Introduction
Central blood pressure (CBP) has been established as a strong predictor of cardiovascular risk. European guidelines for systemic arterial hypertension recognize CBP as a useful tool in the evaluation of treatment, risk stratification, and detection of target organ damage1. Likewise, surrogate markers of CBP that translate vascular stiffness, aortic pulse wave velocity (PWVAo), and aortic augmentation index (Aix) have been associated with cardiovascular risk2.
However, the measurement of CBP is far from its use in daily clinical practice due to multiple factors including the lack of reference values between individuals of different races, gender, age, and body mass index (BMI).
The objective of this study was to evaluate the CBP, central pulse pressure (cPP), PWVAo, and Aix in a population of healthy Mexican subjects, to identify reference values, and to know their behavior according to gender, age, and BMI.
Methods
Design and population
Between 2015 and 2016, an observational cross-sectional study was conducted. The recruitment was done through open invitation to the people who were accompanying patients of the outpatient care department of our institution by convenience. These subjects were asked to fill out a survey and undergo an electrocardiogram to rule out any cardiovascular disease. Those with a history of hypertension, diabetes mellitus, smoking, alcoholism, ischemic heart disease, peripheral vascular disease, and electrocardiographic data of hypertensive heart disease were excluded from the study. A clinical questionnaire was applied and anthropometric measurements of weight in kilograms and height in meters were made to calculate the BMI. Subjects were classified according to their BMI values: underweight (< 18.5), normal (18.5-24.9), overweight (25-29.9), obesity Grade 1 (30-34.9), obesity Grade 2 (35-39.9), and obesity Grade 3 (≥ 40).
Measurement of CBP
An Arteriograph (TensioMed) device with oscillometric technique was used for its evaluation3; the CBP measurements of the subjects were carried out between 9:00 a.m. and 11:00 a.m., on a single occasion, all records were obtained in a quiet environment, after resting in supine position for 5 min and later analyzed with software (version 3.0.0.4.), which reported CBP, cPP, systolic brachial pressure (SBP), brachial pulse pressure (bPP), PWVAo, and Aix.
Statistical analysis
The numerical variables are summarized as mean and standard deviation or median and quartiles 25 and 75, according to their distribution. The categorical variables are summarized in frequency and percentage. We performed bivaried analysis of two independent groups with t-test or MannWhitney U-test for numerical variables and Chi-square test for categorical variables. When there are more than two groups to be compared, the ANOVA, KruskalWallis, and Chi-square linear trend tests were used, depending on the case. Bivaried correlations were performed (Pearson or Spearman, according to distribution). Multivariate analysis was performed with logistic regression to predict CBP > 140 mmHg, PWVAo > 9 m/s, and Aix > 33% using the Statistical Package for the Social Sciences 22.0, a two-tailed p < 0.05 was considered statistically significant.
Results
We included 1009 participants, 72% were female, average age of 47 ± 12 years (minimum of 15, maximum of 89 years), 7% with active smoking, 26% with normal weight (BMI in the whole population: 28 ± 4.6 kg/m2), 43% overweight, 22% obesity Grade 1, 6% obesity Grade 2, and 2% obesity Grade 3.
Analysis by sex
Table 1 shows the results divided by sex. There were no differences in age, BMI, or brachial systolic blood pressure. However, women had higher levels of CBP and cPP, with higher proportions with CBP above the expected limit, without statistical significance (> 140 mmHg, 29% vs. 23%, p = 0.056). At the same time, women had significantly higher values of PWVAo and Aix. Similarly, the calculated arterial age was higher for women, despite similar chronological ages. When taking the CBP cutoff points ≥ 140 mmHg and cPP ≥ 50 mmHg for the diagnosis of high blood pressure, a higher proportion of new diagnoses was observed in women, without observing important changes in men or when using brachial measurements (Fig. 1).
