Introduction
Cholecystectomy is the second most common surgery in pregnant women, gallstones affects up to 7% of nulliparous women and up to 20% of multiparous women1. Hormonal and physiological changes during pregnancy condition gallbladder hypomotility with bile sludge formation in 31% and gallstones up to 2%2-5, however, presenting it is not an indication for intervention. Asymptomatic patients do not require treatment during pregnancy but the need for cholecystectomy during the first year after delivery is likely due to repetitive acute conditions or complications thereof 6.
Overweight and obesity are another important risk factor for this entity; the increase in the body mass index (BMI) in pregnant patients is a factor that increases the incidence of cholecystolithiasis (5), this caused by a higher concentration of cholesterol in the bile 7.
Non-obstetric acute abdomen occurs in 1/500-635 pregnant patients, the first cause being acute appendicitis and secondly cholecystitis with an incidence of 0.05-0.8% 5,7-9. For its diagnostic approach, abdominal ultrasound is the study of choice for gravid patients with suspected biliary pathology with an effectiveness of up to 90% 10 despite being an operator-dependent study.
Material and methods
A retrospective, observational study was carried out by reviewing the records of all the patients who underwent laparoscopic cholecystectomy during pregnancy from January 2017 to April 2020 at the Hospital Universitario “Dr. José Eleuterio González “. Among the variables to study are the age of the patient, weeks of gestation, clinical diagnosis, surgical procedure performed, postoperative complications, and maternal and perinatal morbidity and mortality. A statistical analysis was carried out with the JMP 10 program of the pregnant patients who underwent laparoscopic cholecystectomies, and a descriptive univariate analysis of the categorical variables was carried out by means of frequencies, percentages and numerical variables by means of measures of central tendency and dispersion.
Pregnant patients who underwent laparoscopic cholecystectomy during any of the three trimesters of pregnancy, who did not suffer severe complications of pancreatic-biliary disease (cholangitis, pancreatic collections, pseudocysts, pancreatic necrosis) who did not need a cholecystectomy as main treatment were included, otherwise patients whose data in the records were not collected in their entirety for this study were excluded.
The decision to perform cholecystectomy in the patients in our study was made jointly by the surgeon in charge of the case and the patient, knowing the risks and benefits of surgery. The indications for performing laparoscopic cholecystectomy in our patients were acute cholecystitis, biliary pancreatitis with previous endoscopic retrograde cholangiopancreatography, bile duct obstruction or risk of choledocholithiasis and cholecystolithiasis without complication data when recurrent biliary colic (more than three occasions) or when it was diagnosed during the second trimester of pregnancy.
The diagnosis of uncomplicated cholecystolithiasis was considered to be patients who presented biliary colic on one or more occasions without data of systemic inflammation, negative Murphy’s sign, without alteration in laboratory studies, with data of lithiasis or biliary sludge by ultrasound without thickening (<3 mm) or dilation of the common bile duct (<6 mm). The diagnosis of biliary pancreatitis was defined clinically (transfictional pain in the epigastrium, accompanied by nausea and vomiting) coupled with at least one of the following: increase in serum amylase value of at least 3 times the normal value or suggestive imaging data. Acute cholecystitis was classified as patients with pain in the right upper quadrant, with a positive Murphy’s sign, with systemic data on inflammation, or imaging data (increased thickness or edema of the gallbladder wall, perivesicular fluid, etc.).
The risk of choledocholithiasis was determined based on the criteria of the ASGE (American Society for Gastrointestinal Endoscopy)10(Table 1).
Table 1 Clinical predictors of choledocholithiasis according to ASGE
| Clinical predictors of choledocholithiasis according to ASGE | |
|---|---|
| Very strong | – Calculus in the common bile duct evidenced by ultrasound |
| – Ascending cholangitis clinic | |
| – Bilirubin> 4 mg / dL | |
| Strong | – Dilation of the common bile duct on ultrasound (> 6 mm with gallbladder in situ) |
| – Bilirubin level 1.8 - 4 mg / dL | |
| Moderated | – Abnormal liver biochemical tests other than bilirubin |
| – Biliary pancreatitis clinic | |
| – Age> 55 years | |
Preterm birth was considered to be that which occurs between weeks 22 and 36 weeks with 6 days of gestation, as well as spontaneous abortion when the product was lost before the 20th week of gestation or weighing less than 500 grams.
It was considered as the first trimester from conception to 13 weeks with 6 days, second trimester from week 14 to week 27 with 6 days and as third trimester from week 28 onwards.
