INTRODUCTION
The risks of residing or visiting sites at a high altitude above sea level (usually considered if >2,500 m) and derived hypoxemia were gradually discovered throughout history, although most of what is known about adaptation to altitude was discovered in the first half of the 20th century. The most relevant research focused on populations that live permanently at >3,500 m above sea level and on diseases due to exposure to high altitudes, generically called “mountain sickness,” with information obtained during ascents or in laboratory simulations with hypobaric oxygen chambers. In the great elevations, however, scarce and unique populations live permanently, concentrated primarily in the Andean and Himalayan zones. Most of the research at extreme altitudes was done because of the implications for mountaineering and to explore physiological adaptations to extreme conditions. Two of the most well-known projects were in fact called Operation Everest, although they studied volunteers from several altitudes. The study of these populations described the responses of humans to high altitude, although extreme, and allowed to compare them with those of other species. However, it is also important to learn about the behavior of populations that live at moderate altitudes (2,000-2,800 m), where a large number of people live in several countries in the world, especially in Latin America.
The objective of the present review is therefore, to describe responses found in populations that live at moderate altitudes, using mainly reported data from Mexico City and the Valley of Mexico (2,240 m above sea level), but also information from other Latin American cities. In the Valley of Mexico, research on altitude has been conducted since the colonial era and more formally in the 19th and early 20th centuries, mainly by Daniel Vergara Lope, prompted in part by observations and conclusions of Dennis Jourdanet1. Vergara Lope flatly rejected an expression of Jourdanet, which disdained the possible adaptation to hypoxemia of the population of the Valley of Mexico and considered it irreversibly affected by its consequences. In fact, exposure to moderate altitude with physical activity may have health benefits for some patients2. Relevant investigators in Latin America also studied in the mid-20th century the adaptation to altitudes3-5, centering mainly in populations residing at high altitude.
The focus of this review is primarily on aspects relevant to respiratory and cardiovascular responses, although other important aspects such as the impact on prenatal development, reproduction, sports training, and neuropsychological functions6 are not included here, as well as the basic mechanisms that trigger hypoxemia and its response, among others, all deserving detailed summaries. The effect on respiratory diseases is also not dealt with, although a recent review was published7 dealing mainly with the impact on asthma, COPD, pulmonary hypertension and sleep apnea. The Supplementary Annex contains a short list of general texts on high-altitude medicine and physiology, including the book edited by Hornbein and Schoene with more than 3,000 references.
Search procedure
To gather the information, we searched publications in PubMed with the following keywords: altitude, arterial blood gases, hypoxemia, combined with Mexico, City of Mexico, and moderate altitude. Furthermore, information was searched in Google's scholar, in web pages in Spanish, with the equivalent terms, to find articles primarily of Latin American origin published in local or regional journals that are not incorporated into PubMed. Research conducted at these elevations is scarce but indicates an impact of altitude on its inhabitants, and it is certainly partial on purpose, because it is based primarily on information published in Latin America.
IMPACT OF ALTITUDE
The atmosphere maintains an oxygen concentration close to 21% and does not vary with altitude throughout the whole inhabited and visited areas of the world. The main effect of altitude is the reduction of the barometric pressure (Pbar) and of the partial pressure of oxygen (PO2) of the air and therefore, of the concentration of oxygen molecules per liter of air (molar concentration of oxygen). For example, in relation to sea level, the Pbar in Mexico City (585 Torr or mmHg on average) is 77% that of sea level (760 Torr), and the PO2 of the inspired air (PIO2), the air, hot and humid in the trachea, is 113 Torr, 75% of 150Torr at sea level.
The limit for a permanent residence of humans is considered an altitude of 5-5.5 km, where the Pbar is reduced to about 50% of that at sea level (more precisely, at an altitude of 5.8 km, Pbar falls to half of the pressure at sea level). Above this altitude, there is only temporary human presence either for work – in general mostly during the day, and sleeping in lower places – or for mountaineering. The other absolute limit has been the ascent to Everest without oxygen, a feat that can be performed by very few humans, and on favorable days when the Pbar is higher than average.
WORLD POPULATION LIVING AT MODERATE ALTITUDES
The population that permanently lives in sites of moderate altitude is substantial in the world and in Latin America, especially in countries such as Peru and Bolivia8. It is estimated that around 140 million people live in the world at altitudes higher than 2,500 m above sea level9, including 25% of Peruvians, and 4.5% of Mexicans. In Mexico, 50% of the population lives at altitudes higher than 1,500 m10. The cities of Mexico, Puebla, and Tlaxcala, with altitudes of around 2,200 m, Zacatecas and Pachuca 2,400 m, and Toluca 2,650 m, are examples of cities at moderate altitude where large populations are concentrated11,12.
