Introduction
Since its origins, the human being learned to take advantage of animal, mineral, and plant peculiarities for healing purposes; this knowledge was developed empirically, based on trial and error, and surely as a result of great observation capacity. This way, an effect-based knowledge was gradually built, but without the scientific bases to explain the different properties of the used elements. This document aims to address an 18th century prescription to make an approach to the scientific basis that allows explaining its greater or lesser success in the treatments it was intended for.
The ancestral use of medicinal plants is attributed to the experience of indigenous people, royal physicians, and doctors from different eras of New Granada medicine, who were able to directly perceive elements in nature that are useful to therapeutics that confront disease, thus allowing the development of medical prescriptions that were widely used in the New Kingdom of Granada for the management diseases. The arrival of different manuscripts brought from the old continent, coupled with American natives’ knowledge based on their own flora, and enriched medical practice. In this process, the training of local physicians was led by José Celestino Mutis (1732-1808), pioneer in the creation of chairs of medicine in Santa Fe. Mutis managed to merge medicine and botany by giving importance to phytotherapy, which, in those days, was the main source of health with herbal agents for treating mild or moderate diseases, as well as an adjuvant in chronic diseases such as insomnia or depression, among others1.
Palpitations are a common symptom in doctors’ practice, and it is referred to as an abnormal and uncomfortable sensation of vigorous heartbeats or contractions, described in the chest and/or neck as pounding or jerks that sometimes are associated by patients with a sense of “impending doom.” These are an underlying symptom in various heart diseases of electrical or structural and not cardiac nature2-4. In the mid-18th century, New Granada’s medical advances were influenced by knowledge and practices that were essentially Spanish; nevertheless, the pathophysiology of palpitation-associated diseases was unknown.
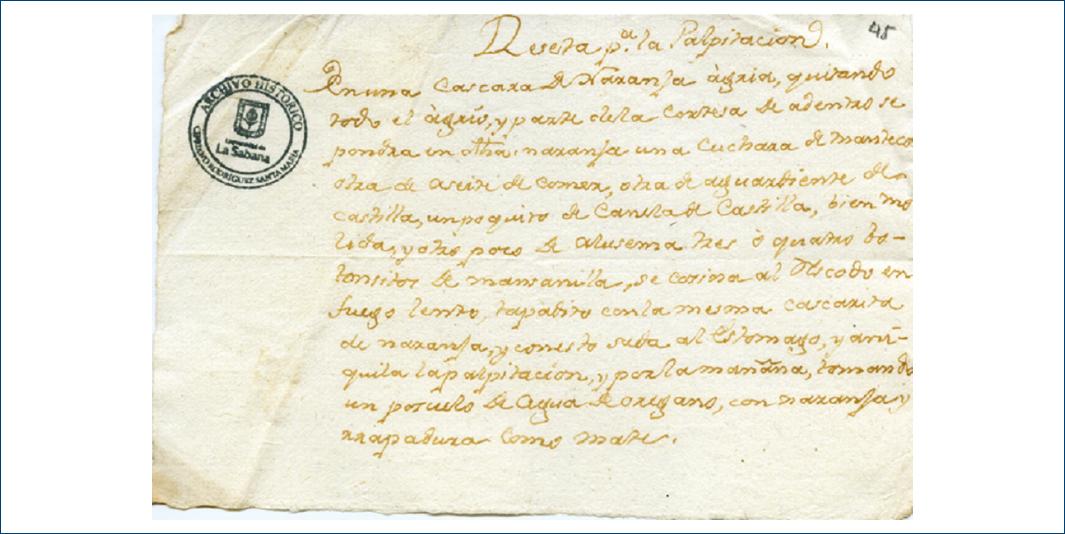
The Cipriano Rodríguez Santa María historical archive, of the University of La Sabana, has different medical prescriptions of the 18th and early 19th centuries. Among these, it preserves a prescription about practices of more than 2 centuries ago, the purpose of which was the treatment of palpitations (Fig. 1). A historical look at the past allows understanding the scientific bases that support phytotherapy, back then an entirely empirical medical practice.
Materials and methods
Historical, cultural, and scientific review, based on the document called “Prescription for palpitations,” preserved in the Cipriano Rodríguez Santa María historical archive of the University of La Sabana. A search was carried out in the ScienceDirect, ClinicalKey, Ovid, PubMed, and SciELO databases, using the terms “palpitaciones” (palpitations), “fitoterapia” (phytotherapy), “historia” (history), “fitoquímicos” (phytochemicals), and “history of 19th century,” with no time limits and English and Spanish language. Once the information was collected, a review of modern heart palpitations definition, pathophysiology, and treatment was carried out, as well as of the 18th and 19th centuries medical advances in the New Kingdom of Granada. Simultaneously, the phytochemicals found in the prescription and their possible mechanism of action in the management of palpitations or underlying diseases were described.
