INTRODUCTION
Mantle cell lymphoma (MCL) is a rare and aggressive disease which accounts for approximately 5% of all B-cell non-Hodgkinӳ lymphomas (NHL)1. The incidence of MCL is higher in non-Hispanic Whites in the United States2,3. There is very limited information about this variant of NHL in México4. We have previously shown that several B-cell malignancies such as chronic lymphocytic leukemia (CLL), multiple myeloma, Waldenstromӳ macroglobulinemia, and others are substantially less frequent and less aggressive among Mexican patients than in Caucasian populations4,5. Here, we report a retrospective analysis of a group of 12 patients with MCL.
MATERIALS AND METHODS
Patients
The files of all the patients identified with the diagnosis of MCL after January 2003 were analyzed. Clinical evaluation of MCL patients included history and physical examination, assessment of performance status, comorbidities, B symptoms, features of the treatment, response to treatment, evolution, and current status.
Approval
Clca Ruiz Institutional Review Board approved this study and every participant signed and provided a consent document before the study.
Laboratory workup
It included a complete blood cell count with differential count, comprehensive metabolic panel, lactate dehydrogenase, beta-2 microglobulin levels, hepatitis panel, HIV status, and serum immunoglobulin levels. Immunophenotype on peripheral blood looking for the typical MCL phenotype (CD5, CD20, CD19, sIgM/sIgD, FMC-7 + B cells with monoclonal kappa/lambda light chains, and dim/negative CD23, dim/negative CD200, and strong cyclin D1) was done.
Histological studies
Involved tissue and bone marrow aspiration/biopsy were performed at the time of the initial diagnosis. Immunohistochemical analysis of involved nodal/extranodal tissues looking for a strong nuclear staining for cyclin D1 (BCL-1 or PRAD-1) expression on MCL cells and SOX-11 expression was done.
Imaging studies
Imaging studies were obtained for staging purposes: whole-body positron emission tomographyףomputed tomography (CT) scan or computerized tomography (CT).
Statistical analysis
The primary outcome measure was overall survival (OS), defined as the time elapsed between the diagnosis of MCL and death from any cause, with censoring of patients who were alive on the last follow-up date. Secondary outcome measure was complete remission (CR), defined as the absence of adenomegaly, splenomegaly, and monoclonal B cell in the peripheral blood. Differences were assessed with Fisherӳ exact test. OS was estimated by the Kaplaneier method and differences between groups with compared with the log-rank test6. Two-sided p < 0.05 was considered as statistically significant. All statistical analyses were carried out in Stata 14 (StataCorp, College Station, TX).
RESULTS
Patients
Nine males and three females were included; median age was 56 years (range 40-87). Eight patients had a high MCL international prognostic index (MIPI) score, one was intermediate, and three were low. Five patients had circulating malignant monoclonal cells (Table 1).
Table 1 Salient features of the 12 patients with MCL
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 60 | 56 | 56 | 87 | 49 | 46 | 67 | 48 | 49 | 49 | 51 | 61 |
| Sex | F | M | M | F | M | M | F | M | M | M | M | M |
| Site | Nodal | Spleen | Bone Marrow | Nodal | Nodal | Bone marrow | Bone marrow | Bone marrow | Nodal | Bone marrow | Bone marrow | Nodal |
| Leukemia | No | Yes | No | No | No | No | Yes | No | Yes | Yes | No | No |
| MIPI | High | High | Intermediate | High | High | Low | High | Low | Low | Low | Low | High |
| R-CHOP | No | No | Yes | No | Yes | No | No | No | No | Yes | Yes | Yes |
| CHOP | Yes | No | No | No | No | No | No | No | Yes | No | No | No |
| Others | Bleo | No | Bort | PDN | Thal | Thal, bort, dexa | R, benda | Hyper-CVAD, R, MTX, Ara-C | No | No | No | No |
| Splenectomy | No | Yes | No | No | No | Yes | No | No | Yes | Yes | No | No |
| HSCT | Auto | Allo | No | No | No | Auto | Allo | ּ/ | Allo | - | ||
| Remission | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Survival time (months) | 12.7 | 13.5 | 0.05 | 0.24 | 1.9 | 5.7 | 4 | 1 | 2.5 | 11.8 | 6.4 | 3.8 |
| Status | Alive | Alive | Alive | Dead | Alive | Alive | Aliver | Alive | Dead | Alive | Dead | Dead |
F: female; M: male; MIPI: mantle cell lymphoma international prognostic index; R-CHOP: rituximab, cyclophosphamide, adriamycin, vincristine, and prednisone; Bort: bortezomib; Thal: thalidomide; Dexa: dexamethasone; Benda: bendamustine, MTX: methotrexate, Ara-C: cytarabine; HSCT: hematopoietic stem cell transplantation; Auto: autologous; Allo: allogeneic, Time: months after the diagnosis of the lymphoma. MCL: mantle cell lymphoma.
