Introduction
Currently, chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death across the globe, while the World Health Organization (WHO) predicts that COPD will become the third leading cause of death by 2030.1 Similarly as other chronic conditions, COPD negatively affects quality of life and the disease burden is further increased by multiple comorbidities, including cardiovascular disease and cerebrovascular disease. Additionally, patients with COPD are two to three times more likely to have problems of mental health that the general population.2 Patients with comorbid physical and mental ill health are less likely to be identified, diagnosed, and treated.3
Among patients with COPD, various psychological aspects of functioning have been investigated but so far with little consequence for clinical practice.4 In the most recent Clinical Practice Guidelines, anxiety and depression are included as frequent comorbidities in COPD and are associated with poor health status and prognosis. Importantly, comorbidities with symptoms also associated with COPD may be overlooked e.g., heart failure and lung cancer (breathlessness) or depression (fatigue and reduced physical activity).5
The objective of the present review was to integrate the psychological factors associated with COPD and analyze the effective treatment alternatives available. A search was conducted in January and February 2021 with no language restrictions under the following criteria: [COPD OR chronic obstructive pulmonary disease] [COPD-mental health], [psychopathology-COPD], [depression-depressive disorder COPD], and [anxiety- anxiety disorders COPD] to identify manuscripts related to the objective. Inclusion criteria were the diagnosis of COPD and at least one psychological factor with a clearly indicated assessment. We searched for other potentially relevant studies by screening the reference lists and citations of included studies. Finally, all authors reviewed, analyzed using the GRADE system, and discussed the articles to provide recommendations. We present the following article in accordance with the narrative review reporting checklist.6
Anxiety
The morbidity rate of anxiety in non-hospitalized settings of COPD patients has varied from 13 to 46%, and in hospitalized settings from 10 to 55%.7
The coexistence of anxiety disorders and COPD has been shown in a worsening of symptoms, especially the shortness of breath or cough, but also leads to a higher rate of hospital care and increased doses of drugs such as bronchodilators, inhaled corticosteroids, and antibiotics. As an additional result, it causes a higher incidence and severity of adverse effects, accompanied by a worse overall prognosis.8,9
According to the retrospective analysis of a randomized controlled trial found that more than half of trial participants (of a total 1200 responses) reported mood disturbance during the study, participants reported symptoms of anxiety and low mood at least once during the previous 12 months.10
The available evidence suggests that less than one-third of COPD patients with anxiety are receiving appropriate treatment. Untreated comorbid anxiety and depression in patients with COPD have devastating consequences, as they tend to overwhelm the coping strategies of COPD patients and their caregivers, and may increase healthcare utilisation.11
Depression
In a prospective longitudinal study of 355 patients with COPD it was found that depression was a predictor of emergency care in COPD, independent of severity of disease or physical comorbidity. Even mild symptoms of depression increase the risk of care by more than twofold, and moderate to severe symptoms of depression increase the risk by nearly five times (Table 1).12
Table 1: Summary of publications regarding the association between psychological factors and pulmonary obstructive chronic disease.
| Outcome measures/Reference | Odds ratio - risk ratio - adjusted odds ratio - hazard ratio | Other factors found |
|---|---|---|
| Depression and emergency hospital
admissions(12) Depression and attendances at emergency departments |
OR = 2.63; 95% CI (1.48-4.66) OR = 2.78; 95% CI (1.55-4.99) |
Even mild symptoms and moderate to severe symptoms of depression increase the risk of use of urgent care, these findings are independent of severity of disease and comorbidity of other chronic physical conditions |
| COPD and the likelihood of suicide(13) | OR = 1.90; 95% CI (1.27-2.48) | Similarly, risk factors associated with suicide, such as mental disorders, are underdiagnosed and undertreated |
| Comorbid depression and risk of mortality(14) | RR = 1.83; 95% CI (1.00-3.36). | COPD increases the risk of developing depression (RR = 1.69; 95% CI 1.45-1.96) |
| Bipolar disorder and COPD(15) Schizophrenia and COPD(16) |
OR 1.55; 95% CI (1.45-1.65) OR 1.57; 95% CI (1.43-1.72) |
The most important confounding factor the contribution of which must be evaluated to clarify the nature of the association between COPD and major mental illness is the smoking |
| Stress with acute care use in COPD | AOR = 2.51; 95% CI (1.06-5.98) | The high stress group had a 2.5-fold increased adjusted odds of acute care use compared to the low stress group |
| Physical activity-depression in COPD(17) PA-anxiety in COPD |
HR = 0.85; 95% CI (0.75-0.95) HR = 0.89; 95% CI (0.79-1.00) |
The study found more physically active patients [with higher PA levels equivalent to 2.5 metabolic equivalent tasks (METs), e.g., those who report walking outside vs. those who do not] had 15% and 11% lower risks of developing depression and anxiety, respectively, compared to physically inactive patients |
OR = Odds ratio, RR = risk ratio, AOR = adjusted odds ratio, HR = hazard ratio, COPD = pulmonary obstructive chronic disease, PA = physical activity, CI = confidence intervals.