MECHANISMS OF PHYSIOLOGIC RESPONSES TO HYPOXEMIA
Briefly, the responses to hypoxemia are triggered by activation of the oxygen sensor, a protein encoded by the EGLN1 gene, which increases the hypoxia-inducible factors (HIF1A, HIF2A, and HIF3A). These transcription factors, when they accumulate, induce the transcription of hundreds of genes, which, in turn, trigger the various bodily responses to hypoxia: increase in gas exchange, erythropoiesis (through erythropoietin), neovascularization by angiogenic growth and tissue remodeling factors, activation of genes related to glucose metabolism, changes related to vasomotor and endothelial control, and alterations in the functioning of the carotid body. These responses have a time course that can take from minutes to generations. The fastest responses are called acclimatization, typically occurring when a native of sea level travels to higher altitudes, and are generally reversible on returning to sea level; examples are hyperventilation and increased hemoglobin (Hb) concentration. There are non-reversible changes of development in people who were born and live at altitude; and finally, there are changes that occur by natural selection in thousands to hundreds of thousands of years. Most responses to hypoxemia are triggered when SaO2 decreases to below 90%.
Genetic variants of the oxygen sensor have been demonstrated, the hypoxia-inducible factors and gene transcriptions being more frequent in the more ancient populations residing at altitude, the Tibetan and Peruvian, compared to those at sea level. The Tibetan pattern has sustained the hyperventilation of acclimatization permanently (without decreasing with age), but has blocked polycythemia, with opposite changes in the Peruvian population due to variants of the genes related to the oxygen sensor and the transcription factors. Evolutionary changes can be expected primarily in populations that have inhabited high areas for several tens of thousands of years, present, for example, in Asian populations of Tibet and Nepal.
On the other hand, in the Valley of Mexico, in Tlapacoya, human remains have been found with an estimated age of 12,000 years13, along with obsidian objects and animal bones dated between 22,000 and 25,000 years14. According to experts' opinions, these findings can suggest human presence for a long time before the dated ages15, not different from those found at altitude in the Himalayas16. It is important to note that the mechanisms of adaptation to altitude vary between Tibetans, Ethiopians and Peruvians17, the three being effective since they have populations that live permanently and reproduce at similar altitudes. However, the Tibetan form of adaptation appears to have advantages, because they have Hb concentrations similar to those at sea level and higher alveolar ventilations. Of great interest is the high frequency of the gene EPAS1 (which encodes HIF-2alpha) related to Hb, traditionally low in the population of the Himalayas and postulated to originate from the Denisovan hominid race18,19, which was increasing in the population presumably because of exposure to altitude. Previously, high frequencies of the EGLN1 and PPARA genes had been identified in a hypoxemic population, and which could provide adaptive benefits20.
ACCLIMATIZATION TO ALTITUDE
When a person travels to a place at a higher altitude than his or her residence, a process called acclimatization occurs beginning in the 1st days after arrival, with rapid responses such as hyperventilation. In fact, one of the most efficient compensations is the increase in the number and especially in the depth of breaths. Hyperventilation occurs gradually in hours but usually persists for decades in residents of a considerable altitude. The loss of hyperventilation at advanced ages has been described in some South American populations, manifested by an increase in the partial pressure of carbon dioxide in the arterial blood (PaCO2) in middle-aged adults4,5.
Another frequent compensation, which develops in weeks, is the increase in the production of red blood cells and in the concentration of Hb in the blood (polycythemia), triggered by the production of erythropoietin, resulting in an increase in the transport capacity of oxygen in the blood (Fig. 1, lower graph). This increase in Hb, unlike hyperventilation, affects PaO2 very little, but tends to improve the concentration of oxygen in venous blood. Therefore, an improvement in tissue oxygenation up to a certain point is expected, where an increase in blood viscosity slows microcirculation.
