Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Archivos de neurociencias (México, D.F.)
versión On-line ISSN 1028-5938versión impresa ISSN 0187-4705
Arch. Neurocien. (Mex., D.F.) vol.10 no.1 Ciudad de México ene./mar. 2005
Reporte de caso
Accessory middle cerebral artery associated with two intracranial aneurysms
Cerebral media accesoria asociada a dos aneurismas
Román Garza–Mercado, Dagoberto Tamez–Montes, Angel Martfnez–Ponce de León,
Victor Daniel Morales–García
Department of Neurosurgery and Neurological Endovascular Therapy (NET), Nuevo León State Autonomous University School of Medicine and University Hospital "Dr. José Eleuterio González", Monterrey, NL, México
Correspondencia:
Román Garza–Mercado,
Hospital Universitario "J. Eleuterio González", Ave. Madero al Poniente,
64460, Monterrey, NL, México.
E–mail: garzamercado@hotmail.com
Recibido: 16 noviembre 2004
Aceptado: 30 noviembre 2004
RESUMEN
Objetivo e importancia: aunque ya publicado, la duplicación de la arteria cerebral media (ACM) es un hallazgo angiográfico reconocido infrecuentemente. En este reporte, la anomalía fue asociada con dos aneurismas, uno roto.
Presentación clínica: una ACM anómala, tipo gemela, que nace a partir de la arteria cerebral anterior izquierda dominante en segmento precomunicante extendiéndose hacia la fisura silviana, en estrecho paralelismo con el segmento esfenoidal de la ACM, fue identificada angiográficamente como una ACM accesoria. La paciente fue una mujer de 74 años investigada por un episodio reciente de hemorragia subaracnoidea. Se demostraron dos aneurismas intracraneales: uno originado en la arteria comunicante anterior y el otro en la unión del segmento M1–M2 derecho.
Intervención: fue rechazado el tratamiento quirúrgico o endovascular, pero la paciente permaneció hospitalizada. Dos semanas después del internamiento, ocurrió un deterioro neurológico súbito asociado a hidrocefalia aguda, tratada con derivación ventricular al exterior de urgencia. Desafortunadamente, la paciente no mejoró, falleciendo como resultado de una neumonía nosocomial. No se otorgó el consentimiento de autopsia.
Conclusión: se reporta un ejemplo de ACM accesoria, en este caso asociado con dos aneurismas arteriales intracraneales, uno roto. Se hace una breve discusión de la literatura médica.
Palabra clave: ACM accesoria, aneurisma intracraneal, anomalías ACM, aneurismas intracraneales múltiples.
ABSTRACT
Objective and importance: albeit very likely underdisclosed, duplication of the middle cerebral artery (MCA) is a rather unfrequently recognized angiographic finding. In this instance the anomaly was associated with two intracranial aneurysms, one ruptured.
Clinical presentation: an anomalous, twinlike MCA, departing from a dominant left precommunicating anterior cerebral artery and extending recurrently toward the sylvian fissure, in close parallelism with the sphenoidal MCA segment, was angiographically identified as an accessory MCA. The patient was a 74 year old woman being investigated for recent spontaneous subarachnoid hemorrhage. In addition, two intracranial arterial aneurysms were also demonstrated: one originated from the left corner of the anterior communicating artery; the other expanded at the right M1–M2 junction.
Intervention: the proposed surgical or endovascular treatment was refused but the patient remained hospitalized. Sudden neurological deterioration occurred two weeks after hospitalization due to acute hydrocephalus so that an external ventricular drainage system was expeditiously applied. Regretfully, the patient did not improve and expired thereof as result of nosocomial pneumonia. Necropsy request was not granted.
Conclusion: we hereby report a new example of accessory MCA, in this case associated with two intracranial arterial aneurysms, one ruptured. A brief discussion of the pertinent medical literature is made.
Key words: accessory MCA, intracranial aneurysm, MCA anomalies, multiple intracranial aneurysms.
A list of all anatomical vascular variants of the brain should likely begin with the arterial circle extended at the base of the brain, for a balanced arrangement of its components and proximal branches, a socalled "normal" or "symmetrical" circle of Willis, is observed in not quite 50% of cases1. In spite of being the most complex, and have the largest distribution of all intracranial arteries, anomalies of the middle cerebral artery (MCA) are, perhaps paradoxically, less frequently recognized, or reported, than those in other major cerebral vessels. Perusal of the literature reveals several instances of MCA duplication, the anomalous channel departing either from the internal carotid artery (ICA) or the anterior cerebral artery (ACA), as well as some examples of proximal MCA fenestration.
