Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.19 n.2 Ciudad de México Apr./Jun. 2015
Original research
Permanent lower first molar extraction incidence in articular noises
María Julia López Vallejos,* Carlos Eduardo Buffil,§ María Mercedes GonzálezII
* Full-time Teacher at the Dentomaxillary Surgery II Chair.
§ Full-time Head of Practical work, Dentomaxillary Surgery II Chair.
II Head of the Stomatological Clinic Chair.
School of Dentistry UNNE (Universidad Nacional del Nordeste, Argentina).
ABSTRACT
Articular noises are frequently present in the daily dental practice. Some are easily discernible, nevertheless, in some other cases a trained ear might be necessary to perceive them since they might be imperceptible. In the present study, by means of a physical examination and development of a specifically TMJ-designed (temporomandibular joint) protocol dentists recorded data in individual files. Data related to onset frequency according to age and gender were equally recorded. Results revealed the fact that premature extraction of the permanent lower first molar did not bear influence on the onset of articular noises.
Key words: Temporomandibular joint, articular noise, lower molar.
INTRODUCTION
The temporomandibular joint (TMJ) is one of the most complex articulations found in the human body. It is composed of the mandibular condyle which adjusts to the mandibular fossa of the temporal bone.
The biomechanics of the TMJ represent a very complex system, since both articulations, right and left, are connected to the same bone, the mandible, and each articulation can act separately and not simultaneously.1,2
Many authors mention that due to its complexity, many alterations occur in that articulation, but not all patients suffer the same effects.
Etiology of masticatory system functional disorders has become a constant and growing controversy through time.3
In our days, the multi-causal nature of cranio-mandibular disorders (including TMJ) is well established. The influence of occlusal alterations and emotional and psychic disorders on etiology, facial neuromuscular control and mandibular posture has been clearly established.4
Articular sounds (AS) are one of the most frequent symptoms of TMJ disorders.5 They have received different names and have been reported in pre-school age children, adolescents and adults. Due to their diverse etiology and to the fact they are present at any age group, their assessment and treatment can be established by different stomatological disciplines (orthodontics, prosthesis, periodontics and surgery).
AS have received different names such as <<clicking>> <<popping>> crunches, creaking, crepitations, or closing noises.6,7 Nevertheless, presently, the terms more in use are <<clicking>> and <<crepitation>>. 8,9 These noises appear during mandibular movements, which can be opening, closing, or lateral movements. They more frequently occur in young subjects, in elderly population and in females.10
<<Clicking>> is defined as a <<noise similar to a mild or severe sudden blow, similar to the noise made with fingers>>. It is produced by the posterior displacement of the condyle, muscular un-coordination (temporal and lateral pterygoid) disk folding, mandibular trauma, prolonged mandibular opening during dental procedures, accelerated collagen refill as well as anterior disk displacement.11,12 It does not generally experience progress and appears or disappears without treatment.
According to Ogus H3 crunching is an un-coordination among functional TMJ parts. It could be caused by structural damage of articular surfaces, damage to meniscus fixation fibers or a dysfunction of the neuromuscular system which controls articular movements.
Crepitation has been defined as <<a noise similar to that elicited when creasing cellophane paper, or the noise heard when car tires circulate on sand or gravel>>.13,14
It can be caused by congenital or developmental anomalies, neoplastic proliferation, irregularities in the articular disk or in bony surfaces of the articular condyles, it can equally be due to osteophyte presence as well as lack of functional synovial fluid. AS have been associated to degenerative diseases such as osteoarthrosis and osteoarthritis.15
In spite of everything, AS have been detected in normal TMJ; they can be transitory, or generally without any evidence of progress. Bearing this in mind, it can be assumed that its high prevalence does not imply that these patients might suffer severe TMJ disorders. There is high AS prevalence in symptomatic as well as asymptomatic patients.
If we consider the fact that articular sounds are an increasing affliction of the population, it is very important that students and dentists acquire further knowledge in recognizing these sounds as instruments to prevent articulation alterations.
The purpose of the present study was to determine incidence of premature extraction of lower first permanent molar on onset of articular sounds (AS) in patients attending the School of Dentistry at the Universidad Nacional del Nordeste (UNNE) (National University of the North East).
MATERIAL AND METHODS
A cross-sectional study was conducted at the Dental-maxillary Surgery II Chair at the School of Dentistry, UNNE. 100 patients were examined. Patients were divided into two groups, they were both male and female, Argentine nationals and residing in the city of Corrientes.
The first group was composed of patients with five-year or more absence of the lower first permanent molar. These patients should not have absence of more than four teeth in the mouth. The second group was composed of patients who had preserved the permanent lower first molar and were not lacking more than four teeth.
Medical history was established for all patients, they were equally requested to sign an informed consent form which had the approval of the Bioethics Committee of the School of Dentistry.