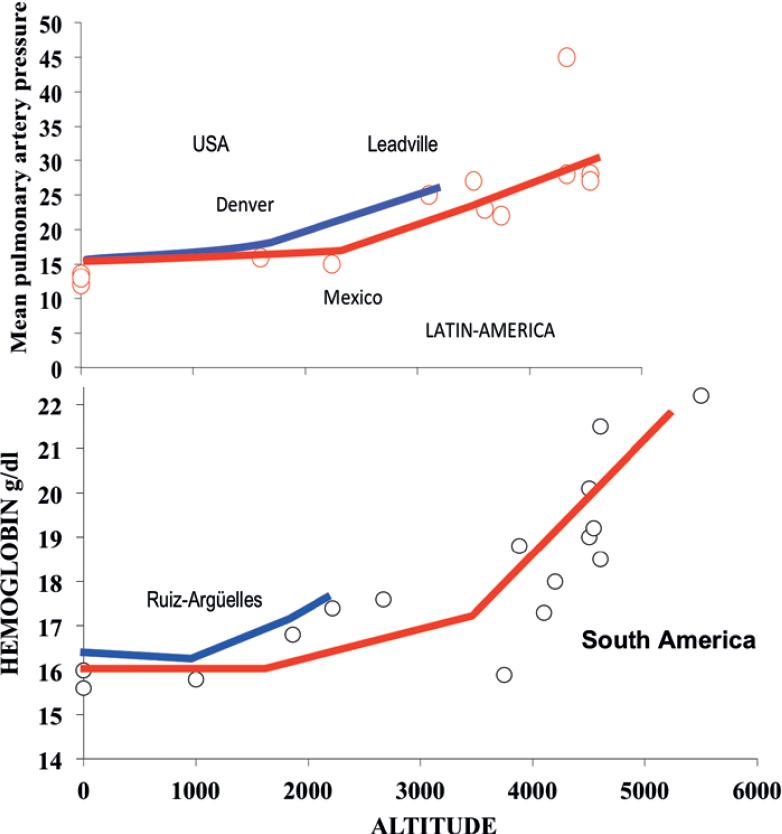
Figure 1 Lower graph: Reported hemoglobin according to altitude in several regions of South-America (mostly in Peru, from Hurtado et al.) and those from Ruiz-Arguelles et al. study from Mexico. Upper graph: Mean pulmonary artery pressure at rest measured at different altitudes in America including Denver and Leadville, Colorado. Rises more consistently above sea level values around 2000 m.
With time, profound tissue changes are generated, which involve vascularization (shorter distance from the tissue to the capillary, with improved diffusion), and adjustments in the enzymes related to the production of energy, with optimization of oxidative processes and energy production.
Alveolar hypoxia leads to pulmonary vasoconstriction, a very efficient mechanism to compensate local or regional lung diseases, shifting the flow to ventilated acini, as occurs in pneumonia, likely the commonest cause of hypoxemia. However, altitude hypoxia leads to diffuse vasoconstriction and increase in pulmonary resistance that may generate pulmonary artery hypertension during exercise or even at rest (Fig. 1, upper graph). The degree of hypoxic vasoconstriction is considered heterogeneous in the population, and these variations may explain an improved or worsened tolerance to altitude in short-term or long-term exposures, and in general, to illnesses associated with high altitude. Pulmonary artery pressure in normal subjects varies among individuals, and according to genetic ancestry. Pulmonary hypertension is expected to be more common among Aymara than among Tibetans at the same altitude, and was reported as normal in Mexico City among healthy subjects21.
ADAPTIVE CHARACTERISTICS IN THE RESIDENT POPULATION OF THE VALLEY OF MEXICO
Table 1 lists several characteristics found in the resident population at moderate altitudes, such as the Valley of Mexico, which are generally known manifestations of altitude adaptation.
Table 1 Adaptive changes to altitude and hypoxemia in population of the Valley of Mexico
| Mechanism | Data | Reference |
|---|---|---|
| Chronic hyperventilation | Mexico PaCO2 31 Torr (mmHg) | 22 |
| Bogotá 33 Torr | ||
| Polycythemia | Hemoglobin about 10% higher than at sea level | 36 |
| Exercise capacity, maximal O2 consumption | Reduced in sea-level athletes competing in Mexico | 45 |
| Ventilatory responses to hypoxemia and CO2 | Often flat to hypoxemia (precise percentage unknown) and normal response (slope) to CO2 | 35 |
| Pulmonary artery pressure | Normal in healthy subjects | 21 |
| Spirometric values | Higher than Mexican-Americans at sea level if adjusted by height, age and gender. Could be an effect of stunting as occurs in underserved areas. | 41 |
| DLCO | Higher than at sea level even after adjustment for altitude and hemoglobin | 43 |
| Maximal voluntary ventilation and Peak expiratory flow rate | Higher than at sea level due to lower air density | 42 |
*We lack information about muscle adaptations as well as vascularization, or glycolysis enzymes or genetic variants linked to Amerindian ancestry, or frequency of genes associated with adaptation to altitude in Tibetan or Peruvian populations.