Transcription of the source document
“Reseta para la palpitación (original spelling of the manuscript is preserved).
En una cascara de Naranja àgria, quitando todo el àgrio, y parte dela cortesa de adentro se pondra en dicha naranja una cuchara de Manteca otra de aseite de comer, otra de aguardiente de castilla, un poquito de Canela de Castilla, bien molida y otro poco de azucema tres ò quatro botonsitos de mansanilla, se cosine al resco[l]do en fuego lento, tapadito con la mesma cascarita de naranja, y con esto suda al estomago, y aniquila la palpitacion, y por la mañana, tomando un poquito de agua de oregano, con naranja y raspadura como mate”.
(In a bitter orange peel, removing all the sour, and part of the inside rind, into said orange, a spoon of butter, another one of edible oil, another of Castillan moonshine, a little bit of well-ground Castillan cinnamon, and a little bit of tiger lily and three or four small chamomile buds are added; then, it is cooked on top of embers at low heat, covered with the same orange peel, and with this the stomach is rubbed, and it annihilates the palpitation, and in the morning, drinking a little oregano water, with orange and peel as a mate infusion.)
Results
This mid-18th century formulation was prescribed to reduce heart palpitations; in those days, medical texts on therapeutics that contributed to the development of medicine in the New Kingdom of Granada started circulating. The prescription thoroughly explains a treatment with a variety of herbal components, but the term palpitation is not defined or described, which might have generated confusion at the moment it was used. Medical advances of the time, based on herbal medicine, did not allow evidence-based scientific support; therefore, phytochemical components biological activity were recognized in an exclusively empirical and deductive way; nevertheless, these components had beneficial effects for health, provided that this treatment became a habit for a long period of time, without it being a cure for diseases, but a promoter of healthy lifestyle.
According to modern knowledge, at the beginning of the 21st century, palpitations have an important place among the most common symptoms as a chief complaint for general practitioners, cardiologists, or emergency departments, only preceded by chest pain3,4, and that are described as a sensation in the chest and/or neck-like pounding, movements, or jerks, occasionally associated by patients with a sense of “impending doom.” Palpitations have a wide range of underlying cardiac and non-cardiac pathologies, are more common in electrical disorders of the heart, generally last from some seconds to a couple of minutes and are produced by extra-systoles (atrial/ventricular), or have a clinical presentation of minutes, hours, or days if associated with sustained tachyarrhythmias (supraventricular/ventricular). For this reason, the patient usually attends the office asymptomatic, which makes it mandatory, for etiologic diagnosis, a thorough clinical evaluation, asking about the symptom, its form of onset, frequency, duration, irradiation of sensation, triggering, and associated factors, without forgetting to enquire for pathological, toxic, and family history5. The paraclinical studies employed are selected thanks to patient history and clinical expertise of the treating physician; an electrocardiogram must be included in the diagnostic ladder due to its easy accessibility and high performance as a diagnostic method. In selected patients, 24 h Holter monitor can be considered5,6.
The pathophysiological mechanisms of palpitations are unclear; their relationship with sensory receptors in the myocardium and pericardium, peripheral mechanoreceptors, and baroreceptors together with an activation of the sympathetic system by afferent pathways has been discovered. Given that palpitations can be caused by multiple conditions such as arrhythmias or heart structural alterations, psychosomatic disorders, systemic diseases such as anemia, consumption of medications, or psychoactive substances; the pathophysiology of these diseases varies between them, making an accurate pathophysiological explanation of this symptom even more difficult. It should be noted that physiological palpitations are perceived and associated by the patient in contexts such as intense physical activity or strong emotions, seen as a bodily response to a generally short-lived challenge5,6.
Palpitations are associated with a low mortality rate; however, the prognosis lies on patient underlying disease and associated comorbidities. The management of palpitations should target the underlying medical condition6.
Although the components of this colonial prescription are the result of knowledge and practices highly used by doctors in the 18th century, they lack current scientific evidence to support their therapeutic effects on the symptom or associated disease, evidence about safety, contraindications, and possible adverse effects in special populations such as the elderly, children, and pregnant women. With the passage of time, and thanks to scientific advances, a relationship was found between healthy eating, phytochemical agents such as those included in the described prescription, thus decreasing the physiological impact of various diseases7,8.
Physicochemical properties
A review of the phytochemical properties of each ingredient used in the colonial prescription is presented, explaining a possible mechanism of action and how this could be useful for palpitations direct or indirect management.
Orange peel (Citrus sinensis)
Antioxidant effect on flavonoids such as flavone glycosides, flavones, and flavonols found by thin-layer two-dimensional chromatography9.
