Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.16 no.4 Ciudad de México oct./dic. 2012
Case report
Problematic feeding in newborn patient, stomatological approach. Case report
Américo Durán Gutiérrez,* Érika Berenice Castillo Mancilla,§ Eduardo de la Teja Ángeles,II Jaime A Ramírez Mayans¶
* Physician Attached to Pediatric Stomatological Service at the Pediatrics National Institute. Specialty Associate Professor.
§ Former Resident, National Pediatrics Institute.
II Head of Pediatric Stomatology, National Pediatrics Institute.
¶ Head of the Gastro-nutrition Service, National Pediatrics Institute.
ABSTRACT
One of the newborn's main functions in life is feeding. This vital mechanism is performed through proper suction and deglutition as well as coordinated respiration. These functions enable the newborn to feed properly. Nevertheless, sometimes, we find patients who, due to their physical characteristics, genetic syndromes (Treacher-Collins, Pierre Robin, lip and palate clefts) or neurological characteristics such as psychomotor retardation or arthrogryposis, are conditioned to difficult feeding. It is therefore important to establish a treatment protocol to efficiently treat these patients, so they don't end up, as first instance, with gastrostomty cases. It is also important to recover functions, to enable feeding after the use of probes and syringes or other devices. A multidisciplinary approach is fundamental for these cases. Based on a scientific literature review of these cases, we present the case of a patient, presenting Treacher-Collins syndrome. The patient presented feeding difficulties in neo-natal phase. We inform of recommended treatment up to the point of complete reinstatement to normal feeding physiology. We deem necessary to assess the characteristics of these patients as well as indications for treatment than cannot be considered conventional.
Key words: Difficult feeding techniques, genetic syndromes, multidisciplinary.
INTRODUCTION
Feeding implies an important challenge when the patient presents genetic syndromes that involve improper development of craniofacial structures, other genetic syndromes such as Treacher-Collins, Pierre Robin sequence facial-auricular-vertebral spectrum, as well as all syndromes presenting clefts in the lips or palate (Table I), as well as patients afflicted with neurological disorders which might condition a difficult feeding process. A multidisciplinary approach is therefore fundamental to achieve full adaptation or reinstatement to feeding basic functions.
Until the XVIII century, almost all live newborns were breast-fed, either by their mother or a nurse. Breastfeeding was vital for newborn survival.1
Establishment of breastfeeding depends on a learning and adaptation process between mother and infant. The first breastfeeding experiences, that is to say, the first oral experiences of the infant are vital to the later development of the breastfeeding process.
Proper feeding depends on the mother, the infant, technique and environmental factors present at that particular time. They can result in success or represent a risk for the infant's survival.2
At birth, identification of the infant's adaptive reflexes such as suction, deglutition and search are needed to initiate the process of feeding. Search reflex is the infant's automatic reaction when his cheek is being caressed. It consists on turning the head towards the stimulated side, and beginning to suckle.3 Suction is probably the most important event during breast-feeding. Through this mechanism the infant transfers milk from the breast to the oral cavity. At the same time it triggers a series of reflexes (oxytocin and prolactin release) which regulate synthesis and flow of milk. This becomes evident when observing proper pressure of the lips, as well as generation of negative pressure to bring flow to the oral cavity.4 Even though newborns apparently easily swallow suctioned milk, their deglutition process is still inefficient. This physiological action requires complex neuromotor coordination as well as a complex mechanism5 dependent upon maturation of nervous system. This process takes place in three phases: one voluntary and two reflex phases. When food voluntary mastication is completed, in the oral phase, bolus is brought to the jaws; this action stimulates the rich neural network of the pharynx. In a reflex manner, the soft palate elevates towards the retropharynx. The larynx elevates as well and the pharynx practically closes down. Vocal cords become close together, and breathing is momentarily interrupted so as to complete the pharyngeal phase. Afterwards, the pharynx opens to allow passage of the bolus to the esophagus, where with the help of peristaltic waves it is propelled towards the stomach (Keele and Neil, 1971). Over 30 muscles play a part in the aforementioned movements, therefore, it would be logical to conclude that in order to coordinate all these muscles it is necessary for the neural network to be fully mature.6
In the newborn, feeding is guaranteed by the presence of the aforementioned adaptive reflexes, as well as those reflexes targeting the protection of airways (extrusion, bite, vomit and cough). At the 4th or 5th month of life, this reflex action undergoes a shift towards a voluntary conduct pattern. This is due to the growth of the facial and oral structures, to the maturation of the nervous system, and to the repetition of oral experiences as a function of the feeding process.2 All the aforementioned facts pertain to a healthy newborn.
