INTRODUCTION
SARS-CoV-2 continues to cause a worldwide pandemic associated with important morbidity and mortality, especially among vulnerable groups. As of February 28, 2022 (cutoff point of this report), almost 435 million confirmed cases of COVID-19 and almost 6 million associated deaths had been documented1. Such a burden could rise with reinfections, although the previous reports estimated this occurrence to be rare2-4. Reinfection rates have been estimated in 2.18 per 100 person-years in vaccinated health care workers5 and 2.46 per 100,000 persons per day in vaccinated patients6; however, updates considering the effect of the Omicron wave are lacking. This is relevant for several reasons: a worldwide surge has been caused by the Omicron variant and its subvariants1; waning of immunity may occur over time7; and the odds of reinfection with the Omicron variant and its subvariants are higher8, largely due to their immune-escaping properties9-10. Hospital workers are considered highly exposed individuals, and an estimation of the changes in the reinfection risk along the course of the pandemic is needed. This study reports the reinfection rate in a cohort of hospital workers considering the surge of infections caused by the SARS-CoV-2 Omicron variant.
METHODS
This is a prospective cohort study in a Mexico City tertiary hospital. A waiver for approval by the Institutional Review Board was granted for this study due to its epidemiologic nature, a no greater than minimal risk for study subjects, and the use of deidentified data after database completion and coding.
All hospital workers who voluntarily received on-site medical consultation at no cost between March 1, 2020, and February 28, 2022, due to symptoms suggestive of COVID-19 were followed. Suggestive symptoms included any of the following: (a) one highly suggestive symptom (headache, cough, or fever), with or without (b) two or more other symptoms (malaise, rhinorrhea, nasal congestion, throat pain, myalgias, arthralgias, diarrhea, nausea, or vomiting). COVID-19 episodes were confirmed by either a positive PCR test (NucliSens easyMAG system, bioMérieux, Boxtel, Netherlands [nucleic acid extraction]; and Applied Biosystems 7500 thermocycler, Applied Biosystems, Foster City, CA, USA [real-time reverse-transcription PCR]), or a positive antigen test (Panbio™ COVID-19 Ag Rapid Test Device, Abbott, Jena, Germany). The following was recorded for every study subject: name, sex, age, health care worker type, symptom onset date(s), diagnostic test results, and vaccination history (dates of primary series and boosters). A stratified analysis of clinical workers (physicians, nurses, laboratory workers, and stretcher bearers) was also conducted.
Reinfection was defined as the occurrence of two or more COVID-19 episodes separated by an intercurrent period of ≥ 90 days without symptoms (sequencing of SARS-CoV-2 was not performed during this period). Therefore, only subjects with ≥ 90 days of follow-up were included in the calculation of the reinfection rate (number of reinfection events divided by the sum of persons per day, multiplied by 100,000). For the calculation of persons per day, the number of days between COVID-19 episodes (subjects with reinfection) and the number of days between symptom onset date and February 28, 2022 (subjects with one COVID-19 episode), were added. Time (in days) between a complete primary vaccination series (≥ 14 days after the last dose) or booster (≥ 14 days) and COVID-19 episodes, as well as time between COVID-19 episodes, was summarized using medians and ranges.
Statistical analysis
Excel version 13 (Microsoft Office Professional Plus) and Stata version 14 (Stata-Corp, College Station, TX, USA) were used in analyses. For comparisons, either the Chi-square or Fisher’s exact test was used, and p ≤ 0.05 was considered statistically significant. A subject was excluded from analysis if the test result or symptom onset date was missing. When the day was missing in the vaccination date, the 1st day of the month was assumed, but the date was left blank if any other value was missing.
RESULTS
During the study period, 3732 medical consultations were provided to 2700 study subjects, of whom 1641 (60.8%) were female, 1323 of 2626 (50.4%) were clinical workers (of whom 634 were nurses and 595 were physicians), and 2405 (89.1%) had completed their primary vaccination series. The majority of subjects received one (n = 1945) or two (n = 553) consultations. In total, 1754 subjects (65.0%) were infected after December 28, 2022 (start of boosting in hospital workers), 942 (53.7%) of whom had had a vaccine booster. Test results were missing in 38 subjects (1.0%); after exclusion, 1388 COVID-19 cases were left, of which 721 (51.9%) were cases detected during December 2021 and beyond (Omicron wave) and 73 (5.6%) were reinfection cases. Five non-vaccinated subjects died due to COVID-19 (none were reinfection cases). The hospital epidemic curve was similar to the one observed in Mexico City (10) (Fig. 1A and B).