A systematic review has shown that COPD patients are 1.9 times more likely to commit suicide than people without COPD (Table 1).13 However, it is well known that the association between clinically relevant depression and COPD is bidirectional: a meta-analysis demonstrated that not only COPD increases the risk of developing depression (relative risk RR, 1.69; 95% CI, 1.45-1.96) but also, depression increases the risk of COPD adverse outcomes and mortality (RR, 1.43; 95% CI, 1.20-1.71) (Table 1).14 In a similar manner, an association between COPD, schizophrenia and bipolar disorder has been described. A systematic review found that patients suffering from schizophrenia were significantly more likely to have comorbid COPD as were patients suffering from bipolar disorder.15 It has also been described that acute care use and stress are associated in COPD. These associations are more pronounced in the low-income more high stress population who disproportionately contribute to health care utilization.16 It has been reported as a protective factor to physical activity, in COPD patients, those who perform a great physical activity are less likely to develop symptoms of depression or anxiety in the long term (Table 1).17
Moreover, as a risk factor, the evidence shows that treatment adherence in patients with COPD has a significant negative correlation with depression. In a study about medication adherence among patients with COPD treated in a primary general hospital during the COVID-19 pandemic showed that COPD with possible depression represented 31% of all cases (191 patients), and possible depression was an independent risk factor for poor treatment adherence over the past two months.18
These research data highlight the importance of the proper assessment of the screening tools when measuring depression-anxiety and its appropriate intervention in COPD patients.
Other psychiatric disorders
In addition to mood disorders, patients with COPD are more susceptible to other psychiatric disorders.
One third of patients with COPD reported post-traumatic stress disorder (PTSD) symptoms and met criteria for PTSD. In a study with multivariable analysis model, the presence of two or more exacerbations led to a near twofold increase in the prevalence of post-traumatic stress symptoms related to PTSD (PR, 1.71; p = 0.015) specially in those requiring hospitalization (PR, 1.13; p = 0.030). Overall, these findings suggest that psychological domains should be addressed along with exacerbations in COPD patients.19
Moreover, a study demonstrated a reduced survival in COPD if psychiatric comorbidity was present including substance addiction, schizophrenia, bipolar affective disorder, depressive episode, depressive disorder, anxiety episode, behavioral syndromes associated with physiological disturbances and disorders of personality.20
An high score on the type A personality scale, and an increase in risk propensity were associated with dyspnea, and a decrease in empathy score was predictor of number of infections in men with COPD.21
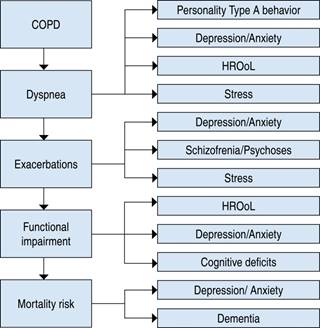
The biopsychosocial factors associated with COPD and their associated adverse health outcomes are illustrated in Figure 1, modified from latent health risk classes associated with COPD.22 Figure 2 shows some of the most common symptoms in COPD with their associated psychological factors, based on comorbidities of chronic obstructive pulmonary disease.

Modified from Latent Health Risk Classes Associated with pulmonary obstructive chronic disease.22
COPD = pulmonary obstructive chronic disease.