FEEDING IN SPECIAL CHARACTERISTICS PATIENTS
Oral dysfunctions are disorders of the proper suction-deglutition pattern. They can be primary or secondary dysfunctions. Primary dysfunctions are a consequence of immaturity, of individual anatomical characteristics that hinder proper fit. Defects in the first and second branchial arch result in the lack of fundamental structures which enable feeding, they can also give rise to neurological alterations.7,8 These neurological alterations can be transitory or permanent, and they hinder the newborn's position during the process of suckling, forcing the infant into acquiring atypical postures.9 Secondary oral dysfunctions arise when the newborn modifies his original deglutition-suction pattern in order to avoid facial pain (use of forceps) or due to certain deleterious habits such as the use of a pacifier and nursing bottle during the neonatal period.2
CLINICAL ASSESSMENT
Clinical assessment is paramount to achieve a proper diagnosis.10 First, all personal data of the newborn must be recorded, as well as the reason for the consultation. Proper history must be taken, geared towards pediatrics data, oral, facial and myofunctional assessment, as well as evaluation of nutrition and assessment of deglutition. The physician responsible for this assessment must thoroughly be cognizant with healthy newborn physical and physiological characteristics, as well as characteristics pertaining to newborn affected by different conditions. One of the main questions that must be asked is whether the patient is afflicted with any disease, since, many of the disorders which induce difficult feeding can be, either neurological disorders secondary to postnatal hypoxia (psychomotor retardation, central origin motor insufficiency) or they can be a component of a genetic syndrome (Treacher-Collins, Pierre Robin, vertebral-auricular-facial spectrum, arthrogryposis, etc.), all the aforementioned are conditions which would be the basis for a variety of diagnosis within the same patient.
ORAL-FACIAL AND MYOFUNCTIONAL ASSESSMENT
a) Assessment of muscle tone and forces as well as posture control of head and neck:
• Alterations in muscle tone influence in oral-facial function, and conversely, lack of control in head and trunk cause difficulty to dissociate movements of the head with respect to the movements of lips, jaw and tongue.
b) Assessment of oral phase and gestures:
• Face expression, face coloring.
• Face contour and facial asymmetry.
• Sialorrhea.
• Saliva: amount and consistency.
• Tongue, length of frenulum.
• Velum of soft palate, size and mobility.
• Uvula: shape and position.
• Quality of crying.
• Color of gums.
• Lips: presence of asymmetries.
c) Sensitivity assessment:
• Tongue sensitivity (reaction to tactile or taste stimuli).
• Sensitivity of the oral mucosa.
d) Assessment of reflexes.
• Search reflex.
• Suction reflex.
• Deglutition reflex.
Assessment must be established of whether these reflexes are present, hyperactive, absent, or whether primitive reflexes are present.11
e) Ventilatory function assessment:
• Ventilatory mode: nasal or oral breathing.
• Thoracical enlargement.
• Respiratory rhythm.
• Apnea.
• Oxygen saturation.
f) Assessment of nutrition modality
• Assessment of suction mode (whether it is normal, whether it coordinates suction-deglutition with respiration, whether the child tires when feeding).
A child afflicted with oral motor dysfunction generally exhibits some of these conditions:
1. Hypertonia. The whole body exhibits increased motor tone. The head shows tendency to extension. When the infant is held from the waist (girdle), arms are firmly pointing downwards. When examining the mouth, it is felt that the child bites the finger and strongly pressures it against the hard palate. In these cases, it is recommended to sit the child in front of the mother, in as much as possible a fetal position, so as to relax the newborns facial muscles. It is also recommended to massage the lower gums of the newborn before undertaking the feeding process.