Oxygenation level
Table 2 compares the typical arterial blood gases' values at sea level, and those found in Mexico City as a result of a compilation of PaCO2 values (which show an average of 31 Torr in arterial blood) and PaO2 (on average 65, although it decreases with age) reported in healthy subjects22, with a mean SaO2 between 92% and 94%. On the other hand, a mean pH of 7.4 (with its range of values) and the appropriate base excess for the pH of 7.4 (the normal value for Mexico City is a mean of –5 mEq/L), have been traditionally considered normal. PaO2 values fall with age (between 0.25 and 0.3 Torr or mmHg per year) and with increasing weight, among other factors23. PaCO2 remains more constant throughout life, although an increase in PaCO2 with age, especially in postmenopausal women, has been described24.
Table 2 Normal values at sea level and at 2,240 m above sea level (Mexico City)
| Variable | Sea level | 2,240 m (Mexico City) |
|---|---|---|
| Mean Pbar (Torr) | 760 | 585 |
| PaO2 (Torr)* | 80 - 100 | 65 - 70 |
| PaCO2 (Torr) | 40 ± 2 | 31 ± 2 |
| pH | 7.35 - 7.45 | 7.35 - 7.45 |
| HCO3- (mEq/L) | 24 ± 3 | 19 ± 3 |
| Base Excess (mEq/L) | 0 | – 5 |
| SaO2 (%) | 97% | 92 - 94% |
| Hemoglobin (g/dL, men and women) | 16 ± 2, 14 ± 2 | 17.4 ± 0.9, 14.6 ± 1 |
| Hematocrit (%) | 47 ± 5, 42 ± 5 | 51.6 ± 2.6, 44.6 ± 2.7 |
| P(A-a)O2 (Torr) | <15 (about age/3) | <15 (age/3) |
| Mean Pap (Torr) | <16 | <16 |
*PaO2 declines with age (approximately 0.3 Torr or mmHg per year) and in decubitus; see text. For hemoglobin and hematocrit is mean and standard deviation. Shunt in both altitudes is < 5% of the cardiac output in healthy subjects. Chlorine should increase in the same proportion as bicarbonate decreases to maintain ionic equilibrium.
Pbar: mean barometric pressure; PaO2: partial pressure of O2 in the arterial blood; SaO2: oxygen saturation of hemoglobin in the arterial blood; P(A-a)O2: alveolo-arterial difference in PO2; Pap: pulmonary artery pressure.
In Mexico, a compilation of published studies has been frequently used as a reference, which in general has been adequate and concludes at an average PaCO2 of 31 Torr22. This PaCO2 level implies that the residents of Mexico ventilate (alveolar ventilation) 29% more than people living at sea level, which although substantially improves oxygenation, it increases the basal respiratory work and work at any exercise level. Hyperventilation facilitates the generation of dyspnea, a complex feeling that occurs consistently when minute ventilation or respiratory work is close to the individual's maximum, especially relevant for respiratory patients.
On the adverse side, there is also a greater exposure to pollutants (at the same atmospheric concentration; see section on environmental pollution) and, in principle, a greater caloric and water loss. Chronic hypocapnia is accompanied by a loss of bicarbonate and base excess, and most probably an increase in chlorine (Cl-) for ionic balance (Table 2).
The SaO2 at rest in Mexico City, although above 90% (in healthy and young individuals), the limit below which many of the responses to hypoxemia are triggered, is near the knee of the Hb dissociation curve with oxygen, in a region where mild falls in PaO2, such as those that can occur during sleep25, or in decubitus, especially in obese people and with aging, cause a greater decrease in saturation. In the metropolitan area of Mexico City, 6% of the population ≥40 years of age has an SaO2 of ≤88%, which, if chronic, meets the current criteria for recommending home oxygen therapy23. That is, a reasonable compensation for hypoxemia can be achieved only if the entire gas exchange system works properly but there is a limited reserve.