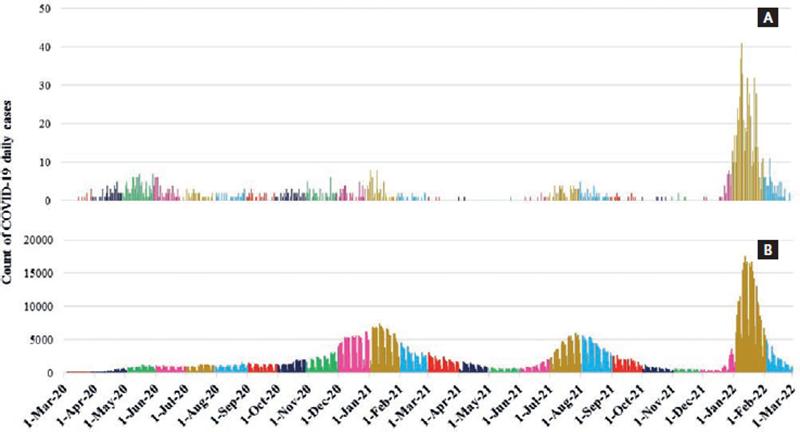
Figure 1. Epidemic curve of COVID-19 cases in: (A) hospital workers of our institute and (B) Mexico City population, March 2020-February 2022.
A comparison between groups (one infection vs. reinfection) is shown in table 1. Groups were similar, except for greater age, a higher adherence to the primary vaccine series and a higher proportion of nurses (38.4% vs. 23.8%, p = 0.0048) and kitchen workers (5.5% vs. 1.4%, p = 0.0091) in the reinfection group.
Table 1. Comparison between groups (one SARS-CoV-2 infection vs. reinfection)
| Variable | One infection (n = 1242) | Reinfection (n = 73) | p |
|---|---|---|---|
| Age (median, range) | 34 (19-90) | 39 (24-72) | 0.0108 |
| Female sex (n, %) | 739 (59.5) | 50 (68.5) | 0.1277 |
| Clinical workers (n, %) | 597 (48.1) | 40 (55.0) | 0.2635 |
| Primary vaccination series (n, %) | 1102 (88.7) | 71 (97.3) | 0.0224 |
Follow-up comprised a total of 316,276 persons per day (median = 494 days, range = 99-712 days) in 662 subjects with COVID-19 (47.7%). The global reinfection rate was 23.1 per 100,000 persons per day. Before December 2021, five reinfection cases had been documented among 258,683 persons per day (reinfection rate of 1.9/100,000 persons per day).
A median of 487 days (range = 99-664) elapsed between episodes in reinfected subjects. In seven of these subjects, there was a median of 112 days (range = 26-181) between the primary vaccine series and the first infection episode (all other cases had been infected before vaccination); in 68 subjects, the corresponding value between the primary vaccine series and the reinfection episode was 323 days (range = 73-374). Twenty-two subjects with reinfection (30.1%) had a booster completed before the second episode (median of 6 days before reinfection, range = 0-33).
DISCUSSION
In this study with a long follow-up, the reinfection rate of SARS-CoV-2 rose substantially (by a factor of 12) during the Omicron wave in a cohort of vaccinated hospital workers, although cases were mild. This rate was substantially higher than that reported previously5,6, partly due to some differences, as shown in table 2. Although a clear-cut distinction between hospital- and community-acquired cases cannot be made in this study, the similarity of the epidemic curve of our hospital’s health care workers and the curve for Mexico City, in addition to our hospital’s mask mandate, supports a higher probability of acquisition in the community. In fact, the previous reports have estimated that the majority of infections identified among hospital workers were possibly acquired in the community12-14.