Treatment patterns
Five patients were treated initially with rituximab, cyclophosphamide, daunorubicin, vincristine, and prednisone (R-CHOP) and two with CHOP; three were given subsequently bortezomib with or without thalidomide or lenalidomide; and one patient was given bendamustine. In four patients, splenectomy was performed: the removed spleens weighed 1.4, 1.8, 2.8, and 4 kg. Five patients were given hematopoietic stem cell transplantation (HSCT): three allogeneic and two autologous (Table 1). No patients were treated with ibrutinib, acalabrutinib, obinutuzumab, temsirolimus, idelalisib nor venetoclax.
Survival
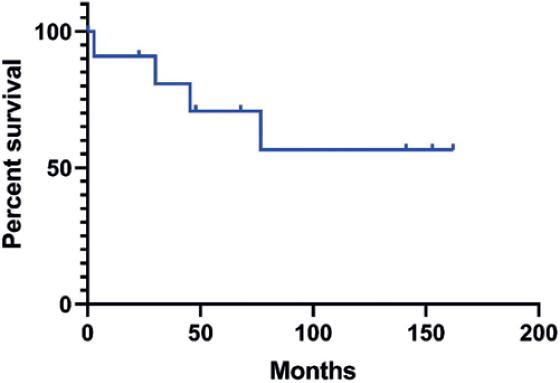
Patients have been followed for a median of 44 mos (range 0.6-162). Median OS for all the patients has not been reached and exceeds 162 months, whereas the OS at 162 months is 56% (Fig. 1). The 5-year OS for patients with high or low MIPI scores was 60 and 83%, respectively (p = 0.91), whereas the 5-year OS of patients given or not HSCT was 51 versus 83% (p = 0.69, Fig. 2). The median OS for patients having their spleen removed was better than that of non-splenectomized patients (>162 vs. 77 months, p = 0.55, Fig. 3), whereas the median OS of patients with or without a leukemic pattern of the disease was > 162 months versus 77 months (p = 0.35). Achieving a CR after the initial treatment was a significant prognostic factor: patients who achieved it had a median OS exceeding 141 months, whereas those who did not achieve it had a median OS of 16 months (p = 0.0006).
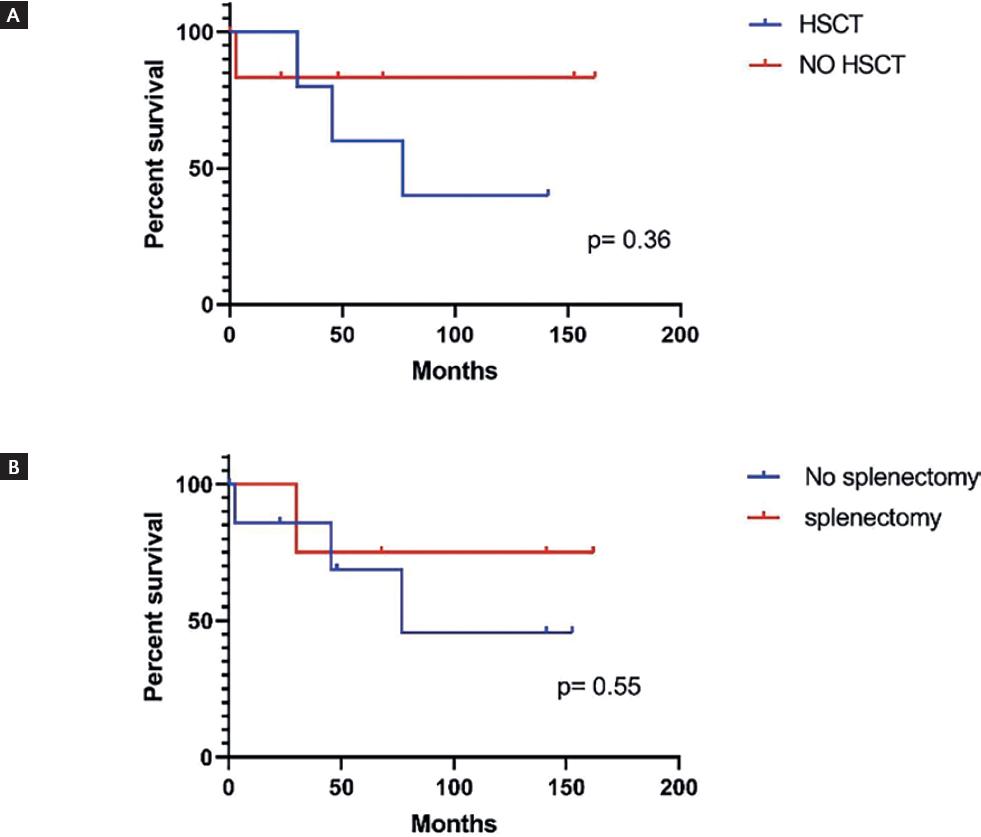
Figure 2 A) Overall survival of the 12 patients with mantle cell lymphoma, given or not hematopoietic stem cell transplants. Differences are not statistically significant (p = 0.36). B) Overall survival of the 12 patients with mantle cell lymphoma, having the spleen removed or not. Differences are not statistically significant (p = 0.36).