Even with these usual levels of oxygenation, SaO2 between 92-94% (vs. 97% at sea level), responses to hypoxemia in healthy and young people are observed in Mexico City (Tables 1 and 2), which proves the need for improved indicators of hypoxemia than a point measure of arterial blood gases or pulse oximetry, measured awake and resting. Within these measures, the continuous estimation of SaO2 could be considered for prolonged periods, at least 24 h, which allow identifying hypoxemia during sleep or exercise, undetectable for typical measurements at rest. Of more relevance would be the measurement of tissue oxygenation, general or regional, but at this moment, there are no instruments that allow to perform it in the clinical setting in a routine and non-invasive way.
With altitude, red cell 2,3 diphosphoglycerate tends to increase leading to a rightward shift of the standard oxyhemoglobin dissociation curve and PO2 at 50% saturation (p50). However, the presence of respiratory alkalosis during acclimatization to simulated altitude tends to compensate the in vivo p50.
ESTIMATION OF GASOMETRIC VALUES AT DIFFERENT ALTITUDES IN MEXICO
Because it is unlikely that reference values will be generated for many altitudes in Mexico, Latin America or other countries with settlements at various altitudes, it is important to have estimates of the expected values10. Although these estimates cannot substitute for actual measurements, they can be of great help for the proper interpretation of gasometry data, instruments that are accessible in many places. These estimates based on the alveolar gas equation (Supplementary material) are available for different altitudes and populations in Mexico, and a proper estimate depends to a large extent on having an estimated PaCO2 close to the real one for altitude, based preferably on interpolation of empirical data. Other moderate-altitude reports on arterial blood gases can be found in additional publications24,26-28.
Oxygenation during sleep
Healthy, young subjects residing in Mexico City frequently have an SaO2 <90% at night25. It is known that the sleep of visitors at high altitudes, generally above 2500 m, is interrupted in coincidence with periodic breathing, which generates wide oscillations in oxygenation. Like other alterations frequently observed at high altitudes, it could occur29, but less frequently, at moderate altitudes in visitors who arrive from sea level. In the residents of the Valley of Mexico, periodic breathing is not a characteristic of their breathing during sleep, but the frequency among visiting lowlanders is unknown. On the other hand, respiratory patients30,31 and obese individuals32 suffer from severe hypoxemia during sleep much more frequently than at sea level, at the same degree of lung damage, which presumably worsens their prognosis unless domiciliary oxygen therapy is prescribed. In the PLATINO population study, 6% of the 40+ year-old population in the metropolitan area of Mexico City had an SaO2 ≤88%, level at which oxygen should be prescribed to prevent deterioration in health and an increase in mortality, especially if additional indicators of hypoxemia are present: polycythemia, pulmonary hypertension, or hypertrophy or dilatation of the right heart. Acetazolamide may reduce altitude periodic breathing in newcomers to moderate altitude, as well as supplementary oxygen, acting as stabilizers of the breathing rhythm.
RESPONSE OF THE CHEMORECEPTORS TO HYPOXIA AND HYPERCAPNIA
The ventilatory response to hypoxemia and hypercapnia has been evaluated in residents of Mexico City33-35. The slope of the response to CO2 does not differ from that found at sea level, but the intercept is modified by the baseline level of PaCO2, which is lower in Mexico City than at sea level33, with a higher respiratory drive than at sea level34. That is, the change in ventilation per change in PaCO2 is similar in the Valley of Mexico to that at sea level (same slope of the response curve). On the other hand, in a minority of healthy individuals, the response found to hypoxemia was flat35. This has been previously reported in Andean areas, and its consequence is uncertain since, although it would be expected that respiratory work and periodic breathing during sleep would decrease, it could cause greater hypoxemia in the face of a lung disease or due to an ascent to higher altitudes. It would be necessary to determine how widespread this response is in the healthy population that resides at moderate altitude, and if it occurs since childhood or develops with age, or whether it is associated with the Amerindian genetic contribution.
HEMATOPOYESIS
Ruiz-Arguelles et al. studied the hematological indices at the level of the cities of Puebla and Toluca, finding a clear increase in Hb at the altitude of Puebla (same as that of the Valley of Mexico) and even more so in Toluca, with a borderline change at lower altitude (Fig. 1, Lower graph)36. Hb increases 5.5% in lowlanders acclimatized to 2,100 m and stabilizes after 7 months37,38. It is important to note that within Mexico City, there is a variation of altitudes due to land unevenness, with areas of a considerably higher altitude. For example, the main exit roads of Mexico City rise up to 3,100 m, similar to the altitudes of Toluca (the Marquesa), Cuernavaca (Tres Marías) and Puebla (Río Frío), with settlements on these sites, as well as in the area of the Ajusco mountain (up to 3,930 m). Therefore, individuals with higher than usual degrees of polycythemia can be seen in the city, although these values could be appropriate for the person's place of residence, an information which should always be considered for an adequate understanding of the oxygenation level of an individual. Erythropoietin increases rapidly after exposure to moderate altitudes39, although differences have not been reported among blood donors compared to published studies at sea level40.