This paper emphasizes the persistence of an accessory MCA demonstrated by means of cerebral angiography in an elderly lady who suffered an episode of subarachnoid hemorrhage (SAH), due to the rupture of one of two associated inatracranial aneurysms.
CASE REPORT
A 74 year old, right–handed woman, with an eight–year history of untreated arterial hypertension, was hospitalized in our Service on november 19,2002. Three days earlier, intense suboccipital headache of sudden onset occurred, followed by transient (30 minutes) loss of consciousness and lefthemiparesis. The patientwas taken initially to another local hospital where a computerized tomography (CT) scan, which turned out to be abnormal, was obtained. Hence, she was transferred to the University Hospital for further evaluation and treatment.
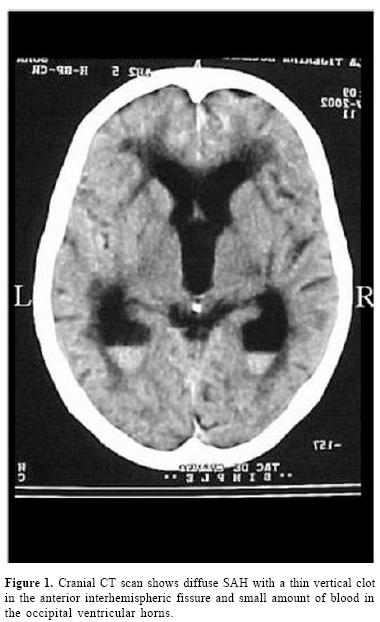
Upon admission, her blood pressure was 160/ 90 and the rest of the physiological constants, were normal. The patientwas disoriented but could attend verbal commands and move freely, if not with her left side. There was moderate neck stiffness, mild left hemiparesis and bilateral extensor plantar response. The pupils were symmetrical and reactive and the fundoscopic examination revealed slight hypertensive arteriolar changes but no subhyloid hemorrhages. A noncontrasted cranial CT scan that relatives carried along (figure 1) showed diffuse SAH, a thin linear clot in the frontal interhemispheric fissure and small amount of intraventricular blood at the bottom of both occipital horns. The ventricular system was slightly enlarged due patient's age.
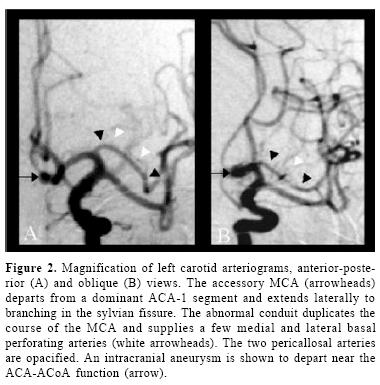
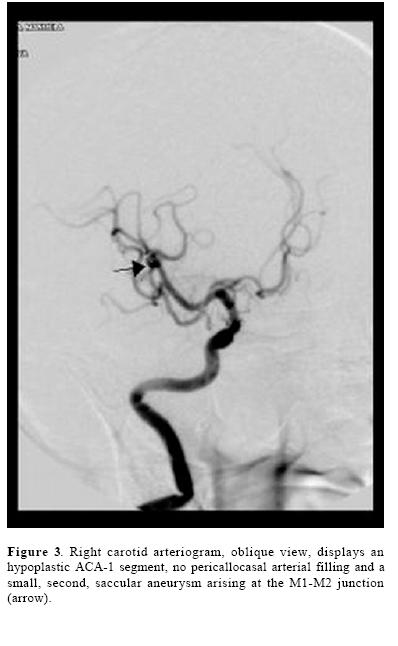
Transfemoral cerebral panangiography was carried out under light sedation the following day. Left ICA injection (figure 2) revealed dominance of ACA–1 with opacification of both pericallosal arteries and a saccular aneurysm arising from the left corner of the anterior communicating artery (ACoA), which was recognized as the SAH's culprit. In addition, an anomalous arterial channel, roughly paralleling the course of the left MCA, was clearly observed in the anterior–posterior and oblique views. As this second, "twin" like MCA departed from the proximal portion of ACA, extended laterally in the sylvian fissure to arborisation, supplying pari–passus thin basal perforating branches, it was readily categorized as an accessory MCA. The right ICA injection (figure 3) demonstrated an hypoplastic A1 segment, 1 no pericallosal filling and asecondaneurysm, emerging at the M1–M2 junction. The proposed micro–neurosurgical or endovascular treatment was refused.
The patient, however, remained hospitalized.