Medical history and research protocol included the following data:
A) Medical history
1. Persona data.
2. Hereditary predisposition.
3. Personal history.
B) Visual examination
1. External observation of the face and facial profile.
Observation of facial symmetry, nose, labial philtrum, chin, lip corners etc.
Presence of obvious prognathism or retrognathism.
Observation of smile and its relation with facial esthetics: Is it symmetrical? Do teeth show when smiling? Do the gums show when smiling?
2. Simple observation of teeth and occlusion. With mirror and torch, assessment was made on absence of many teeth (which must be duly recorded), on whether present teeth presented wear surfaces and whether the upper arch was properly related to the lower arch (do inter-incisive lines coincide?).
3. Observation of articular movements.
3.1. Active opening: the patient must open his mouth to the utmost, we must assess three aspects: amplitude, symmetry and presence of pain.
Amplitude: in adults, normal opening varies from 40 to 54 mm at the inter-incisal point. With the help of a caliper we must measure the distance between upper and lower inter-incisor points. An opening larger than 54 mm often might indicate a state of hyperlaxity caused by many etiologies.
If the opening is lesser than 40 mm there is presence of a restriction which can be caused by disease of the articulation or muscles.
Symmetry: Symmetry must be found in movements of mandibular opening and closing. Any deviation larger than 2 mm from the lower inter-incisive point must be considered indicative of disease and must be explored further. We must observe the esthetic repercussions of this symmetry.
Presence of pain: presence of pain is always indicative of disease, therefore, its origin must be assessed (articular, muscular, otitis, etc). We must bear in mind that since this articulation participates in reflex movements like yawning, either we fixate it with inter-dental banding or it will be impossible to maintain it at rest position.
3.2. Forward and backward flexion movements: by this we imply the movements used to advance and retract the mandible. We will only examine the ability to advance the mandible from a resting position, since, from that position, there is barely the possibility to retract it. The amplitude of this movement is approximately 10 mm. Lesser amplitude generally indicates presence of an articular problem.
The movement has to be symmetrical, in cases when there is presence of disease, the chin deviates towards the affected site. The movement has to be painless.
4. TMJ exploration.
4.1. Bilateral external palpation: the clinician's index fingers must be placed at the front of the patient's tragus. Palpation of both sides must be simultaneous. Pain upon palpation, articular sounds or relief symmetries are assessed. Palpation is conducted with the articulation at rest as well as in opening and closing movements. If a pathological noise appears during movements, a record must be made to know at which amplitude it appeared.
4.2. Auscultation: the stethoscope is placed in the pre-tragus area and the patient is asked to perform opening, closing, retro-flexion etc movements. In normal circumstances, we should not hear any sounds, just a soft sliding. In general, crepitant sounds are normally produced by arthrosis, and clicking by disk problems. If sounds are heard, it must be noted at which movements and openings they appear.
4.3. Krough-Poulsen test: it entails biting a hard object (generally a wood tongue depressor) with the molars of the painful side. As a general rule it can be said that in cases when the pain is of muscular origin it will increase, if pain is of articular origin it will not increase.
5. Masticatory musculature exploration.
In a very simple manner we must palpate at least the masseter and temporal muscles, in search of swelling or painful areas. We must equally explore the trapezius and sternocleidomastoid muscles, bearing in mind that all cervical muscles form a group. Exploration of pterygoid muscles is more complex and must be left to specialists.
6. Exploration of mandibular movements.
6.1. Forced passive opening: it is the movement of greater interest to us in the assessment of passive tests.
In normal circumstances, forced opening should only increase the active opening of the patient by 1 or 2 mm, it should not be painful. Pain is a disease indicator. If we find resistance, we should record at which opening degree it appears, and we must describe whether it is a rigid resistance (articular origin) or elastic resistance (muscular or simulation origin).
6.2. Movements against resistance: these are opening and closing movements, movements of forward flexion etc. Basically they represent musculature exploration and should not elicit pain.
Obtained data must be recorded in a file in order to process them at a later date.
RESULTS
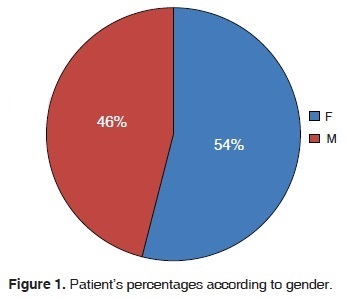
100 cases were analyzed. Patient average age was 29.54 years. 54% of all patients were female (Figure 1). This figure coincides with existing high female attendance to the service, therefore, it is not an indicator that articular sounds appear more in males than in females.