LUNG FUNCTION AT MODERATE ALTITUDES
Lung function and, therefore, respiratory function tests can be affected at altitude by several mechanisms. On the one hand, the ethnic composition of the population tends to change with the altitude, having in general populations with a greater indigenous component living at higher altitudes, as is the case in Peru and Mexico, among other countries. Ethnic composition can have important implications for health and disease susceptibility. Frequently, the populations at higher altitudes also have lower socioeconomic levels and greater degree of marginality, which considerably affects the health, anthropometric measures, and the respiratory function itself. Malnutrition and marginal conditions tend to reduce height and the proportion between the body's upper or thoracic segment and the lower or pelvic segment, so that at the same height, the proportion of chest and lungs is higher than usual. Since the prediction equations for spirometry and other tests of respiratory mechanics include height as a predictor, it has been shown that children and adults of the Valley of Mexico have consistently higher altitude-adjusted values than populations of European or Mexican-American ancestry at sea level, and considerably higher than those of African origin41.
There are respiratory tests based on maximum expiratory or inspiratory flows that involve turbulent flow, dependent on the air density, such as the peak expiratory flow rate (PEFR) and maximum voluntary ventilation (MVV). With altitude, the air density decreases and higher maximum flows can be generated, which has been demonstrated for the PEFR41 and for the MVV42. Finally, exposure to chronic hypoxemia, from the prenatal stage and during growth and development, can affect the size of the chest and lungs, which has been shown at high altitudes, but not reliably at moderate altitudes.
The single-breath diffusing capacity of the lungs for carbon monoxide (DLCO), a gas exchange standard test, increases consistently with altitude due to both the lower partial PaO2, and the tendency of Hb to increase with altitude36. However, in spite of making the usual altitude and Hb adjustments recommended, the DLCO tends to be higher in Mexico City and Bogotá than that found at sea level43, which indicates a larger alveolo-capillary surface area for gas exchange, either by recruitment of alveolar capillary units even at rest, or by an effect on lung development.
GAS EXCHANGE AT MODERATE ALTITUDES
The behavior of gas exchange at moderate altitudes was recently analyzed by computational models of the lung44. These models allow us to estimate pulmonary performance under different controlled circumstances, a very useful situation from an educational and theoretical point of view but requiring empirical verification of the findings, which in real life are more complex since several changes occur simultaneously, and adjustments are not considered in the models. The patterns of response to changes in cardiac output, minute ventilation, base excess, shunt, ventilation/perfusion (V'/Q') heterogeneity, inspired fraction of oxygen, Hb, or p50, estimated for Mexico City are generally parallel to those estimated for sea level displaced to the lower levels of PO2 and PCO2.
EXERCISE CAPACITY
A reduction in the maximum capacity to exercise and maximum oxygen consumption is expected in Mexico City at least during acute exposure or after a short acclimatization45, a phenomenon observed in athletes since the Olympic Games in Mexico in 1968, where the distance runners increased their time by 5-10% in relation to times achieved at sea level (Fig. 2). There was also an increase in the times of the winners of long-distance tests, compared with those of the previous and subsequent Olympic games. The best marathon times in Mexico City are slower than those at sea level (in 2017, in men, Fikadu Kebede, 2:17:27; in women, Gladys Tejeda, 2:36:15), while the best world records, in places at low altitude, are for men (Dennis Kiputo), 2:02:57 and for women (Paula Radcliffe), 2:15:25, and with a permanent tendency to drop. On the other hand, due to the lower air density, in Mexico City, speed increases during short tests, especially in cycling, so the velodrome in Mexico City was frequently used for attempting to break a velocity record.