Sudden deterioration occurred two weeks later, the Glasgow coma scale grading declining to 7. After immediate endotracheal intubation and stabilization in the Intensive Care Unit, repeat CT scan of the head disclosed acute hydrocephalus with no trace of recurrent SAH. Actually, the subarachnoid and intraventricular blood observed in the previous CT scan, had vanished. A system for continuous external ventricular drainage was inserted. Regretfully, the patient expired on december 17, 2002, due to nosocomial pneumonia with no neurological improvement. Autopsy request was not granted.
DISCUSSION
An abnormal arterial conduit running back from ACA into the sylvian fissure to replace the orbital branch of the MCA, was observed in a posmortem investigation by Blackburn, as early as 19082. The nomination, however, of such irregular recurrent arterial conduits as accessory MCA, took place in 1962, by Crompton3, following the examination of 347 cadaveric brains. In his investigation, 11 examples of double MCA were found, an incidence of 3.2%. The circumstance that 10 of the anomalous arteries departed from ICA and one from ACA did not preclude him from characterizing them all with the same name, attending more to its course than to its different arterial origin. Two years later, Jain4 published 10 examples of, again, accessory MCA, discovered among 300 postmortem sylvian arteries dissected, a rate of 3.3%. But at this time, eight of the variants sprang from ACA, and only two from ICA. Finally, in 1973, Teal et al.5, in reporting five additional angiographic examples of double MCA, clarified the confusion by restricting the designation of accessory MCA to the anomalous channel departing from ACA, and to term the one deriving from ICA as duplicate MCA.
Hence, by universal acceptance, all accessory MCAs arise from ACA, most often from ACA–11,4,6,8, but they will at times depart from ACA–26,9,10 or ACoA10,11. The duplicate MCA, in turn, will develop directly from ICA, either at the level of the anterior choroidal artery (AChA)6, between AChA and ICA end7,10, or opposite the origin of ACA, as an early ICA bifurcation1. As rather unique necropsy findings, an accessory MCA and a duplicate MCA, both, concurred in one occasion in the same cerebral hemisphere6; in one other, the accessory MCA presented bilaterally4, and in a third instance, an ICA–originated repeat MCA, was associated with reduplication of the circle of Willis12. A bilateral accessory MCA has been diagnosed also in a few patients by means of cerebral arteriography11,13.
More recent posfmortem microanatomical studies of the sylvian arteries upon unfixed adult brains16 have validated MCA duplication at a rate of 2.9% to 4.0%. In 1968, Handa et al.13 and Krayenbhül and Yasargil14 first showed such MCA anomalies by in–vivo cerebral arteriography. The reported angiographical incidence of accessory and duplicate MCAs combinedly ranges from 0.32%8 and 1.6% 7, to as high as 4.6% 15 but some of these anomalies will pass clinically unrecognized or unpublished16. Proximal fenestration (short, partial duplication) is a third MCA anomaly disclosed at autopsy1,3,6,11 or observed in cerebral angiograms at a rate of 0.26%1.
MCA abnormalities like these have been described as fortuitous angiographic findings in the investigation of patients suffering from head injury or ischemic stroke7, 8,16, craniopharyngioma or paraganglioma7, moyamoya disease10,17 or cerebral arteriovenous malformation18. Yet, their most frequent associations are intracranial aneurysms, usually single1,3,9,14,19,20, at times originating from the abnormal arterial conduit itself3,15,21. In a series of 24 patients with SAH and MCA variants drawn from the literature by Umanski et al.1 there were 35 associated intracranial aneurysms diagnosed. In five occasions, an aneurysm arose at the site of the anomaly (20.8%) and in five patients, the aneurysms were multiple (three patients with two, one with four, and one with six aneurysms). Our patient had two aneurysms. Nevertheless, a proclivity for aneurysmal development greater in these patients than in the general population, there seems not to be1.
The embryological significance of the MCA irregularities is not completely dilucidated as to whether they are the result of early blood flow dynamics or represent a persistent fetal vascular supply. Marubayashi18 suggests the accessory MCA is a residual congenital artery and the duplicate MCA represents an early ICA bifurcation. Handa et al19. See the accessory MCA as an hypertrophic recurrent Heubner artery (RHA) for it originates from ACA and supplies basal perforating branches. Yet, the accessory MCA and the RHA may coexist, usually with independent departure. Takahashi et al.22 consider both, the accessory MCA and the RHA, resulting from a primitive anastomotic vascular network supplying the pyriform cortex, with final predominance of one or the other, usually the latter. Furtheremore, Komiyama et al.7 believe the duplicating MCA is a precocious ramification of early MCA branching while Yasargil and Smith10 prefer not to derive any definitive conclusions in this regard.
