)