If the child causes the mother to experience sharp pain or develop cracks in the breasts, she can extract her milk and feed the child with a probe o glass, during the time it takes for the hypertonia to abate. This process takes place in a few days, with the help of maturity and massages.
2. Hypotonia. Body tone is decreased. The newborn's head is not firmly into place and when the child is held by the waist, his arms show tendency to raise. This condition is more frequent in children born underweight. When suckling, the child exerts very little, irregular pressure, and milk runs off from the lip corners. In these cases, it is useful for the mother to hold the child's chin while having the child sitting with secured head and back. Sometimes it is necessary to use some devices, like syringes or pacifiers, to help the newborn and prevent him from tiring during the feeding process.
Deglutition disorders are varied, and possess different origins. They encompass dysfunctions pertaining to efficiency and/or security in the deglutition function. Presence of these alterations is correlated with poor nutritional state, increase in morbidity and mortality, pneumonia, and disability among survivors of diseases which warrant critical care.12
BASIC FEEDING TECHNIQUES
The main problem of feeding disorders in the newborn is closely related to lack of coordination with the breathing process. Parents must be educated into realizing that techniques must not interfere.13 As an example we can mention FLAP, where sealing plates are placed14 to separate oral way from nasal cavity, as well as ensuring vertical position to ease the passage of the bolus,15 lateral decubitus position in dysmorphiae in order to avoid glossoptosis, decreasing the diameter of the feeding bottle in cases where the patient possesses deglutition and suction abilities, but tires easily (cardiopathies, neuropathies, FLAP). Parents must be very patient and count with proper medical counseling.3 The use of certain devices, like taps in the feeding bottle, adaptation of pacifiers to syringes to propel milk, or drop-by-drop feeding are also recommended when feeding disorders do not endanger the patient's life, and it is just a case of integrating the newborn into normal function.16
GASTRIC PROBE, TRANSPYLORIC TUBE AND GASTROSTOMY
Gastric and transpyloric probes are warranted when nutritional requirements are not ideal, and weight gain is seriously compromised.17 Enteral feeding for longer than 3 months is recommended for patients with total or partial inability to swallow, patients who experiment inability to gain weight and growth, and for children with associated surgical conditions.18
HOLISTIC APPROACH TO POOR FEEDING
Poor feeding can be caused by any defect involving the gastrointestinal system. Therefore, patients with oral and facial characteristics hindering proper feeding must be treated with well pre-established plans. This treatment must be devised by inter-disciplinary teams including gastroenterologists, neonatologists, therapists, surgeons, and stomatologists. All these professionals constitute the minimum required group to conduct initial approach of the problem. If improper treatment is administered, atrophy of feeding mechanisms will ensue.
INTEGRATION TO FEEDING
Once the newborn's initial feeding emergency is redressed with placement of gastric or transpyloric probes or gastrotomies, the newborn must be properly reinstated to a suitable digestive system. This must start with the mouth, pharynx, epiglottis, cardia, stomach and pylorus.