Butter (margarine)
It is an important source of trans fatty acids, while butter is high in saturated fat. Consequently, it is used as an eventually flavoring agent with the other ingredients of the prescription, with no phytochemical properties that explain a benefit for palpitations.
Olive cooking oil (Olea europaea)
There has been evidence of a protective effect against inflammation in animal models due to different classes of hydrophilic phenols, hydroxytyrosol, and derivatives of oleuropein aglycon, dimethyl oleuropein, and ligstroside, present in the olive fruit. Among these protective effects, the reduction of phospholipid peroxidation in liposomes, protection of low-density lipoproteins against oxidation, reduction of oxidative damage in human erythrocytes, and change of peroxynitrite nitrogenated bases stand out, together with a reduction in the production of free radicals on the mitochondrial matrix10.
Castilla Cinnamon (Cinnamomum zeylanicum)
In vitro and in vivo evidence in animal models explains vasodilatory phytochemical properties by inhibiting extracellular calcium through type L voltage sensitive channels, which allows to position it as an natural antihypertensive agent; in addition, this ingredient appears to reduce blood glucose and serum cholesterol11.
Castilla moonshine
Alcohol at low doses has beneficial effects on blood pressure and acute-phase reactants such as C-reactive protein; simultaneously, it increases myocardial tolerance to ischemic injury, a mechanism known as “ischemic preconditioning”12.
Chamomile (Matricaria recutita)
Apigenin (5,7’4-trihydroxyflavone), a molecule isolated in this plant with high affinity for gamma-aminobutyric acid receptors, which binds competitively without activity on muscarinic and adrenergic (alpha 1) receptors, exerting an anxiolytic effect by reducing chlorine currents in a dose-dependent form, similar to benzodiazepines. In animal model studies, a benefit on blood pressure and lipid profile was also demonstrated13.
Madonna lily (Lilium lancifolium)
Traditional Chinese plant with effect on macrophages, which increases their phagocytic activity and pro-inflammatory cytokines phosphorylation, thus decreasing chemotaxis and thereby the immune response14.
After this brief description of the mechanisms of action of these herbal agents included in the prescription under study, it is possible beneficial effect on palpitations or underlying diseases can be postulated. However, the absence of evidence enough in human beings renders further investigation into this model to be necessary to determine its specific effect and therapeutic impact.
Discussion
In the 17th and 19th centuries, speaking about medicine was synonymous of empirical and scientific knowledge brought from Europe, which allowed a compilation of medical prescriptions by Spaniards and Native Americans that overtime would be increasingly used in the new continent. One of them, used the for management of palpitations, was composed of phytochemicals with antioxidant, anti-inflammatory, and anxiolytic properties, which were able to achieve, to a certain degree, control of palpitations, or some benefit in underlying diseases as a natural antihypertensive agent. However, vague information on parameters or conditions of its use and on the symptom description discredits its potential employment in those days for the control of palpitations or as a targeted phytochemical agent for diseases that cause said symptom. The work done by doctors or apothecaries, who were in charge of prescribing herbal medicine based on prescriptions, following patient evolution and achieving effectiveness in symptom relief stands out. This happened at a time in history when the church and the crown decided who should practice medicine, despite the fact that this was an act of courage due to the absence of public health and to the high biological risk, the doctor or apothecary was faced with by having a close relationship with the patient.
Conclusion
Until the 17th century, the humanity had reached a moderate development in understanding various aspects associated with most medical phenomena. From the second half of the 17th century and until the beginning of the 19th, several medical theories that would struggle for a place against Galen’s ideas, which had been in force for more than 1500 years, were developed. These theories gave rise to different concepts of disease and, consequently, to the modification of the therapeutics used until then. This entire movement took place under the influence which in that moment was determined by different currents of philosophical thought in the development of medical science of those times. This influence is reflected on the origin of the first medical practices that were initially based on two different ways of approaching the problem: the first one is primitive empiricism, characterized by pragmatism and by the use of medications and treatments obtained from nature, and the second one, medical vision influenced by the magical-religious current, which tried to explain disease from the point of view of mysticism and the beliefs institutionalized by the church.
Although in the Viceroyalty of New Granada, the knowledge of medicine was developed in a very similar way to the European, it was primarily marked by the encounter of three worlds, the indigenous, the Spanish, and the African world, which, starting from a conception of health-disease polarity, were similar in terms of their high cultural, social, moral, and emotional load, related to punishment, sin, degeneration, and vices, as a cause or reason for pathology.
This work seeks to contribute to the construction process of the history of national medicine, based on the analysis of documents that recreate, from different angles and pathologies, the medical approach of the moment, trying to find a comprehensive and documented explanation of local medical practice and knowledge predominating at that time in history.











 nueva página del texto (beta)
nueva página del texto (beta)