Table 1 Central blood pressure and arterial stiffness parameter by sex
| Parameter | Total (n = 1009) | Female (n = 727) | Male (n = 282) | p-value |
|---|---|---|---|---|
| Age in years | 47 ± 12 | 48 ± 12 | 46 ± 13 | NS |
| BMI (kg/m2) | 27 (24-30) | 27 (24-31) | 27 (24-30) | NS |
| SBP (mmHg) | 126 (117-139) | 126 (117-141) | 129 (119-139) | NS |
| bPP (mmHg) | 53 ± 10 | 54 ± 11 | 52 ± 9 | 0.001 |
| CBP (mmHg) | 126 (113-141) | 127 (113-143) | 124 (111-138) | 0.03 |
| cPP (mmHg) | 53 ± 14 | 54 ± 14 | 47 ± 12 | < 0.001 |
| PWVAo (m/s) | 7.8 (6.9-9.3) | 7.9 (7-9.7) | 7.6 (6.8-8.5) | < 0.001 |
| Aix (%) | 33 ± 13 | 36 ± 13 | 27 ± 13 | < 0.001 |
| Arterial age | 40 ± 16 | 41 ± 16 | 38 ± 15 | 0.001 |
BMI: body mass index; SBP: systolic brachial blood pressure; bPP: brachial pulse pressure; CBP: central blood pressure; cPP: central pulse pressure; PWVAo: aortic pulse wave velocity; Aix: augmentation index. Variables are summarized as mean and standard deviation or median and quartiles 25 and 75, according to their distribution.
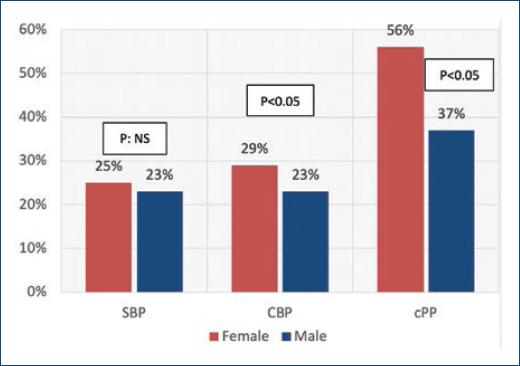
Figure 1 New diagnoses of high blood pressure. Red bar represents female. Blue bars represent male. With SBP, similar proportion of new high blood pressure diagnosis was made. With CBP, a higher proportion of high blood pressure new diagnosis in female was observed. The proportion is higher with cPP. SBP: systolic brachial blood pressure; CBP: central blood pressure; cPP: central pulse pressure.
Analysis by age
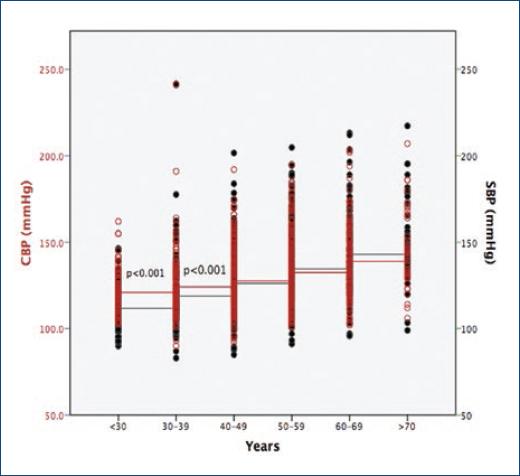
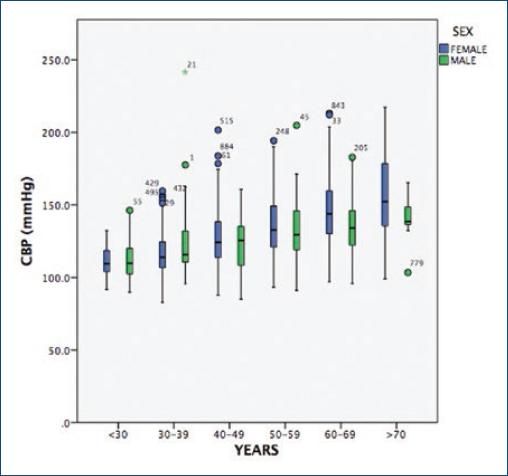
Table 2 shows the measurements obtained by age group. We observed a moderate direct association between age and SBP (rho = 0.34, p < 0.001), which improves for CBP (r = 0.47, p < 0.0001) and cPP (r = 0.49, p < 0.0001). Two other phenomena were observed: the first, in subjects younger than 40 years, a significant gradient between SBP and CBP is observed, after this age, the pressures are similar (Fig. 2). Second, women under 40 years have lower values of CBP; however, when this age is exceeded, CBP exceeds men (Fig. 3). Regarding the parameters of vascular rigidity, both have moderate direct association with age (r = 0.52, p < 0.001 for PWVAo and r = 0.57, p < 0.001 for Aix). Regardless of age, women have higher Aix values.