SUCTION AND DEGLUTITION STIMULATION
Safe and successful feeding in newborns (NB) and infants require proper and well coordinated sequence in the suction, deglutition and breathing processes. This suction-deglutition-breathing sequence requires integration of multiple afferent and efferent pathways of the nervous central system. One of the most complex neuromuscular units in the human body is the upper digestive tract, which acts as a conduit for passage of air and food. Deglutition (suction-deglutition-breathing) is a complex and integrated event, requiring the participation of several cranial nerves (V, VII, IX, X, XI, and XII), brainstem and cerebral cortex, as well as 26 muscles of the mouth, pharynx and esophagus. This mechanism enables NB and infants to suction and swallow efficiently and rapidly, greatly reducing the duration of the respiratory pause, thus allowing proper feeding.11,19
Certain disorders can compromise deglutition (e.g. William-Beuren syndrome, moebius, Prader-Willi, Rubinstein-Taybi, psychomotor retardation, etc). Acquired or hereditary damage to the central nervous system during neonatal period, can lead to feeding difficulties, such as slow or weak suction. This finding can well be the first sign indicating that the newborn suffers some neurological problem. Deglutition disorders are common in infants who will later develop cerebral palsy or infants presenting other developmental problems. Infants suffering genetic syndromes, frequently suffer feeding and deglutition difficulties as a result of the complex interactions among anatomical, medical, physiological and behavioral factors. As an example we could mention neuromotor coordination disorders in Down's or Prader-Willi syndrome patients. These alterations are due to hypotonia, poor control of the tongue, and tendency to keep the mouth constantly open. These facts frequently interfere with acquisition of effective oral-motor skills, leading thus to feeding difficulties.19
It has been suggested that circum-oral stimulation boosts the immature or neurologically compromised infant's ability to coordinate suction and deglutition. This stimulation is performed on the skin located above masseter and orbicular muscles of the lips. Rapid, one second pressure is applied following the nerve path. Circum-oral stimulation takes place, touching the cheeks from the TMJ towards the corner. Pressure is applied with index and thumb. With the index finger, moderate pressure is exerted in a circular manner in the cheeks area. With thumb and index, circles are traced around lip muscles exerting moderate pressure. With thumb and index, lower and upper lip are alternately protruded. Index is rapidly passed over the upper lip, then over the lower lip. These exercises must be conducted by physical rehabilitation experts. The pediatric stomatologist can also perform them, in cases when he feels trained to do so. These type of actions highlight the need to count with an inter-disciplinary team to tackle the problem.3,20-22
INTEGRATION OF GASTRIC FUNCTION AND PROPER FORMULA
The fact of being aware that suction and deglutition reflexes are maintained does not warrant initiation of feeding. An interdisciplinary treatment must prevail. Placing transpyloric probes for a long time greatly deteriorate gastro-esophageal function, this is due to its disuse. When removing the probe, the patient, as part of survival instinct, will suction and swallow, nevertheless he will quite probably sustain emetic events. These events will bring latent risks of dehydration and hyperemia, which might endanger his life.
CHOICE OF FORMULA
Selected formula will depend on age, gastrointestinal functioning and diagnosis of patient. Mode of administration must also be considered. Choice of formula must be individual. Amount and quality of nutrients must be assessed, as well as micronutrients coverage. Interconsultation with pediatric gastroenterologist physician is always required, since this specialist is who will decide upon proper formula to cover requirements of each individual patient.23-25
SURGICAL TREATMENTS
Osteogenic distraction in patients afflicted with Pierre Robin sequence or syndrome, is a surgical solution for the formation of new bone. This technique provides elongation of the bone callus after a surgical fracture has been performed. This procedure targets promotion of rapid growth of the lower jaw, facilitating thus breathing. This technique is also indicated in Treacher-Collins cases, facial-auricular vertebrate spectrum, etc.26 Another alternate procedure used is to locate a traction point at the base of the tongue for severe apnea cases due to glossoptosis, or the decrease of the base of the tongue with the use of a harmonic scalpel.27
CLINICAL CASE
Two month old female patient, with base diagnosis of Treacher-Collins syndrome. The patient was referred to the stomatological science service from pediatric out-patient service, due to her difficulties in feeding. The mother informed the patient was at the time fed with a transpyloric probe. This probe had been placed approximately six weeks before, seeing that the patient experienced difficulties in the feeding process and suffered reflux and weight loss.
Physical examination revealed patient's characteristic facial traits: malar hypoplasia, bilateral microtia with low implantation, artresia of both ear canal, lower lid bilateral coloboma, wide nasal bridge, oral cavity with uvula, complete hard and soft palates, short neck, thorax devoid of alterations (Figure 1).