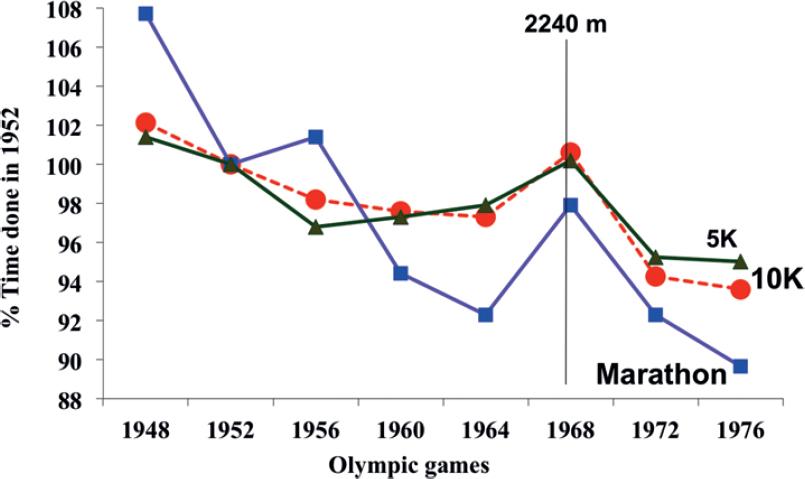
Figure 2 Olympic marks in long-distance running competition from 1948 to 1976. A continuous reduction in times is observed (expressed as percentage of 1952 Olympic Games), except for the Mexico City Olympics in 1968.
Interpolating data derived from experiments at simulated progressive altitudes that reached up to the altitude of Everest (Everest operations), the expected drop in maximum oxygen consumption at 2,240 m altitude is 9%, an amount difficult to demonstrate among inhabitants of the Valley of Mexico unless compared against themselves in experiments in compression chambers or with mixtures simulating sea level. Some studies have evaluated an exercise response in Mexico City46 and at other moderate altitudes47.
Not surprisingly, desaturation at high levels of exercise is frequent due to diffusion limitation, which at sea level has been reported only at maximum exercise in high-performance athletes. The altitude of residence has to be considered in the interpretation of desaturation in exercise, usually considered an indicator of interstitial lung disease, pulmonary vascular disease, or emphysema. However, at altitude, desaturation can be seen in healthy people if a high level of oxygen consumption is reached47. It is important to consider that desaturation in exercise can also be due to alveolar hypoventilation, especially in people with very abnormal pulmonary mechanics, or with muscle weakness, a situation that is not identified with the pulse oximeter but is perfectly clear with an arterial blood gas analysis showing increasing PaCO2 during exercise.
ALTITUDE AND IMPACT OF ENVIRONMENTAL POLLUTION
Pollutant concentrations in communities at moderate or high altitude vary; however, biomass smoke in rural areas may be a relevant outdoor pollutant in addition to being an ancient indoor pollutant in developing countries. Geographical location also may reduce pollutant dispersion, as occurs in the valleys of Mexico, Toluca, and Puebla, surrounded by high mountains. Chronic hyperventilation derived from residing at altitude implies greater exposure to air pollutants. The dose of pollutants, that is, the amount reaching the respiratory system (not necessarily the particles or toxins that pass into the blood or adhere to the mucous membranes), increases proportionally to hyperventilation. That is why an adjustment has been proposed to the permitted levels of pollutants recommended at sea level for places such as Mexico City48. The increase in ventilation does not have a linear relationship with Pbar, and it varies with ethnicity. At high altitudes, the Tibetan population maintains greater ventilation than the South-American Aymara, which has been considered an adaptation (not only acclimatization) more beneficial than that achieved in South America. At altitude, the reduction in the molar concentration of oxygen makes combustion more difficult, and it is easier for it to occur incompletely, generating more pollutants and carbon monoxide.
RELEVANT FUTURE RESEARCH ISSUES
There are a variety of research topics within the respiratory and cardiovascular areas that require attention and of which a tentative summary is made below. It is important to elaborate on the ventilatory response to hypoxemia throughout growth, development and aging, and the Amerindian contribution to the response. Healthy adults residing in Mexico City often lack a significant response to hypoxemia, and it would be advisable to clarify whether it is a characteristic of the place of birth or is related to genetics, or whether tolerance develops over time. It would be recommended to determine arterial blood gases or non-invasive measurements (pulse oximetry, expired capnography, PaO2 and transcutaneous or expired PaCO2) in subjects at different altitudes, preferably performing ventilatory responses to hypercapnia and hypoxemia, and measurement of Hb and the Amerindian genetic contribution.