Table 2 Central blood pressure and arterial stiffness parameter by age
| Parameter | < 30a (n = 95) | 30-39a (n = 156) | 40-49a (n = 286) | 50-59a (n = 285) | 60-69a (n = 150) | > 70a (n = 37) | p-value |
|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | 24 (25-28) | 27 (25-31) | 27 (25-31) | 27 (25-31) | 27 (24-30) | 27 (26-29) | < 0.001 |
| SBP (mmHg) | 120 (112-126) | 121 (115-130) | 124 (117-137) | 129 (120-144) | 138 (124-152) | 142 (130-165) | < 0.001 |
| bPP (mmHg) | 52 (45-59) | 49 (44-56) | 51 (44-57) | 52 (46-59) | 58 (50-56) | 63 (52-74) | < 0.001 |
| CBP (mmHg) | 109 (103-118) | 114 (107-128) | 124 (113-137) | 131 (120-149) | 140 (127-156) | 145 (135-168) | < 0.001 |
| cPP (mmHg) | 42 (38-45) | 43 (38-50) | 48 (42-58) | 54 (45-63) | 63 (52-71) | 69 (57-79) | < 0.001 |
| PWVAo (m/s) | 6.3 (6-6.9) | 7.1 (6.4-7.6) | 7.6 (7-8.3) | 8.4 (7.5-10) | 9.7 (8.3-11) | 10.5 (8.7-11) | < 0.001 |
| Aix (%) | 18 (11-24) | 24 (15-32) | 31 (23-39) | 39 (31-46) | 44 (35-52) | 47 (37-53) | < 0.001 |
| Arterial age | 18 (15-27) | 31 (18-38) | 38 (30-46) | 47 (38-60) | 60 (46-60) | 60 (51-60) | < 0.001 |
BMI: body mass index; SBP: systolic brachial blood pressure; bPP: brachial pulse pressure; CBP: central blood pressure; cPP: central pulse pressure; PWVAo: aortic pulse wave velocity; Aix: augmentation index. Variables are summarized as median and quartiles 25 and 75, according to their distribution.
BMI analysis
Table 3 shows the measurements by weight category. Weak direct associations were observed between BMI, SBP (rho = 0.24, p < 0.001), and CBP (rho = 0.19, p < 0.001); however, the values of these last two increase to a greater degree of obesity in a significant way. When analyzing vascular rigidity parameters, no association with BMI is observed.