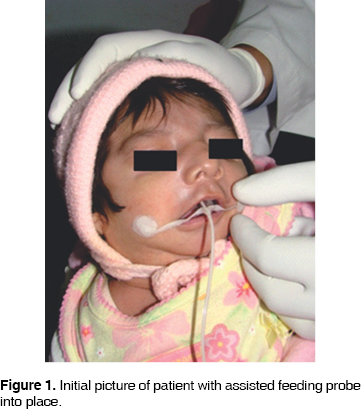
Search and suction reflexes were stimulated. Search reflex is elicited when the infant's check is caressed. In this instance, a proper response was obtained, since the patient turned the head towards the stimulated side. To confirm presence of suction reflex, the index finger was introduced into the patient's mouth and pressure was exerted against the palate. At this point, the child exerted pressure upon the finger, and the tongue was able to embrace the finger to then perform a peristaltic movement. After studying these responses, it was determined that born reflexes were not compromised. Consultation with the out-patient pediatric service was undertaken to remove the oral-gastric probe. In the absence of any contra-indication, the probe was withdrawn. The mother was instructed on how to achieve the feeding technique based on syringe and pacifier. The mother was willing to undertake the treatment (Figure 2).

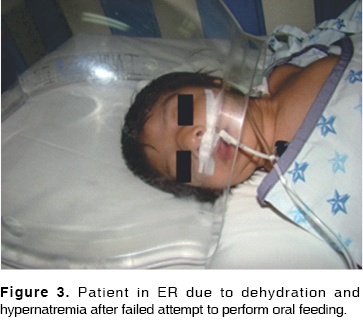
The next day, the mother requested opening of a clinical file at the pediatric out-patient service where staff attempted to achieve suction and deglutition processes. The pediatrician diagnosed absence of these reflexes, since, when feeding, there was milk runoff through the corners of the lips. This was due to the patient's inability to swallow. When taking clinical history, pallor and respiratory pause were observed. The child was instantly stimulated and recovered on the spot. The child was at that point referred to emergency prehospitalization service (Figure 3). As a result of probe removal, the child experienced emetic and dehydration events. These events conditioned presence of hypernatremia (increase of sodium level in the blood). This can cause muscle spasms and death, as well as dehydration and malnutrition. This case was important to highlight the fact that interdisciplinary approach must prevail in all treatments of this kind, and also the need to avoid making unilateral decisions, since this might endanger a newborns life. Management of this patient was not optimal, since the child was exposed to unnecessary risks. Adventuresome, unsupported decisions were taken. Upon removal of the transpyloric probe the patient experienced vomiting caused by formula intolerance. A gastroenterologist physician should have been consulted to devise the proper formula according to the child's nutritional requirements. This leads us to suggest a diagnostic pathway for this type of patients, so as to be able to establish proper treatment. We present the following algorithm based on information found in scientific literature (Figure 4).
The first step to undertake therapeutic route in the newborn afflicted with feeding problems is to determine the deficiency which causes the problem, whether it be motor, physical or neurological. After this, the origin of the deficiency must be established to determine whether it is part of a genetic syndrome or an isolated event.27 Born reflexes such as suction, deglutition, search and SNC and cranial pairs evaluation must be included in the neurological evaluation.3
In cases of structural deficiency such as in cleft palate and lips, placement of special devices might be required, such as bottles or orthopedic plates, to simplify the feeding process.26
Nutritional intervention should be recommended, enteral or supplement nutrition in cases of calorie and protein malnutrition (nutritional index < 90%), irrespectively of whether ingestion is proper or not, five days before the indication. In cases when nutritional situation does not improve, gastrotomy will be indicated.29
DISCUSSION
In 2007, Durhand informed on the fact that successful breastfeeding depends on a learning and adaptation process taking place between mother and infant. The newborns first oral experiences are of paramount importance for the later development of breastfeeding. Facts related to the mother, the newborn, the breastfeeding techniques and hospital practices can hinder initiation of proper breastfeeding and doom it to failure. Frequently we find that full term newborns, in good health, and showing no apparent problems which might interfere in the development of proper breastfeeding habits, present atypical conduct or oral movements during the process of breastfeeding.2 Mariela Costas, in 2004, mentioned the fact that suction is one of the newborn's first and most complex motor-sensitive integrated skills. The action of sucking mainly develops to cover nutritional requirements of the child. The mother's behavior provides proper environment optimizing feeding efficiency, as well as growth and development: this is an interactive process between mother and child.4 McGuire et al., in 2007, mention that premature newborns are likely to present poor suction and deglutition coordination, which can in turn delay safe oral feeding. Enteral feeding can be provided with the help of a catheter passing from the nose or mouth into the stomach or to the upper part of the small intestine.15 Udaeta-Mora, in 2004, refer that the standard by which efficient feeding in the newborn is measured is to match it to intrauterine growth rate. At birth, newborns present a transition period in which loss of body weight occurs. This is especially the case of low weight, critically ill, pre-term infants.17 Presently, at the National Institute of Pediatrics (NIP) children are assessed following a multi-disciplinary approach, bearing in mind the possibility of finding several disorders which might warrant assisted feeding. It is necessary to remember that, as important as providing assisted feeding, is the fact of reintegrating the newborns to an autonomous mode of feeding.