Another matter of interest would be to advance the understanding of the impact of altitude on mortality due to various diseases, and oxygen therapy requirements in Mexico. An additional relevant point is whether having lived for thousands of years at moderate altitudes, such as in the Valley of Mexico, confers a population further protection to hypoxemia, which would make it advisable to adjust the criteria for chronic oxygen therapy. The usual criterion to prescribe oxygen is the arterial blood gases in stable patients (PaO2 <55 Torr, or <60Torr with cor pulmonale, polycythemia or pulmonary hypertension) and the question is whether these cut-off values, obtained at sea level and very consistent across a number of studies, apply to the population living at moderate altitude.
Elucidating the impact of altitude-induced hyperventilation on the damage conferred by highly concentrated pollutants in the large cities of several Latin American countries and where appropriate, the need to adjust permissible standards of contaminants for altitude, is of great relevance for the best protection of the health of the inhabitants.
CONCLUSIONS
The residents of Mexico City ventilate approximately a quarter more and have a concentration of Hb 10% higher than residents of sea level. These compensations reduce the impact of altitude hypoxemia, but do not eliminate it. Among healthy young people in Mexico, the level of oxygenation in the blood is between 92% and 94% (compared to 97% at sea level) (Figure 3), and in Mexico, it is more frequent to fall to <90% while sleeping.
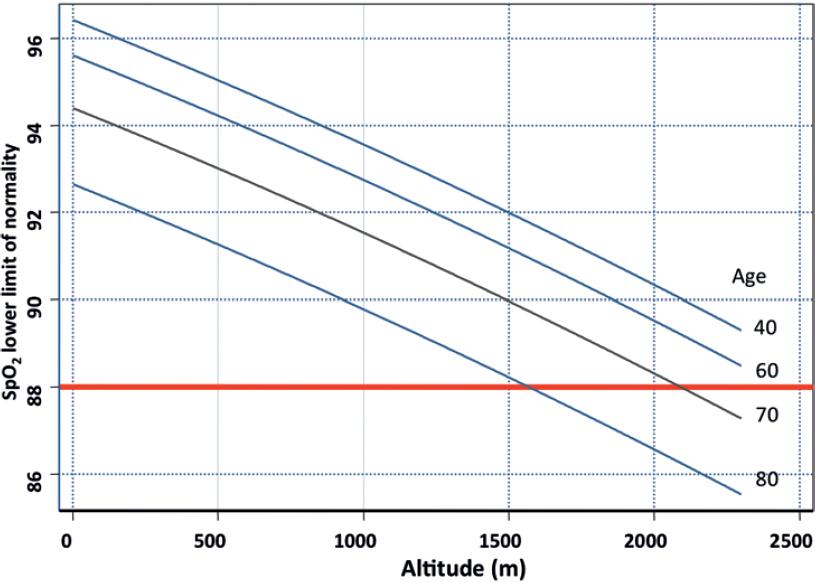
Figure 3 Lower limits of normality (5th percentile according to altitude and age, from a population-based survey in 5 cities of Latin America (PLATINO STUDY).
It is thus clear that the healthy residents of Mexico City manifest physiological responses to the lack of oxygen whose impact is little known. It is possible that pulmonary growth is stimulated during childhood, or that over many generations of residence at altitude the transport mechanisms and use of oxygen in tissues improve, although we do not know for sure. Residing at moderate altitudes provides a better tolerance to hypoxemia, at least in some circumstances49. For example, the inhabitants of Mexico City are more likely to reach the top of the Popocatepetl volcano (5,426 m) than those who attempt to reach it from sea level, protecting from the mountain sickness developed in other residents at a moderate altitude50.
On the other hand, patients with respiratory diseases living in Mexico City are more susceptible to severe deoxygenation, which worsens their condition rapidly and makes them require supplemental oxygen or move to sea level, and increases their exposure to air pollutants.
From the biological point of view, humans lack the best adaptations to live at high altitudes described in vertebrates because they evolved at low altitudes. The feat of climbing Mount Everest (8,890 m) without oxygen is achievable for very few elite athletes and always on the verge of damage and death. Staying at these extreme altitudes is possible only for very short periods of time and, in fact, a permanent residence at altitudes greater than 5,500 m is harmful. Furthermore, among the natives of altitudes higher than 3,000 m, after years, a group develops in the absence of lung disease the so-called chronic mountain sickness or Monge's disease, characterized by cardio-respiratory failure and polycythemia and shortened life, which can be cured by traveling down to the coast or by using oxygen. For now, clearly the altitude of Mexico City results in a greater need for oxygen therapy at home, and makes us inhale deeper the city's air.











 text new page (beta)
text new page (beta)