Figure 1: Illustrative model of biopsychosocial factors that interact in pulmonary obstructive chronic disease and its adverse health outcomes.
Psychological interventions for patients with COPD
The first-line treatment recommended in the COPD clinical practice guidelines is cognitive behavioral therapy (CBT). The CBT has recollected scientific evidence related to its effectiveness and has proven to be a cost-effective alternative. A meta-analysis and systematic review which analyzed randomized controlled trials to evaluate the effect of CBT on anxiety and depression in patients with COPD, showed that CBT can effectively improve anxiety and depression, CBT can change patients’ wrong cognitive ideas through communication and emotional management, eliminate patients’ negative emotions such as negative pessimism and low self-esteem, help patients form a healthy lifestyle and improve their quality of life.23
According to a meta-analysis CBT can serve as a complementary therapy to improve anxiety, depression, visits to emergency departments and quality of life in COPD patients and deserves more widespread application in clinical practice.24
A Cochrane review analyzing the benefits of psychological therapies for the treatment of anxiety disorders in patients with COPD pointed out that studies were heterogeneous, treatment efficacy was inconclusive, and overall quality of evidence was low.25 Therefore, well-controlled randomized trials are needed. In another more recent Cochrane review indicated that psychological therapies (using a CBT-based approach) may be effective for treating COPD-related depression; the patients improved more in the intervention (CBT) groups compared to: 1) no intervention (attention placebo or standard care), 2) educational interventions, and 3) a co-intervention (pulmonary rehabilitation). However, the effect sizes were small and quality of the evidence very low due to clinical heterogeneity and risk of bias.26
Group psychological treatments, aimed at improving functional social support, have been found to promote expansion in peer networks, since social comparison and interaction with other people with COPD offer learning opportunities, a sense of validation of the lived experience and an opportunity to make new friends, promoting the sense of belonging and identity to a group.27
In a randomized controlled trial conducted by Farver-Vestergaard et al.,28 on a group intervention that integrates mindfulness meditation with elements of cognitive-behavioral therapy, called mindfulness-based cognitive therapy for patients with COPD; was shown to be capable of achieving a statistically significant and lasting effect on psychological distress, indicating that it may be an effective complement to standard programs for patients with COPD.
The National Institute for Clinical Excellence (NICE) advises clinicians to ‘ask people with COPD if they experience breathlessness, as they find it frightening. If they do, consider including a cognitive behavioral component in their self-management plan to help them manage anxiety.29
On the other hand, a meta-analysis examined the efficacy of digital interventions on the outcomes of psychological comorbidities (depression and anxiety) related to a specific group of chronic diseases in adult populations (cardiovascular disease, stroke, diabetes, and COPD) revealing an overall moderate and significant effect on the depression outcome. However the effect on anxiety was small and non-significant.30
A survey eliciting clinician and patient perspectives on what is appropriate for ongoing health crisis, involved clinicians (n = 55) and patients with COPD (n = 19) and respondents agreed that there are activities appropriate for remote provision such as: planned activities (gathering patient information on COPD and health status, providing counseling on smoking cessation, and providing education on COPD or developing a self-management plan) and urgent care activities (triaging patients for face-to-face care and initiating use of rescue packs).31
Conclusions
Psychological comorbidities are very common in COPD, and adversely affect well-being, and quality of life. Multidisciplinary interventions including nurses, psychologists, rehabilitators, occupational therapists, home care services especially working as a team are effective in improving the condition of patients and the prognosis of evolution.
Still to be defined is to measure the impact of comprehensive care of patients with COPD, in quality of life, in prevention of exacerbations, reduction of dyspnea, adherence to treatment and survival. Thus, awareness of the importance of timely screening for these conditions should be promoted among clinicians and heightened attention should be paid to modifiable risk factors.
Psychosocial factors related to COPD should be considered for comprehensive care. Clinicians should strengthen patient supervision and monitoring; encourage integrated medical teams including pharmacists, nurses, and psychologists; and improve disease management, as well consider humane and empathetic care with patients, further studies are needed and should be focused on enhancement of adjustment to illness, preserving mental health and quality of life related to health.











 text new page (beta)
text new page (beta)