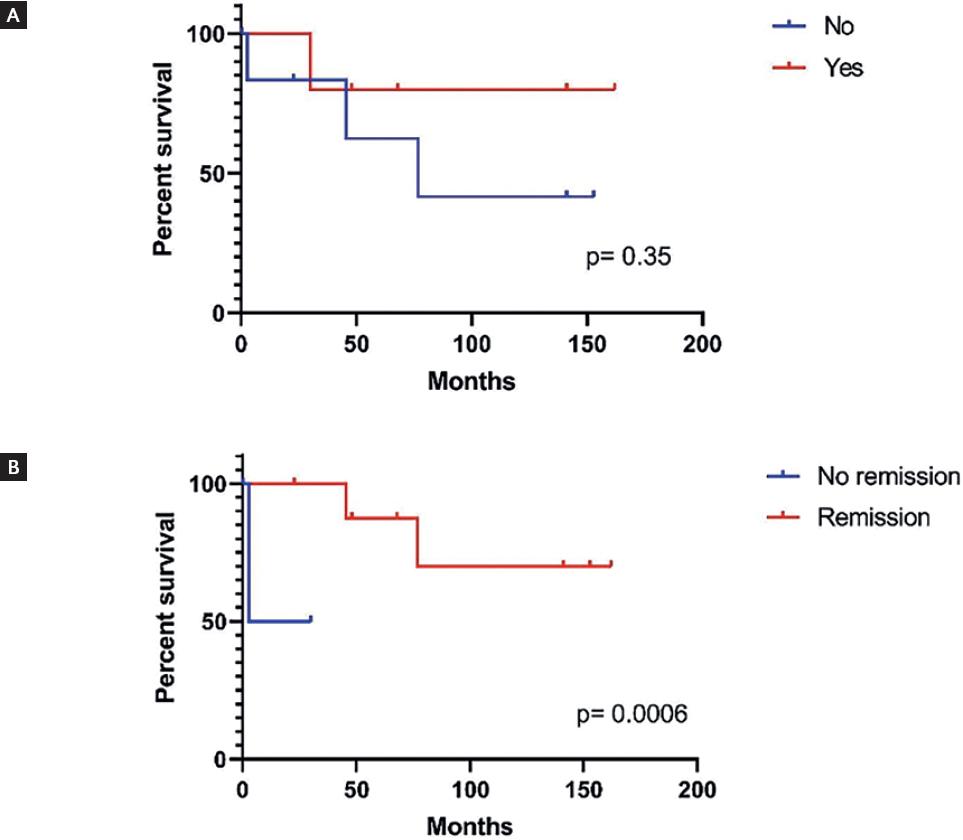
Figure 3 A) Overall survival of the 12 patients with mantle cell lymphoma, having or not malignant monoclonal cell in the peripheral blood. Differences are not statistically significant (p = 0.35). B) Overall survival of the 12 patients with mantle cell lymphoma who achieved or not a complete remission. Differences are statistically significant (p = 0.0006).
DISCUSSION
Jean Bernard, an icon in the world's hematology, presented in 1963 the concept of ԧeographic hematology" distinguishing two major branches; the so-called ethnic hematology that dealt with differences between populations and a second branch about environmental factors such as food habits, infections, and its implication with the hematological diseases referred as environmental hematology4,7. Along this line, we have analyzed the salient features of several hematological diseases, making comparisons with the features of some conditions in other populations4: we have shown that two B-cell malignancies, both CLL and multiple myeloma, are less frequent and less aggressive in México than in Caucasian populations4,8,9.
Different from other chronic mature B-cell malignancies, MCL seems to be in Mexican Mestizos as frequent as in Caucasians: Carballo-Zárate et al.5 have shown that MCL represents in México 6.7% of all B cell NHL, a figure similar to that informed from the United States, which is around 5%1,2. As far as the prognosis is concerned, we found that outcomes are substantially better than those informed in the literature both in Caucasian individuals3 and Taiwanese patients10, and could suggest that MCL has a more benign course in Mexican mestizos. Almost half of patients with MCL presented with leukocytosis, and a third, with splenomegaly; these cases resembled CLL but the immunophenotype of the clonal circulating malignant cells disclosed the true nature of the malignant B-cell proliferation; patients with a leukemic form of the disease had a worse prognosis. In four cases, the spleen was removed and it is interesting to point that the OS of splenectomized patients was better than that of the non-splenectomized patients, thus supporting a role of splenectomy in the treatment of MCL, as it had been previously recommended11, a procedure not even considered in the current therapeutic recommendations3. It is also noteworthy that achieving a CR was a significant prognostic factor since patients who achieved it had a median OS exceeding 141 months, whereas those who did not were significantly lower. The OS of patients who were grafted was worse than that of those who did not receive a transplant; this may reflect the fact that grafted patients had more aggressive forms of the disease (Fig. 2).
This study has several drawbacks: it is retrospective, includes a small number of patients and the treatment of the patients was non-randomly assigned. This small analysis of data on MCL treated at a single institution in Mexico, suggests that some of MCL patients in Mexico have an indolent clinical course with median survivals that exceed 10 years, particularly in patients who achieve a CR to initial treatment and who undergo splenectomy as part of their treatment program. Additional studies are needed to either ratify or rectify these observations.











 text new page (beta)
text new page (beta)