To avoid the risk of preterm delivery induced by surgery or general anesthesia for laparoscopy, the patients entered a protocol of close clinical surveillance by the obstetrician in charge of the case, 24 hours before and 24 hours after surgery with cardiotocographic record. In the event of preterm birth, a single dose of uterine inhibitors such as indomethacin 100 mg rectally was administered and for pregnancies less than 32 weeks’ gestation. Or nifedipine 20 mg, initial dose and reassessment to escalate in pregnancies greater than 32 weeks.
Results
A total of 46 laparoscopic cholecystectomies were performed, of which only one was converted to an open procedure and only in 2 cases was it necessary to perform cholangiography during it. The average age of the patients was 25 years with a minimum of 13 years and a maximum of 41 years (Table 2). Patients from all trimesters were included, finding 6 (13%) patients from the first trimester, 38 (82.6%) from the second and 2 (4.2%) from the third.
Table 2 Population table
| Age | 13–41 years (average 25 years) |
|---|---|
| Gesta number | – 1: 11 (23.9%) |
| – 2: 7 (15.2%) | |
| – 3: 12 (26.1%) | |
| – 4: 11 (23.9%) | |
| – 5: 3 (6.5%) | |
| – 6: 1 (2.2%) | |
| – 8: 1 (2.2%) | |
| BMI | – Low (<18.5): 1 (2.2%) |
| – Normal (18.5–24.9): 22 (45.7%) | |
| – Overweight (25–29.9): 12 (26.1%) | |
| – Obesity Grade I (30–34.9): 7 (15.2%) | |
| – Obesity Grade II (35–39.9): 3 (6.5%) | |
| – Obesity Grade III (> 40): 1 (2.2%) | |
| Gestational age | – 1st Trimester: 6 (13%) |
| – 2nd Trimester: 38 (82.6%) | |
| – 3rd Trimester: 2 (4.3%) |
It was found that 11 patients (23.9%) were in their first pregnancy and 35 (76%) of them were multipara at the time of the procedure. 54% of the patients had had at least one previous episode of biliary colic.
52% (n = 24) of the patients were overweight and had some degree of obesity (26.1% overweight, 15.2% grade I obesity, 6.5% grade II and 4.3% grade III. While 45.7% (N = 21) had a normal BMI and only one patient (2.2%) was underweight.
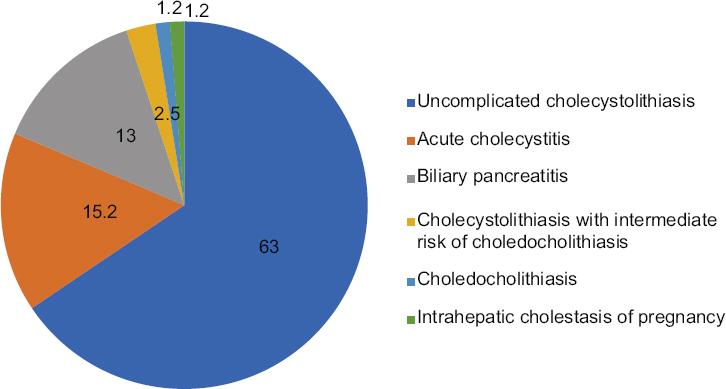
Thirty of the patients (65.2%) were admitted with the diagnosis of biliary colic with uncomplicated cholecystolithiasis, 8 (17.3%) presented acute cholecystitis, 6 (13%) biliary pancreatitis, one (6.7%) with choledocholithiasis resolved by ERCP and another patient (6.7%) with cholecystolithiasis and jaundice who, as jaundice after ERCP and cholecystectomy did not resolve, was diagnosed with intrahepatic cholestasis of pregnancy (Fig. 1)
The mean surgical time was 57 minutes with a range between 20 minutes and 2 hours and thirty minutes, only 100 cc bleeding occurred in one patient (2.2%). Regarding complications, only 3 patients (6.5%) corresponded to a bilioma, a grade I uterine lesion at the time of the umbilical trocar placement which was resolved intraoperatively without further complications and the loss of a product during the first 24 hours postoperative. The mean length of hospital stay was 8.13 days with a range between 2 and 15 days.