In any case, their existence in the brain, in particular the accessory MCA, may serve as significant alternative channels for collateral blood supply reducing a potentially devastating neurological deficit in cases of acute or chronic, embolic or surgical ICA and/ or MCA occlusion16,17,20. In this eventuality, not rarely, the accessory MCA will be demonstrated to fill angiographically from the opposite ICA, across the midline. The preoperatory definition of this type of abnormalities will help the microvascular or endovascular surgeon toward the best treatment of intracranial aneurysms and occlusive cerebral disease.
CONCLUSION
One additional angiographic example of an accessory MCA, in this case associated with two supratentorial intracranial aneurysms, is presented. The anomalous MCA in our patient departed from ACA and extended laterally in a recurrent fashion paralleling the course of MCA, providing a few basal perforating arteries before branching.
REFERENCES
1. Umanski F, Dujovny M, Ausman Jl, Diaz FG, Mirchandani HG. Anomalies and variations of the middle cerebral artery: a microanatomical study. Neurosurgery 1998; 22:1023–7. [ Links ]
2. Blackburn IW. Anomalies of the encephalic arteries among the insane: A study of the arteries at the base of the encephalon in two hundred and twenty consecutive cases of mental disease, with special reference to anomalies of the circle of Willis. J Comp Neurol Psychol 1908; 17:493–517. [ Links ]
3. Crompton MR. The pathology of ruptured middle–cerebral aneurysms with special reference to the differences between the sexes. Lancet 1962; 2:421–5. [ Links ]
4. Jain KK. Some observations on the anatomy of the middle cerebral artery. Can J Surg 1964; 7:134–9. [ Links ]
5. Teal JS, Rumbaugh CL, Bergeron RT, Segall HD. Anomalies of the middle cerebral artery: accessory artery, duplication and early bifurcation. Am J Roentgenol Radium Therapy Nucl Med 1973; 118:567–75. [ Links ]
6. Gibo H, Carver CC, Rhoton AL, Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg 1981:54:151–69. [ Links ]
7. Komiyama M, Nakajima H, Nishikawa M, Yasui T. Middle cerebral artery variations: duplicated and accessory arteries. AJNR 1998:19:45–9. [ Links ]
8. Watanabe T, Togo M. Accessory middle cerebral artery. J Neurosurg 1974:41:248–51. [ Links ]
9. Tacconi L, Johnston FG, Symon L. Accessory middle cerebral artery. Case report. J Neurosurg 1995:83:916–8. [ Links ]
10. Yasargil GM, Smith RD. Association of middle cerebral artery anomalies with saccular aneurysms and moyamoya disease. Surg Neurol 1976; 6:39–43. [ Links ]
11.Yasargil MG. Middle cerebral artery, in Microneurosurgery. Stuttgart, Georg Thieme Verlag 1984, vol I, 86–91. [ Links ]
12. Fisher ER, Davis JS, Lemmen MJ. Anomalous reduplication of the circle of Willis. J Neurosurg 1959; 6:331–6. [ Links ]
13. Handa J, Seta K, Handa H. Die akzessorische A cerebri media. Fortschr Roentgenstr 1968; 108:539–41. [ Links ]
14. Krayenbühl HA, Yasargil MG. Cerebral Angiography, ed 2. London, Butterworth 1968. [ Links ]
15. Miyazaki S, Ito K, Ishii S. Aneurysm at the origin of the accessory middle cerebral artery. Surg Neurol 1984; 22:292–4. [ Links ]
16. Komiyama M, Nishikawa M, Yasui T. The accessory middle cerebral artery as a collateral blood supply. AJNR 1997;18:587–90. [ Links ]
17. Komiyama M, Yasui T. Accessory middle cerebral artery and moyamoya disease. J Neurol Neurosurg Psychiatry 2001; 71:129–30 (letter). [ Links ]
18. Marubayashi T. Accessory middle cerebral artery and duplication of middle cerebral artery–terminology, incidence, vascular etiology and developmental significance. Neurología Medico Chirurgica 1992; 32:262–7. [ Links ]
19. Handa J, Shimizu Y, Matsuda M, Handa H. The accessory middle cerebral artery: Report of further two cases. Clin Radiol 1970;21:415–6. [ Links ]
20. Mueller DP, Sato Y, Yuh WTC. Accessory middle cerebral artery as a source of collateral blood flow. AJNR 1991; 12:1223–4. [ Links ]
21.Waga S, Kojima T, Morooka Y, Sakakura M. Aneurysm of the accessory middle cerebral artery. Surg Neurol 1977; 8:359–60. [ Links ]
22. Takahashi S, Hoshino F, Uemura K, Takahashi A, Sakamoto K. Accessory middle cerebral artery: is it a variant form of the recurrent artery of Heubner? AJNR 1989; 10:563–8 (abstr). [ Links ]