Table 3 Central blood pressure and arterial stiffness parameter by BMI
| Parameter | Normal (n = 264) | Overweight (n = 441) | Obesity Grade 1 (n = 228) | Obesity Grade 2 (n = 57) | Obesity Grade 3 (n = 19) | p-value |
|---|---|---|---|---|---|---|
| Age by years | 46 (33-57) | 49 (41-57) | 49 (40-57) | 48 (42-55) | 48 (43-56) | 0.003 |
| SBP (mmHg) | 124 (114-133) | 125 (117-138) | 130 (12-144) | 143 (124-154) | 143 (129-159) | < 0.001 |
| bPP (mmHg) | 51 (44-57) | 51 (45-58) | 54 (48-61) | 60 (53-65) | 60 (52-73) | < 0.001 |
| CBP (mmHg) | 121 (109-136) | 125 (112-141) | 128 (115-145) | 142 (124-155) | 139 (132-162) | < 0.001 |
| cPP (mmHg) | 48 (41-60) | 49 (42-60) | 51 (43-63) | 59 (51-69) | 59 (50-69) | < 0.001 |
| PWVAo (m/s) | 7.7 (6.7-9.4) | 7.8 (6.9-9.4) | 7.9 (7-9.2) | 8 (7.2-9.5) | 8.2 (7.5-9.2) | 0.42 |
| Aix (%) | 33 ± 14 | 33 ± 13 | 32 ± 13 | 34 ± 12 | 35 ± 13 | 0.79 |
| Arterial age | 39 (24-60) | 41 (29-60) | 42 (30-60) | 43 (33-60) | 45 (37-60) | 0.27 |
BMI: body mass index; SBP: systolic brachial blood pressure; bPP: brachial pulse pressure; CBP: central blood pressure; cPP: central pulse pressure; PWVAo: aortic pulse wave velocity; Aix: augmentation index. Variables are summarized as mean and standard deviation or median and quartiles 25 and 75, according to their distribution.
Logistic regressions
Table 4 shows logistic regressions. Independent predictors for CBP > 140 mmHg are age and BMI and for PWVAo > 9 m/s and Aix > 33% are age and sex, without showing effect by the BMI on these parameters related to vascular stiffness.
Table 4 Logistic regressions
| Parameter | OR (CI 95%) | p-value |
|---|---|---|
| To predicts CBP > 140 mmHg | ||
| Age by years | 1.08 (1.06, 1.1) | < 0.0001 |
| BMI (K/m2) | 1.09 (1.05, 1.13) | 0.001 |
| Male sex | 0.8 (0.5, 1.1) | NS |
| To predicts PWVAo > 9 m/s | ||
| Age by years | 1.12 (1.1, 1.14) | < 0.0001 |
| BMI (k/m2) | 1 (0.9, 1.03) | NS |
| Male sex | 0.36 (0.24, 0.54) | < 0.0001 |
| To predicts Aix > 33% | ||
| Age by years | 1.11 (1.09, 1.13) | < 0.0001 |
| BMI (k/m2) | 0.97 (0.94, 1) | NS |
| Male sex | 0.25 (0.18, 0.36) | < 0.0001 |
BMI: body mass index; CBP: central blood pressure; PWVAo: aortic pulse wave velocity; Aix: augmentation index.
Discussion
Central aortic pressure has been established as a reliable measure for the stratification of prognosis and cardiovascular risk. Its elevation has been correlated with the thickness of the intima-media of the carotids4, increase and regression of left ventricular mass in hypertensive patients5, and with a better ability to predict cardiovascular events compared to brachial blood pressure2. Similarly, the cPP ≥ 50 mmHg is associated with morbi-mortality1.
However, the measurement of CBP in daily clinical practice is far from being a reality, for a variety of reasons. Among them, the multitude of equipment available for measurement, the lack of normal reference values for particular populations (such as Hispanics) and of reference tables in patients according to age, sex and body weight6.
In addition, the evidence regarding CBP in relation to cardiovascular risk is not conclusive since it mostly comes from subanalysis, with sometimes contradictory results. Therefore, although it shows a promising role in the non-invasive stratification of risk, CBP has not succeeded in replacing brachial measurements in the diagnosis, follow-up, and prognosis of patients with systemic arterial hypertension.
The present study tries to solve, in part, the problem described above, delimiting the normal values of reference in healthy Hispanic population (which in itself presents a higher cardiovascular risk than other races) and with the use of equipment widely validated in the previous studies, with the objective of establishing a base in the area of research on central aortic pressure in Mexican population.