Table 2. Comparison of studies that have reported reinfection rates
| Variable | Malhotra et al.5 | Hammerman et al.6 | Current study |
|---|---|---|---|
| Country | India | Israel | Mexico |
| Population | Hospital workers (clinical and non-clinical) – one center | Patients of health-care organization | Hospital workers (clinical and non-clinical) – one center |
| Study time period | March 3, 2020-June 18, 2021 | March 1, 2021-November 26, 2021 | March 1, 2020-February 28, 2022 |
| Predominant variant | Delta | Delta | Omicron |
| Participants with past episode (n) | 1917 | 149,032 | 1388 |
| Mean/median age (years) | 36.6 | 39.3 | 35 |
| Female sex (%) | 42.3 | 54.5 | 60 |
| Vaccinated subjects | 56.8% with two doses | 56.0% with ≥ 1 dose | 89.8% with ≥ 2 doses |
| Reinfection rate × 100,000 persons per day (vaccinated subjects) | 6 | 2.5 | 23.1 (1.9 before December 2021) |
Although vaccination reduces reinfection risk5,15, results of this study showed that the reinfection rate increased during the Omicron wave in hospital workers that were highly compliant with vaccination; however, more information is needed regarding the protection provided by one or more booster doses. Although the exact causes behind the surge in this highly immunized population (i.e., highly compliant with the primary series, as per vaccine availability for the eligible population at the time of this study) are not totally clear, it is very possible that both the emergence of an immune-evading variant and the relaxation of non-pharmacologic preventive interventions over time (perhaps more pronounced in vaccinated individuals) played a role; nonetheless, the relative weight of these factors is currently unknown. It also remains to be studied to what extent (if any) children were involved in the transmission of the Omicron variant in Mexico, since they were not included in vaccination campaigns before and during the Omicron wave.
Aside from the individual consequences of one or more episodes of infection, the last pandemic wave disrupted medical services due to the high number of clinical workers (in this study, mainly nurses) that had to comply with leave days at home. Interestingly, nurses and kitchen workers were overly represented in the reinfection group. Although the cause of this is unclear, two factors could underlie a possible increase in reinfection risk: (1) these groups were among those most infected during the initial pandemic wave in Mexico16 and (2) many female nurses are also homemakers (a factor known to confer an increased risk in Mexico)17.
Due to the stated considerations, we call for continued surveillance and prevention of COVID-19 cases caused by known (and possibly future) SARS-CoV-2 variants and subvariants that are able to evade previous immunity.
The main strength of this study was its ability to provide an estimate of COVID-19 reinfection episodes in a highly vulnerable population group highly compliant with vaccination and closely followed during 2 years. However, we acknowledge limitations: (1) it is possible that results may not be generalizable to other populations (mainly because this hospital provides access to on-site, free and unlimited diagnostic testing for its employees, but also because of local/regional differences in transmission patterns that could have modified human behavior and vice versa); (2) there could be an underestimation of the true reinfection rate due to the voluntary nature of the on-site medical consultation program and the occurrence of asymptomatic infections that were not considered; (3) no distinction between vaccine types was made, although the BNT162b2 and ChAdOx1-S vaccines were used for the primary series and boosters, respectively, in the great majority of hospital workers (who were vaccinated in our hospital in accordance with the national vaccination program); (4) there is not enough information to determine whether booster doses provide protection against reinfection, but the cohort will continue to be followed; (5) sequencing of viral isolates was not performed systematically in reinfection cases, although we used an accepted definition to exclude cases of persistent infection; (6) adherence to non-pharmacological interventions was not assessed over time, although the mandate to use medical-grade masks inside the hospital was not modified during the study period; and (7) comorbidities and human behaviors were not measured and remain to be studied as factors potentially related to reinfections.
In conclusion, the rate of SARS-CoV-2 reinfection cases in hospital workers rose from 1.9 to 23.1 cases per 100,000 persons per day during the Omicron wave despite a high primary vaccination coverage rate. The extent to which booster doses may have affected this rate remains to be determined, but preliminary results indicate that almost one-third of reinfected workers had received a booster dose before their last COVID-19 episode. Although reinfection episodes were mild in this cohort, a call for continued prevention efforts is needed to lessen impacts at the individual and societal levels.











 text new page (beta)
text new page (beta)