Of the 64 patients, 35 (76.1%) continued to monitor their pregnancy in our institution, of these 35 patients, 57.1% (n = 20) had physiological delivery, 34.3% (n = 12) surgical and 8.6% (n = 3) had product loss. One of the patients lost the product in the first 24 hours after laparoscopic cholecystectomy despite the uterine contraction inhibition measures that were performed for a gestation of less than 32 weeks, in the rest of the patients the need for use was not recorded of uterine inhibitors. In another case, fetal death was found in a control consultation, which was related to poor control of gestational hypertension, and the third was a spontaneous abortion at week 8 of gestation. It is worth mentioning that the patient was unaware of her pregnancy at the time of her surgery, which was carried out electively during week 5 of gestation. In 80% (n = 28) of the population the product reached full term and 11.4% (n = 4) presented preterm delivery. No maternal mortality was found in this series.
Discussion
Traditionally, it is accepted to perform cholecystectomy in patients with complicated biliary pathology, that is, acute cholecystitis, choledocholithiasis, biliary pancreatitis and sometimes the persistence of recurrent biliary colic, however, it has recently been described that surgery in uncomplicated biliary pathology is associated with a low rate of maternal-fetal complication11,12. Cholecystectomy is recommended in symptomatic pregnant patients since the recurrence of symptoms is found in 92% when the first episode occurs in the 1st trimester, 64% in the second and 44% in the third semester13. 23-39% of pancreatic-biliary complications have also been found in patients with conservative treatment6,9,14,15. A recurrent acute pancreatitis is associated with high morbidity and mortality in the mother and fetus5,16, with an incidence of maternal mortality of 15% and up to 60% of fetal loss8,9.
Among the main concerns during laparoscopic surgery in pregnant patients are damage to the product during insertion of the trocars, obtaining an adequate technique (which is especially difficult in the third trimester due to the gravid uterus) and the decrease in return venous to the patient during the procedure after the addition of pneumoperitoneum and compression of the vena cava. Even so, it has been found that the benefits of laparoscopic cholecystectomy are greater than conventional surgery in pregnant patients, among the benefits is less postoperative pain (which is related to less use of opioids and therefore less ventilatory depression in the product, lower rate of surgical wound complications, lower risk of thrombotic events, fewer days of hospital stay and prompt reactivation of work activities) 9,10. Intra-abdominal pressure during the procedure of 12-15 mmHg and monitoring of the product is recommended6.
Post-operative surveillance of these patients is crucial, since it is possible to use uteroinhibitory drugs depending on gestational age if it is the case of facing premature labor after laparoscopic surgery17,18. There is much description in the literature regarding individualization of these treatments and their use is safe to avoid catastrophic results6,19-22, and the use of uteroinhibitors prophylactically is not supported23,24.
In 2010 Dhupar et al. They carried out an observational study in which they compared the evolution of surgical treatment against conservative treatment of patients with a diagnosis of uncomplicated cholecystolithiasis in pregnant patients, finding that women with conservative treatment had 36% obstetric complications compared to 18% in the operated patients1. Other studies have reported a readmission percentage of between 30-70% in patients managed with conservative treatment25.
No increase in fetal mortality and preterm delivery has been found when comparing conservative versus surgical treatment. The second trimester is considered the safest to perform cholecystectomy; even so, it is considered safe to perform it during the first and third trimesters in an emergency6,25. Historically, the second trimester has been preferred for the intervention because the organogenesis is complete and the gravid uterus is not yet so large as to obstruct the vision25.
In a meta-analysis by Sedaghat et al. Up to 3.8% conversion to conventional technique has been reported26, while in our series of cases it was only found in 2.2%. Cholecystectomy is recommended in symptomatic pregnant patients since the recurrence of symptoms is found in 92% when the first episode occurs in the first trimester, 64% in the second and 44% in the third trimester. 23-39% pancreatic-biliary complications have also been found in patients with conservative treatment6,9. In our series, it was found that 54% of the patients had previously presented symptoms.
A recurrent acute pancreatitis is associated with high morbidity and mortality in the mother and fetus5, with an incidence of maternal mortality of 15% and fetal loss of up to 60% 8,9.
Cholecystectomy during pregnancy is an effective and safe procedure and should be considered as it reduces the recurrence of symptoms, obstetric complications, and hospital readmissions.
Conclusions
Laparoscopic cholecystectomy during pregnancy is a procedure that should be considered in conjunction with an obstetrician and a surgeon with experience in these cases. The complications of untreated gallstones can become risky for pregnancy, so it is preferable to perform surgery with an expert. There are obstetric complications due to surgery, they are reported in the literature, but they are minor compared to the possible consequences of not operating a complicated or on the way to get complicate condition.











 nueva página del texto (beta)
nueva página del texto (beta)