CONCLUSIONS
Feeding is not an isolated function. It is the initiation of the digestive process which leads to gathering nutrients needed for indivudal's growth and development. Treatment of patients afflicted with feeding difficulties must be approached in a multi-disciplinary manner. Appropriate specialties must be part of this treatment, stomatology, neonatology and gastroenterology are but the basic ones. It is possible that, depending on the origin of the disorder, other specialists might have to be consulted. These specialists could be proficient in genetics, maxillofacial surgery, oncology, cardiology, immunology, plastic surgery, etc. It might also be possible to find a situation where the newborn possesses some intact functions such as suction and deglutition, but this does not mean that he is ready to feed by himself. On the other hand, the digestive apparatus might be intact, but nevertheless presenting functional limitations caused by defects of the oral cavity. A proper assessment is of paramount importance to attain success in the treatment of these patients. A multidisciplinary team is of vital importance. The timing of each specialist's intervention even more so, always in conjunction with the pediatric stomatologist. The fact of seeking specialist consultation does not imply disengagement from the patient. On the contrary, the new specialist must be requested to participate in the group of experts who will treat the patient until his complete recovery.
REFERENCES
1. Ortiz AA, Peña LQ. Lactancia materna y salud publica en nutrición. Rev Salud Pública y Nutrición 2006; 82: 753-67. [ Links ]
2. Durhad SB. Disfunciones orales en el inicio de la lactancia materna. En: IV Congreso Español de Lactancia Materna, 2006, Tenerife. Anales del IV Congreso Español de Lactancia Materna, 2006. [ Links ]
3. Fragoso RJA. Estomatología del recién nacido. México, D.F. Editorial Diseño y Publicidad; 1992. [ Links ]
4. Costas M, Santos S, Godoy C, Martell M. Patrones de succión en el recién nacido de término y pretérmino. Arch Pediatr Urug 2004; 75: 36-50. [ Links ]
5. López HN, Padín HM, Bennet RE. Presencia de la disfagia en los trastornos neurológicos de la comunicación. Rev Mex Neuroci 2004; 5: 455-9. [ Links ]
6. http://www.cheesehosting.com/saludinfantil/nutricion+infantil+desarrollo+deglucion.html
7. Ruiz de LA, Clavé P. Videofluoroscopia y disfagia neurogénica. Revista Española de Enfermedades Digestivas 2007; 99: 3-6. [ Links ]
8. Cabrejas RM. Trastornos de la deglución del niño: Evaluación y tratamiento fisioterápico. Fisioterapia y Rehabilitación México 2008: 1-7. [ Links ]
9. Arancibia JC. Secuencia de Pierre Robin. Neumología Pediátrica 2006; 1: 1-41. [ Links ]
10. Arteaga JP, Olavaria LC, Naranjo DB, Elgueta LF, Espinola MD. Cómo realizar una evaluación de la deglución completa, eficaz y en corto tiempo. Rev Otorrinolaringol Cir Cabeza Cuello 2006; 66: 13-22. [ Links ]
11. Taveras EM, Li R, Grummer S, Richardson M. Opinions and practices of clinicians associated with continuation of exclusive breastfeeding. Pediatrics 2004; 113: 283-90. [ Links ]
12. Domínguez TC, Gómez MG. Trastornos de la deglución en el paciente en estado crítico. Lecturas Sobre Nutrición 2004; 11: 55-71. [ Links ]
13. Kramer FJ et al. Quality of life and family functioning in children with nonsyndromic orofacial clefts at preschool ages. Journal of Craniofacial Surgery 2008; 19: 580-7. [ Links ]
14. Sala MS, Merino T, Escuin HT. Evaluación protésica en pacientes fisurados labiopalatinos. A propósito de un caso con comunicación oronasal. Med Oral Patol Oral Cir Bucal 2006; 11: 493-6. [ Links ]
15. Riordan J, Averhback K. Breastfeeding the infant with special needs: cleft lip and palate. Breastfeeding Resource Guide 1997: 4-5. [ Links ]
16. McGuire W, McEwan P. Alimentación por sonda transpilórica versus alimentación por sonda gástrica para los recién nacidos prematuros (Revisión Cochrane traducida). En: La Biblioteca Cochrane Plus 2008; 3. Oxford, Update Software Ltd. Disponible en: http://www.update-software.com. (Traducida de: The Cochrane Library, Issue. Chichester, UK: John Wiley & Sons, Ltd. [ Links ]).