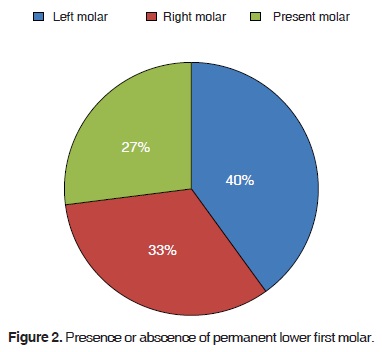
Permanent lower first molars were observed in the following manner: left lower first molar in 40%; right lower first molar in 33%, and presence in 27% without noting differences between left and right (Figure 2).
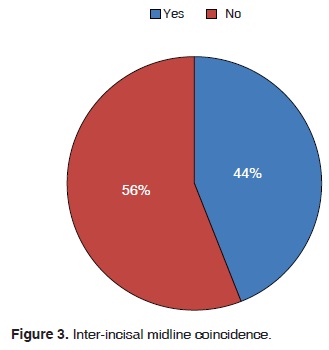
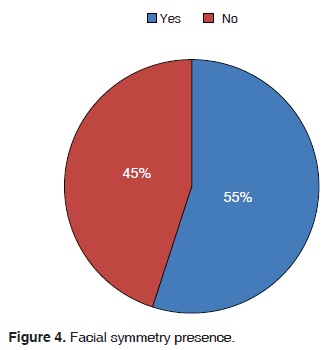
Upon analysis of facial symmetry and inter-incisal midline the following could be observed: 55% presented facial symmetry (Figures 3 and 4), from those values it could be assumed that 35% exhibited articular sounds.
CONCLUSIONS
Extraction of lower first molars does not directly affect the presence of articular sounds.
Presence of articular sounds is an indication of the onset of temporomandibular alterations.
Association of tooth extraction with midline deviation exhibits incidence in articular sounds onset.
In the professional daily practice it can be established as a simple diagnosis method to prevent TMJ complications.
REFERENCES
1. Winkler S. Prostodoncia total. México: Editorial Limusa Noriega Editores; 2001: pp. 25-26, 554-555. [ Links ]
2. Okeson JP. Tratamiento de oclusión y afecciones temporomandibulares. 5ta edición. España: Editorial Elsevier; 2003: pp. 147-364. [ Links ]
3. Ogus H. Mandibular joint. Internal reanaangement. Brit J Oral Maxilofac Surg. 1987; 25 (1): 118-126. [ Links ]
4. Agerberg G, Carlsson G. Functional disorders of the masticatory system: I distribution of symptoms by questionnaire. Act Odont Scand. 1972; 30 (6): 597-613. [ Links ]
5. Egermark-Erkisson I, Carlsson GE, Ingervall R. Prevalence of mandibular dysfunction and orofacial parafunction 7-11 and 5 years old Swedish children. Eur J Orthod. 1981; 3 (1): 163-165. [ Links ]
6. Drum R, Litt M. Spectral analysis of temporomandibular joint sounds. J Dent. 1987; 58: 485-494. [ Links ]
7. Stockstill JW, Molh N. Valoración de ruidos de la articulación temporomandibular. Análisis, diagnóstico e implicaciones clínicas. Clínicas odontológicas de Norteamérica. México, D.F.: Nueva Ed. Interamericana. [ Links ]
8. Mhol ND, Zarg GA, Carlsson GE, Bugh JD. A textbook of occlusion. Chicago: Quintessence Publish in Co. Inc.; 1988. [ Links ]
9. Widlmalm SE, Westesson PL, Brooks SL et al. Temporomandibular joint sounds: correlation lo joint structure in fresh autopsy specimens. Am J Orthod Dentofac Orthop. 1992; 101: 60-69. [ Links ]
10. Erkson IC, Ingervall B, Carlsson GE. The dependence of mandibular dysfunction in children on funtional and morphologic malocclusion. Am J Orthod. 1983; 107: 194. [ Links ]
11. Westsson PL, Brostein SL, Liedberg JL. Internal degenerament of the temporomandibular joint: morpholoic description with correlation to joint function. Oral Surg Oral Med Oral Pathol. 2003; 59; 323-331. [ Links ]
12. Westesson PL, Eriksson L, Kurita K. Reliability of a negative clinical temporomandibular joint examinations: prevalence of disk displacement in asymptomatic temporomandibular joints. Oral Surg Oral Med Oral Pathol. 2005; 68: 551-554. [ Links ]
13. Rubiano M. Placa neuromiorelajante: elaboración y mantenimiento paso a paso. Bogotá: MRC Editores; 1990. [ Links ]
14. Runge M, Sadowsky C, Sakols E et al. The relationship between temporomandibular joint sounds and malocclusion. Am J Orthod Dentofac Orthop. 1989; 96: 36-42. [ Links ]
15. Helkimo M. Studies on function and dysfunction of masticatory system. IV. Age and sex distribution of symptoms of dysfunction of the masticatory system in the north of Finland. Acta Odontol Scand. 1994; 32: 255-267. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
María Julia López Vallejos
E-mail: mjulialopez@hotmail.com











 text in
text in 