CBP and gender
Regarding the relationship between CBP and sex, a statistically significant difference was observed between men and women, however, with a delta of only 3 mmHg. Studies with a large number of patients in China and Europe showed similar results7,8. It is noteworthy that, after 40 years of age, the CBP is equal and even, when over 60 years old, the gradient is reversed and becomes greater for women than men.
Notably, the use of CBP and its measurements increased the proportion of women with a new diagnosis of hypertension, but not with the use of SBP. According to data from ENSANUT 2016, the prevalence in Mexico of hypertension is 25.5%, and 40% do not know its diagnosis9. The greater proportion of new diagnoses in women is due to the effect of the use of CBP, despite the fact that SBP values were similar.
When comparing the reference values of our population with European and Asian results, higher values were found7,8. These results are relevant because they may be associated with a higher baseline cardiovascular risk in Hispanics, according to previously reported10.
Regarding the cPP and Aix, women presented higher statistically significant values, however, directly influenced by the height, a finding already described previously11. However, the PWVAo (which is not modified by the height) is elevated in women, probably in relation to greater vascular rigidity. Although our results cannot be conclusive in this regard, we believe that they support the hypothesis that women may present different risk and pathophysiology, so they may also need special considerations in treatment.
CBP and age
The increase in age leads to an increase in CBP and vascular rigidity parameters. This association has been reproduced by various publications7,8,12, which is reflected in the higher prevalence of hypertension as the age advances13.
Of relevance, a statistically significant gradient of central-brachial pressure was observed in patients under 40 years of age. After this age, the significance is lost and both pressures present similar measurements. Our results show CBP values of 109 (103-118) and 114 (107-128) mmHg in < 30 and 30-40 years, respectively, and a central-brachial gradient of 11 and 7 mmHg was observed and may consider normal.
The significance of the loss of this gradient or the presence of higher CBP values in this age group and its relationship with an increased risk of arterial hypertension remains to be clarified. Saladini et al.14 recruited 305 patients with an age of 37 ± 10 years and performed measurements of SBP and CBP, finding this central-brachial gradient; at follow-up, subjects with a lower gradient had a higher incidence of high blood pressure. Therefore, the measurement of CBP could have a potential impact on the early diagnosis of high blood pressure in subjects less than 40 years.
CBP and BMI
Regarding the BMI, it was found that the greater the degree of obesity, there is an increase in the CBP and the brachial measurements, data observed in previous publications15,16. However, the parameters of vascular rigidity did not show differences between the degrees of obesity. Other authors have reported this finding15-17, suggesting that different physiopathological mechanisms are present in the patient with obesity. Messerli et al.18 conducted a study to assess the hemodynamic differences associated with hypertension and obesity, reporting that the total blood volume is significantly increased in obese hypertensive patients and found no differences in peripheral resistance or plasma renin activity. The same author later published that obese subjects had lower values of circulating catecholamines when compared with subjects of normal weight19. These data suggest that, at least partially, a cause of arterial hypertension in obese patients is the increase in blood volume and not an effect of vascular rigidity or catecholamines so that treatments should possibly be aimed at this objective.
Conclusion
We observe significant differences in CBP, cPP, PWVAo, and Aix based on age, gender, and BMI. In a Mexican population, higher values of CBP and cPP were found in female, the elderly, and obese, with a central-brachial gradient in younger than 40 years. PWVAo and Aix are high in women and the elderly; however, they are not modified by BMI.
Limitations
The main limitations of our study are the sample size, although, to our current knowledge, it could be the largest Hispanic population included in this issue. On the other hand, the lack of follow-up and hard outcomes makes it difficult to relate our findings to risk, so additional studies are needed to clarify the role of CBP and the parameters of vascular rigidity in the stratification and diagnosis of hypertension in Hispanics. Our study included a greater proportion of female sex because socially in our environment is this gender the natural companion of patients to their medical consultations; this could have an impact on the generalization of the results, mainly in the differences by gender.











 nueva página del texto (beta)
nueva página del texto (beta)