17. Udaeta-Mora E, Toussaint G, Martínez de Castro B, Pérez-Marín P, Carmona-Rodríguez M. Alimentación enteral en el recién nacido pretérmino y de término con bajo peso: estado actual en México. Gac Méd Méx 2005; 141: 283-290. [ Links ]
18. Fiorentino JA. Evaluación del botón de gastrostomía implantado quirúrgicamente: Técnica y dispositivo para una gastrostomía segura. Rev del Hospital de Niños de Buenos Aires 1997; 39: 88-95. [ Links ]
19. Lawrence RA, Lawrence RM. Breastfeeding. A guide for the medical profession. 6th ed. St. Louis: Mosby, 2005. [ Links ]
20. Souto S, González L. Fisioterapia orofacial y de reeducación de la deglución. Hacia una nueva especialidad. Fisioterapia 2003; 25: 248-92. [ Links ]
21. Castells BM. Terapia miofuncional y logopedia. Rev Logop Fon Audiol 1992; 9: 85-92. [ Links ]
22. Lama MR. Nutrición enteral. Rev Protocolos Diagnósticos y Terapéuticos en Pediatría 1997: 5; 335-6. [ Links ]
23. Cebrian CJ, Muñoz CJ, Chamorro PM, García AL, Morán SM, Burgueño GM. Tracción de la base de la lengua mediante fijación para el tratamiento de la apnea del sueño. Revista Esp Cirugía Oraly Máxilofacial 2003; 25: 303-11. [ Links ]
24. Ortiz-Monasterio F, Berlanga RF. Cirugía plástica reconstructiva. Gac Méd Méx 2004; 140: 176-81. [ Links ]
25. Salinas-Valdebenito L, Núñez-Farias AC, Milagros A, Escobar-HRG. Caracterización clínica y evolución tras la intervención terapéutica de trastornos de deglución en pacientes pediátricos hospitalizados. Rev Neurol 2010; 50: 139-44. [ Links ]
26. Ordóñez RA. Recién nacido, alto riesgo, prematuro y postmaduro alto y bajo peso. Hosp Gen Méx 2003. [ Links ]
27. Robaina CGR, Riesgo RSC, Robaina CMS. Evaluación diagnóstica del niño con parálisis cerebral. Rev Cubana Pediatr [revista en la Internet]. 2007 [citado 2010 Mayo 03]; 79 (2). [ Links ]
28. Zulma I, Campos M. Feeding problems in infants. First part: basic concepts. ISSN 1409-0090/2009/21/1/18-25. Acta Pediátrica Costarricense 2009. [ Links ]
29. Bautista CA, Broto MJ, Benavent GM, Elías Pollina J, Roqués SJL, Tovar L JA. Protocolo de nutrición enteral en cirugía pediátrica. Comité de Nutrición de la Sociedad Española de Cirugía Pediátrica. Acta Pediátrica Española 2004; 62: 10. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
Américo Durán Gutiérrez
E-mail: dramerico@hotmail.com











 texto en
texto en 


